Information obtained under HIPAA Privacy Rule
1.August 6, 2014 to Langan with health materials 2. Quest-Clinical

The elements of a criminal offense under HIPAA are fairly straightforward. To commit a “criminal offense” under HIPAA, a person must knowingly and in violation of the HIPAA rules do one (or more) of the following three things.: use or cause to be used a unique health identifier, obtain individually identifiable health information relating to an individual or disclose individually identifiable health information to another person. Criminal penalties under HIPAA, tiered in accordance with the seriousness of the offense, range from a fine of up to $50,000 and/or imprisonment up to a year for a simple violation to a fine up to $100,000 and/or imprisonment up to five years for an offense committed under a false pretense and a fine up to $250000 and/or imprisonment up to ten years for an offense committed with intent to sell, transfer, or use individually identifiable health information for commercial advantage , personal gain, or malicious harm.
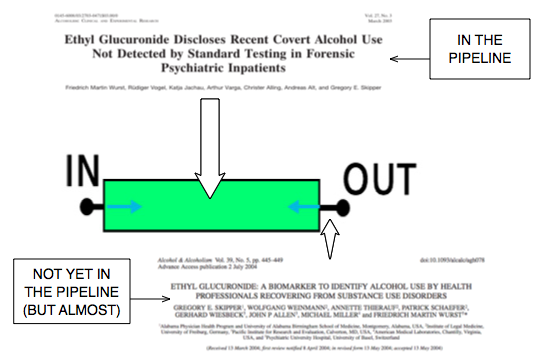
One of the ways physician health programs are engaging in forensic fraud using laboratory developed tests (LDTs) is by changing them from “forensic” to “clinical” samples in order to bypass chain-of-custody. As there is no regulation or oversight of the entire testing process it is easy to do. PHPs have no oversight or regulation. Neither do the commercial drug testing labs using these tests. They are non-FDA approved and CLIA exempt so the only avenue of complaint is the College of American Pathologists (CAP) which is an accreditation agency that does not have the power to sanction.

In terms of criminal penalties I would aim for the $25000 and 10 year mark as the cumulative documentation of HIPAA breaches committed by PHS, Quest and USDTL under false pretense are many and severe.
The Department of Health and Human Services Office for Civil Rights confirmed that my blood test from July 1, 2011 was intentionally changed to a clinical specimen and sent to USDTL with specific instructions to process it as a clinical specimen. Under the updated HIPAA-Privacy Rule “patients’ have the right to request their records directly from labs without authorization of the ordering provider.
It is important to recognize that all three parties had misrepresented this test as “forensic” since 2011. I have been requesting the “external chain-of-custody” from Quest since December of 2011 and the “appended test” from V.P. of Laboratory Operations Joseph Jones since December of 2012 when I was informed that it was changed from positive to invalid on October 4, 2012.
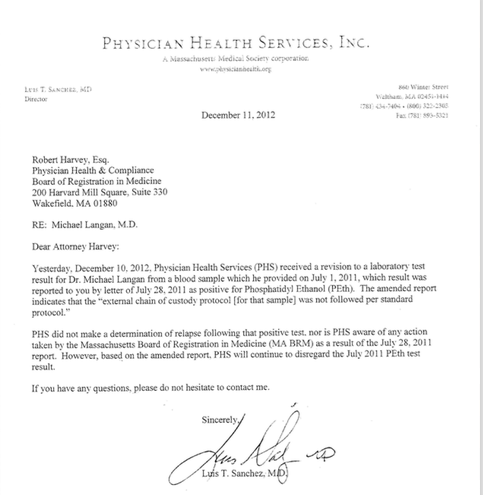
The new documents provided by USDTL include the October 4, 2012 revised test contradicting Dr. Luis Sanchez letter that he “just found out about” the revised test 67-days later.
The importance of this cannot be overstated as I filed a complaint with the College of American Pathologists in January of 2012. The investigation confirmed my suspicion that the test was fraudulent and as a result CAP mandated that USDTL revise the test.

USDTL did so and reported it to Dr. Sanchez but both concealed it and Sanchez took action against my license the following week.
“Moving the Goalpost” is a frequent tactic of PHPs whereby they make a new allegation and disregard the original. By controlling the information that is provided they are able to suppress and conceal whatever they want by misusing existing health care confidentiality law.
The October 19, 2012 report for noncompliance with my contract was done under “color of law” and resulted in suspension of my medical license. The new documentation shows that all three parties were involved in the fraud and the coverup.
The information USDTL provided even contains an email from me to Joseph Jones from December of 2012 requesting that he provide a copy of the October 4, 2012 revision which he ignored.
In response to demand letters from my attorney all three defended themselves by claiming the July 1, 2011 test had absolutely nothing to do with my suspension and blamed it on my non-compliance. The new documentation shows that I was reported for noncompliance after Dr. Sanchez was made aware of the revised test.
As the three parties colluded to produce PHI and used it with malice in a conspiracy to commit fraud and I am therefore requesting that charges be filed against these parties under the HIPAA criminal statute:
The HIPAA criminal statute, 42 U.S.C.A. § 1320d-6, reads in pertinent part:
”A person who knowingly and in violation of this part—
• uses or causes to be used a unique health identifier;
• obtains individually identifiable health information relating to an individual; or
discloses individual identifiable health information to another person, shall be punished as provided in subsection (b) of this section.”
”Whoever willfully causes an act to be done which if directly performed by him or another would be an offense against the United States, is punishable as a principal.” 18 U.S.C. § 2(b).
All three parties knew this was intentionally changed from a forensic to a clinical sample and PHI. Instead of correcting an error both Quest and USDTL took steps to conceal this information. In fact, the complicity of the three parties, cover-up and extent of damages caused by it make this the worst HIPAA-criminal violation to date. I can find nothing comparable and the damages have still not been corrected.
Luis Sanchez was notified of the invalidity of the test on October 4, 2012 but suppressed it for 67-days. This was a result of my complaint to the College of American Pathologists (CAP) that launched an investigation which revealed no external chain-of-custody existed for the specimen rendering it invalid. This was revealed to PHS on October 4th, 2012 but instead of disclosing this and correcting things Dr. Luis Sanchez reported me to the Board for “noncompliance” less than 2 weeks after it was revealed to him that the test was invalid. He then wrote a letter on December 11, 2012 stating that he “just found out” about the invalid test.

Sanchez violates M.G.L. (B) Section 69 on 3 separate occasions 1. July 28, 2011 when he reports the fabricated test to the Board of Registration in Medicine (BORM) 2. October 19, 2012 when he reports non-compliance with my contract leading to my suspension. 3. December 11, 2012 when he reports PHS was made aware of the invalidity of the test the day prior when it was actually 67-days prior (and 2 weeks prior to the report of non-compliance). His attempt at “moving the goal-post” was made clear with the August 2014 provision of the October 4, 2012 report from USDTL to Sanchez. Both USDTL and Sanchez suppressed this information to conceal the crime.

The additional evidence was provided in December of 2011 with the litigation packet. Since that time Ms. Stoller has received exculpatory evidence that undeniably refutes the test including an investigation by the College of American Pathologists. In addition Ms. Stoller has been made aware point by point the crimes involved. She is aware that this is not only “invalid” but the product of forensic fraud. Her stance has been to ignore each and every point and support PHS regardless of facts and truth while professing to serve the public interest.

Letter from USDTL to Sanchez reporting the absence of external chain-of-custody and invalidating the positive test. This was concealed until August of 2014.

While concealing the October 4th test correction Sanchez reports “non-compliance” with A.A. meetings. The positive test was the sole justification for the A.A. meetings.
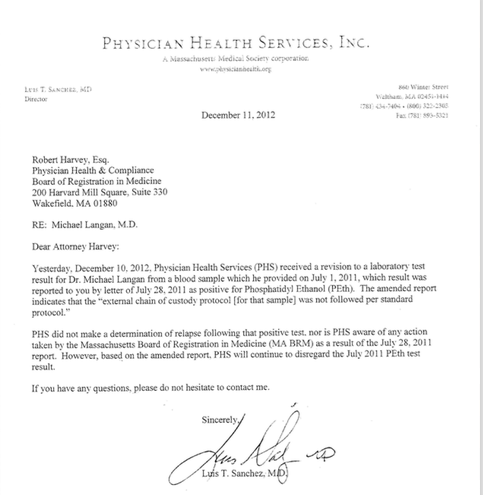
Sanchez claims that he just found out about the revised test 67-days after he actually did. Note he makes it a point to state that the test did not cause any consequences confident that the October 4, 2012 document will remain concealed.
A Request to Inspect and Copy Protected Health Information and Authorization for Use or Disclosure of Patient’s Protected Health Information was sent to USDTL in July and August of 2014.
The July 1, 2011 PEth test was drawn as a forensic specimen and subsequently changed to “clinical” (rendering it PHI) at the request of Quest’s client, PHS, Inc on July 7th, 2011. USDTL sent the materials within the 30 day deadline.
Quest Diagnostics, however, refused to comply with my request for the authorization and release of information forms required for them to draw a clinical specimen (which I knew did not exist) as well as any documentation related to the request by PHS that Quest (in violation of all regulations, professional standards, and clinical laboratory law) changed a “forensic” to a “clinical” specimen. The Quest attorney insisted that I sign a “release” from PHS.
PHS and the colluding labs were apparently unaware of the updated HIPAA regulations removing the need to obtain a signed release from a “provider” to obtain PHI.
I only received it because the DOJ-OCR agreed that this was PHI and forced Quest to send it.
PHS manipulated the test, set up a system in which they could claim me non-compliant , then did so immediately after the test was amended and hoped I would never find out.
On 10/4/2012 USDTL amended the test noting “external chain of custody was not followed per standard protocol” invalidating the test (this was the result of the initial CAP investigation under the assumption it was a forensic test). This was faxed to PHS but they withheld this information from me and the Board of Registration in Medicine.
The very next week they deemed me “non-compliant.”
PHS then officially reported me to the BORM as “noncompliant” on 10/19/2012.
On 12/10/2012 I found out from Amy Daniels of CAP that the test had been amended. I then called PHS and they issued a letter the very next day 12/11/2012 stating “Yesterday, December 10, 2012 Physician Health Services (PHS) received a revision to a laboratory test” referring to the July 1, 2011 PEthstat. They then try to cover themselves by claiming they were not aware of any action taken by the board as a result of this test.
The documents reveal that PHS is violating multiple state and federal criminal laws including clinical laboratory laws. It not only involves forensic manipulation but sending laboratory specimens as “clinical” samples when they are not authorized to do so and misrepresenting them as “forensic.”
Joseph Jones goes on record as a strict advocate of quality control and chain-of-custody with his “Defense in Depth Strategy” video and multiple written documents proclaiming how USDTL follows strict and rigid protocol. Well the ” litigation packet” contradicts and even negates this. How can any of USDTLs testing be trusted in light of what is seen here.
There is nothing that correlates that test with me and for all intents and purposes it could be a positive template used specifically for this type of misconduct. They pointed out that it does not pass the common sense factor (i.e. what would an average person think under normal circumstances about this?)
What it shows is that Mary Howard of PHS changed a test that was drawn as a “forensic” test to “clinical.” She is listed as the ordering “physician.” None of the required information exists to obtain a clinical sample. There are no authorization forms signed by me or to whom the information can be disclosed–clear violations of “Prohibited Activities” under Massachusetts law governing clinical laboratories.
Quest and USDTL representation has already clarified that PHS requested this test be sent by Quest to USDTL as a “clinical sample” with specific instructions to process it as a “clinical” sample. PHS is a monitoring agency not a treatment provider.
A “clinical” laboratory specimen is defined (CLIA, DPH, HHS, state laboratory law, essentially everyone) by its use in the diagnosis and treatment of a patient in a doctor-patient relationship. It necessitates patient “care” which PHS is unable to legally provide as a “non-profit” charitable organization.
As this is both “bad-faith” and ultra vires “confidentiality agreements” and “peer review” protection should no longer be an issue. Just one removes it.
PHS is an agency that utilizes drug and alcohol screens to detect if doctors are using substances they are prohibited to use. It is not a clinical provider. I am sure Bresnahan has spun some sort of logical-fallacy argument to say it is, but the documentary facts negate this. Organizational purpose is clear. As a monitoring agency their drug and alcohol testing is forensic. This brings in to question their “charitable organization” non-profit status.
Accountability requires both the provision of information and justification for actions
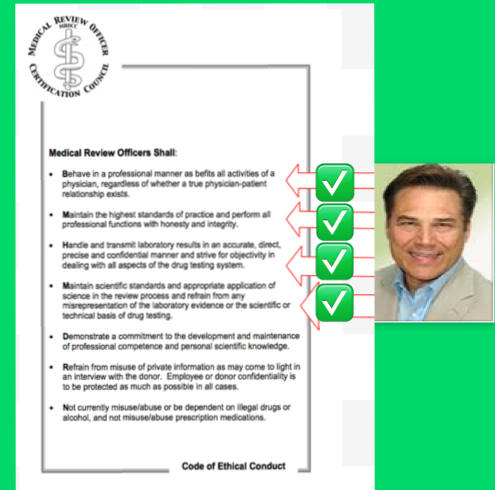
Accountability also requires consequences for violations of professional standards-of-care, ethical codes of conduct and the law
PHS is able to do what they do by both blocking information and relying on others to overlook, table or otherwise dismiss valid complaints–complacent that these are good people helping doctors and protecting the public. The current incarnation does neither
There should be zero tolerance. PHS has been unaccountable for this type of behavior but this needs to be addressed.
Accountability requires both answerability, justification and consequences. There is no conceivable procedural, ethical or legal justification for what is shown here. The compounding of crimes over time is self-evident and therefore it is the responsibility of the state to hold him accountable for his crimes. The fact that he pontificates on professionalism and stands in judgment of others makes it even more important. There are no exceptions to the rules or the law..
And we now know why Quest was so reluctant to provide the records. Quest was complicit in this and obtained and processed a known forensic sample as “clinical” without any of the required documents. The test lists “ordering physician” as Mary Howard (who is a secretary at PHS). There are no signed release of information forms or authorization forms indicating who my PHI could be distributed to.
This is in violation of the HIPAA criminal statute. As a business associate It is my understanding PHS can be tied to it by the conspiracy statute.
There should be zero-tolerance for this type of criminal activity. There is no excuse for forensic manipulation and this must be addressed. The people who are engaging in this should be in jail yet they remain unscathed. This is a systemic problem that is best met with head on and in real time. It makes Annie Dookhan look like a girl scout.
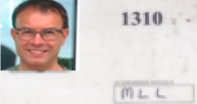
7/1/2011—PHS requests blood test at Quest Diagnostics. No outside factors are involved in PHP requesting this. There is no outside complaint or concern behind it. I provide blood sample using my PHS unique identifier #1310
7/28/2011—verbal report that test was positive to the Board of Registration in medicine and requests I have a “reevaluation.”

I request test results in form of “litigation packet” but PHS tries to dissuade me and eventually threatens me with “unintended consequences.”
11/29/2011—PHS agrees to provide “litigation packet. Check dated 11/29/2011 is given for payment.
12/5/2011—Receive USDTL Litigation Packet Sole document from Quest is a fax that is time stamped and arrived 3 hours after the specimen was collected when I was in clinic at MGH rendering this impossible. In addition it is not my signature:

Signature on Quest document

A fax from PHS to USDTL is also included requesting that my ID # 1310 and a “chain-of-custody” be added to an already positive specimen with no unique identifier connecting it to me.


PHS asking that my ID # 1310 be added to this sample and “chain-of-custody” be updated
A report dated 7/20/11 from USDTL “revised report per clients request” and “corrected donor ID from 46130 to 1310 and “corrected collection date to 7/1/2011”

USDTL adds my ID # 1310 to an already positive sample and adds collection date of July 1, 2011
Note this backdating of chain of custody and addition of my ID # is on 7/20/11 (one day after Dr. Luis Sanchez reported the test as positive to the Board of Registration in Medicine. )


Joseph Jones certifies that the specimen was processed with laboratory SOP. This is signed on 12/3/2011

Note that Dr. Luis Sanchez “explained that the testing laboratory is willing to support the test results and provide the litigation packet’ December 5, 2011
Note- the “PHP-referred” attorneys are an essential part of this racket. Although ostensibly representing your interests they are also serving the PHP as they will not go beyond certain boundaries. They will not address the forensic fraud facilitated by the labs or the “tailoring” of assessments to fit the diagnosis. Their other job is 12-step facilitation. They enforce mandated 12-step and essentially threaten you that the medical board will suspend you if you do not show them you accept it. My attorney would not even contact the labs involved. Although discovery of the fraud would have been exculpatory my attorney felt a better approach would be to blame the positive test on my asthma inhalers and referred me to an “expert witness” who for $3000..00 would write a letter supporting this. I even write a letter for him to USDTL. He will not contact the labs but offers to do so if Linda Bresnahan “wants him to.” The deferential almost sycophantic exchange is seen below.

12/14/2011—Bresnahan replies that the one page document with my forged signature is sufficient external chain of custody.
 12/19/2011–I try to do everything I can to get my attorney to address the lab issue. In any other profession this would have been immediately resolved. The lab fraud would have been exculpatory. but in this rigged system it is avoided. The fact that the attorney who is supposedly working for you is actually working against you is a very significant breach of trust It is an essential part of the racket.
12/19/2011–I try to do everything I can to get my attorney to address the lab issue. In any other profession this would have been immediately resolved. The lab fraud would have been exculpatory. but in this rigged system it is avoided. The fact that the attorney who is supposedly working for you is actually working against you is a very significant breach of trust It is an essential part of the racket.

12/29/12—As I am determined to get the truth about the test I request that when that happens the board allow me to repetition for reconsideration. Confident that the College of American Pathologists will confirm the fraud this letter is written to Board Attorney Deb Stoller.

Letter to Board Attorney Deborah Stoller. My contract with PHS was extended for 2 years because I asked for an evaluation at an independent facility not affiliated with PHS and the Like-minded docs. This letter is important as it shows the import of the PEth test which PHS will later say is irrelevant as they “move the goalpost.
1/12/2012—I send “litigation packet” to the College of American Pathologists (an accreditation agency that does not have power to sanction but can investigate and force lab to correct errors under threat of loss of accreditation)

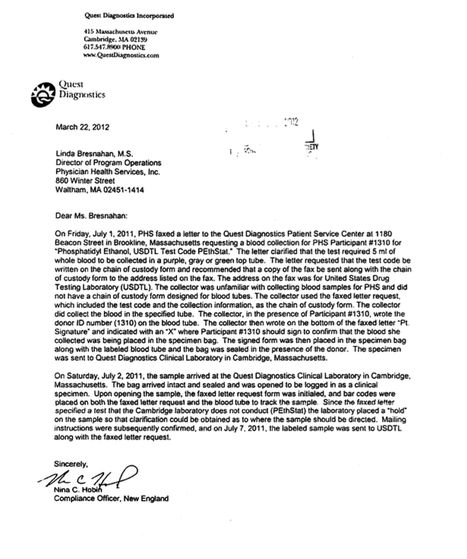
3/22/2012 – Quest New England Compliance Manager, Nina Tobin in response to my persistence in obtaining the absent Quest “chain-of-custody” provides letter documenting all of the errors in collection and process in a letter that seems to try to give the impression some sort of protocol was followed. She notes it was “ logged as a clinical sample.” Note no indication of the validity of the sample and that this was processed as a clinical sample.
10/8 2012 –I am called by my attorney and told PHS is deeming me “noncompliant’ with my contract.
10/19/2012—I am verbally reported to the Board of Registration in Medicine for noncompliance with my contract. This is followed by a written letter: 10:23:12 PHS Letter to BORM-noncompliance

11/5/2012— n appears to be “a purposeful and intentional act by PHS to show MLL’s 7/1/11 test as valid when in reality this test was invalid, and involved both fatal laboratory errors and lack of adequate MRO review of results. Anything based on MLL’s 7/1/11 test as a confirmatory positive should be reversed, rectified and remediated.” This letter remains unacknowledged by Board Attorney Deborah Stoller.
n appears to be “a purposeful and intentional act by PHS to show MLL’s 7/1/11 test as valid when in reality this test was invalid, and involved both fatal laboratory errors and lack of adequate MRO review of results. Anything based on MLL’s 7/1/11 test as a confirmatory positive should be reversed, rectified and remediated.” This letter remains unacknowledged by Board Attorney Deborah Stoller.
12/5/2012 – Contacted by Amy Daniels (investigator for CAP) to follow up on the “appended lab.” She tells me that the July 1, 2011 lab was amended on 10/4/2012 and reported to PHS. I contact PHS and they deny it.
12/11/2012– Dr. Sanchez issues a letter stating “Yesterday, December 10, 2012 Physician Health Services (PHS) received a revision to a laboratory test” referring to the July 1, 2011 test. He claims the test had no consequences.
2/6/2013—I am suspended by Board of Registration in Medicine for the “non-compliance” reported by Dr. Luis Sanchez.
6/23/2014-Letter from PHS attorney Paul W. Shaw claiming PHS immune from damages and documenting that the lab draw was performed by PHS ‘in its capacity as a charitable corporation.” He states “you should be aware that the suspension of Dr. Langan’s license had absolutely nothing to do with the blood test referenced in your letter or any actions on the part of PHS, as detailed in the Board of Registration in Medicine’s {Board Order} dated February 6, 2011” referring to my suspension for the “noncompliance reported by Dr. Luis Sanchez.
6/27/2014—Letter from USDTL attorney William F. Burke stating that “the blood sample was tested clinically at the request of Quest Diagnostics” and that “Dr. Langan’s blood sample was provided to USDTL by Quest Diagnostics on behalf of Physician Health Services as part of medical treatment..” He states “Dr. Langan’s suspension was the result of his inability to comply with the terms of his contract.”
8/6/2014—in response to my request for PHI USDTL provides record. This includes documentation that Dr. Luis Sanchez was made aware of the revised test on 10/4/2012. Note the very next week on 10/8/12 my attorney informed me that he was reporting me to the Board of Registration in Medicine for “noncompliance’ and officially did so on 10/19/12.

Also included in the record is an e-mail from me to Dr. Jones December 10, 2012 with subject “please provide amended lab report.” I request a copy of the amended lab report ASAP specifically to “clarify the truth about this test as explicitly as possible before this goes any further.” I state “PHS has used this test to cause, and continue to cause, a significant amount of harm.” He does not respond to this request for what is now documented PHI. I am suspended 2 months later for non-compliance.
Joseph Jones had already corrected the test 10/4/2012 but both he and PHS concealed it while PHS “moved the goalpost” by deeming me non-compliant.
10/9/14—Receive documents from Quest Attorney Fay Caldwell. No release of information forms or other HIPAA required documentation is found.
Ordering Physician is listed as Mary Howard. (secretary at PHS). Documents reveal no custody and control form information only that it was changed to a clinical specimen by Ms. Howard on July 5, 2011 and sent to USDTL on July 7,2011.

Blind-faith and unquestioning allegiance to expert authority deflects scrutiny and analysis. Few red flags are raised as this type of moral preening promotes misguided plausibility and complacency in the belief that these are indeed experts with good intentions. This needs to be addressed.


































 Accountability needs to be rooted in organizational purpose and public trust.
Accountability needs to be rooted in organizational purpose and public trust. ce of unchecked power. The only two factors that constrain corruption are moral virtue and deterrence.
ce of unchecked power. The only two factors that constrain corruption are moral virtue and deterrence. arketed it as the PEthStat.
State Physician Health Programs are now using the EtG and adding the PEth to confirm alcohol ingestion. And just as they did with the EtG the claims of reliability are grand but without foundation.
All speculative A=B oversimplified thinking that ignores the myriad other factors involved. The science is empty if you remove the dregs of filler and puff. And the conflicts of interest are mind-boggling.
arketed it as the PEthStat.
State Physician Health Programs are now using the EtG and adding the PEth to confirm alcohol ingestion. And just as they did with the EtG the claims of reliability are grand but without foundation.
All speculative A=B oversimplified thinking that ignores the myriad other factors involved. The science is empty if you remove the dregs of filler and puff. And the conflicts of interest are mind-boggling.




























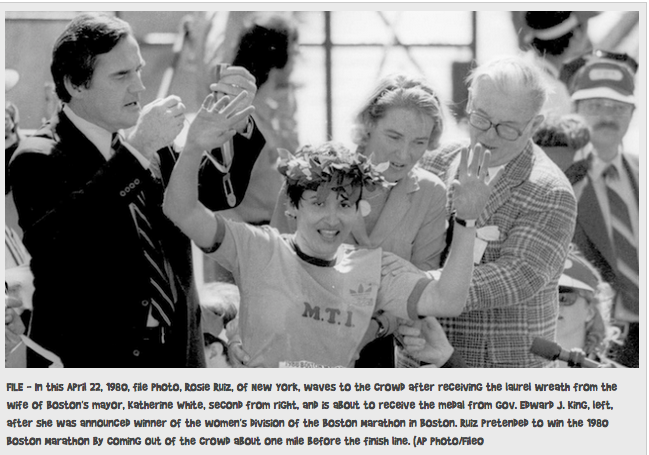 On April 21, 1980 Rosie Ruiz appeared to win the 84th Boston Marathon’s female category with a time of 2:31:56. Her time would have been the fastest female time in Boston Marathon history and and the third-fastest female time ever recorded in any marathon.
On April 21, 1980 Rosie Ruiz appeared to win the 84th Boston Marathon’s female category with a time of 2:31:56. Her time would have been the fastest female time in Boston Marathon history and and the third-fastest female time ever recorded in any marathon.



 Sauerkraut and bananas have even recently been shown to cause positive EtG levels.
Sauerkraut and bananas have even recently been shown to cause positive EtG levels.