“Some people without brains do an awful lot of talking, don’t you think?”
― L. Frank Baum, The Wonderful Wizard of Oz

Elmer Gantry
Sinclair Lewis’ 1927 novel Elmer Gantry is a satire on fundamentalist religion in 1920s America. The eponymous character is a greedy and debauched womanizer who reinvents himself as an evangelical minister. The Reverend Dr. Elmer Gantry is a carney huckster who weasels himself into becoming the leader of a large Methodist congregation. He organizes crusades against immorality while he himself is amoral. Gantry is an unethical and unprincipled power hungry narcissist who contributes to the downfall, injury and even death of those around him. Lewis’ portrayal of pious hypocrisy and opportunism of fanatical religiosity was denounced from pulpits across the country. The book was banned in Boston and many other cities with official censorship boards. Public libraries and some booksellers refused to stock it and the author was threatened with litigation, jail, injury and even death. The attempts at censorship backfired and the novel quickly went to number one on the fiction bestseller list.
The “religion racket” no longer has the power to determine what we read. Unfortunately, similar groups have gained tremendous sway. The “rehab racket” has erected a scaffold able to remove our constitutionally protected rights and civil liberties not only legally but under the pretense of doing so out of our own best interests. According to Erich Fromm rational authority is based on competence, experience and mutual respect. Irrational authority is often disguised as benevolent paternalism and is designed to perpetuate or intensify conditions of inequality through the use or threat of force, deceptiveness and secretiveness.
This system has unfortunately given power and allowances to unethical individuals who are able to exert control over other individuals under the guise of “treatment” regardless of whether or not those individuals even need it as inherent in the current chronic brain disease model of addiction is the importance of external control.
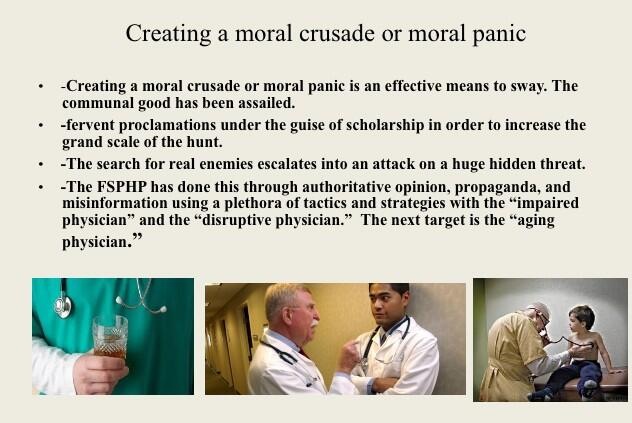
The Federation of State Physician Health Programs (FSPHP) has has played a large part in this. The FSPHP has operated as an unexamined authority for the past 25-years and contains individuals whose pious hypocrisy and carney hucksterism would make Gantry blush. Everything they have done has been done to benefit themselves and their drug and alcohol assessment, testing and treatment affiliates in the provision of protections, power and profit. The FSPHP has pushed bad practice and policy with no discernible scrutiny or meaningful opposition. The impact of any and all of this has yet to be examined. It needs to be.
In Democracy in America Alexis de Tocqueville (1805-1859) warned that the greatest threat the United States faces is the “tyranny of the majority “and that state power would end up concentrated in a single authority until its citizens were “reduced to nothing better than a flock of timid and industrious animals, of which the government is the shepherd,” noting that the newest incarnation of despotism was likely to be ushered in by the “avowed lover of liberty” who is a “hidden servant of tyranny.” “Written laws exist in America,” he wrote, “and one sees the daily execution of them; but although everything moves regularly, the mover can nowhere be discovered. The hand which directs the social machine is invisible” Today several thousand “legislative rules” and regulations are passed each year silently. The impact of this so-called “regulatory dark matter” is usually unknown until it hits us and such is the case here.
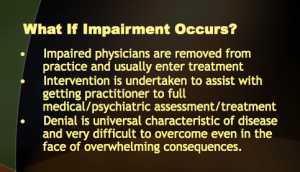
Examining the specific practice and policy that has been pushed by the FSPHP (and ratified by state medical boards and their national organization the Federation of State Medical Boards) reveals a body of false-claims making that is designed to facilitate the systemic use of coercion and threats, removal of due process protections and fundamental rights from physicians (and other health care professionals) and prevent, block and eliminate any evidence of the consequences. This practice and policy collective has created a culture of impunity, immunity and deference that is able to successfully conceal egregious ethical violations and crimes. Uncovering and exposing this wrongdoing is nearly impossible as the gauntlets that have been put in place are multiple and they remain largely unseen. What lies beneath, however, is self-apparent and this system of institutional injustice is undoubtedly a major contributor to the grossly underreported suicide epidemic in the medical profession and the reticence of those who actually need help with substance use and other mental health problems to seek help for those problems. They are afraid an it is as plain-and-simple as that.
The FSPHP has been able to conceal the truth, avoid investigation and prevent punishment for wrongdoing for years and they have done this by systematically and systemically removing themselves from all accountability and all outside inquiry.
Direct and specific questioning appears to be their Achille’s heel as has been seen in the increasing torrent of articles and reports critical of these programs . In a rebuttal to Pauline Anderson’s article “Physician Health Programs: More Harm Than Good?” FSPHP President Doris Gunderson dismissed concerns of fraud and abuse in one fell swoop as “allegations rather than facts” and as second hand anecdotes. Countering allegations of an absence of oversight and regulation she states:
“In fact, we operate under a microscope, answering to individual practitioners, medical boards, malpractice carriers, defense attorneys, state attorneys, medical societies, hospitals, medical schools and residency training programs. We are also accountable to patient safety entities and a Board of Directors.”
Untrue. Accountability demands both provision of information and justification for actions to outside entities capable of punishing misconduct. . What was done and why? No such entity exists and no pathway for appeal or grievance redressal exists either. Zero accountability. Ditto for the “PHP-approved” assessment and treatment centers. As cash only out-of-pocket private facilities they remove themselves from the prying eyes of insurers.
In response to Emmy Award winning P.J. Randhaw’s 2019 investigative journalism piece addressing these issues seen here the FSPHP and its state affiliate would not even respond to direct questioning on these issues. The stance seems to be to ignore these systemic and serious allegations and hope they will go away. They will not go away. Simple and direct questions deserve simple and direct answers and the unwillingness to address the particular and remarkably similar allegations of exceptionally egregious misconduct and fraud is unacceptable. The silence speaks volumes.
The North Carolina PHP Audit found the past FSPHP President and NC PHP director Warren Pendergast could not even identify qualitative or quantitative indicators that are used for “approving” the “PHP-approved” assessment centers. The best justification he could come up with was “reputation” and “word of mouth” yet state medical boards (and other licensing boards) mandate evaluations at these facilities and specifically exclude non-“PHP-approved” facilities.
This is enforced by the Federation of State Medical Boards Policy on Physician Impairment. Each state managed by the FSPHP utilizes the same dozen or so facilities and each state medical board mandates it under threat of disciplinary action. It is in fact a rigged game.
Denying accusations of coercion Gunderson states in her rebuttal to Anderson’s article:
“The detractors of PHPs interviewed for the article maintain that PHPs are coercive. Yet the report fails to mention that PHPs have no authority to mandate treatment and monitoring, suspend or revoke licensure, or otherwise discipline physicians.”
 The report fails to mention it because it is more either/or logical fallacy based on the false dichotomy between “treatment” and “punishment” that is often used to promote the FSPHP mythology. Although PHPs do not have the legal authority to mandate, suspend or revoke a license they have the functional authority to do so. This is also dictated by public policy. (ASAM Policy on Coordination Between Treatment Providers, Professionals Health Programs, and Regulatory Agencies).
The report fails to mention it because it is more either/or logical fallacy based on the false dichotomy between “treatment” and “punishment” that is often used to promote the FSPHP mythology. Although PHPs do not have the legal authority to mandate, suspend or revoke a license they have the functional authority to do so. This is also dictated by public policy. (ASAM Policy on Coordination Between Treatment Providers, Professionals Health Programs, and Regulatory Agencies).
Legitimate authority articulates ethical, evidence-based, or internally consistent arguments when challenged. Legitimate authority does not simply delegitimize one’s opponent and use logical fallacy and obfuscation to avoid addressing the substance of the argument. In her rebuttal Gunderson claims the North Carolina Audit was favorable because no evidence of abuse was found. This is akin to a serial killer claiming victory because no bodies were found in his dungeon replete with torture devices and restraints. State auditor Beth Woods set this straight when she told the BMJ in Physician Health Programs Under Fire that the holes were big enough in the program “you could drive a truck through them” and it would be “difficult, if not impossible, to defend” oneself against an incorrect assessment” as no ability to “appeal a diagnosis or assessment” existed.
 “Compounding the problem, said Wood, was that “the chief executive and medical director were in total control of entire process.” They assessed allegedly impaired doctors, but when those assessments were contested, they were responsible for presenting complaints to the state medical board. The doctors concerned were not allowed to be present and were not allowed to see the programs’ medical reports on them.”
“Compounding the problem, said Wood, was that “the chief executive and medical director were in total control of entire process.” They assessed allegedly impaired doctors, but when those assessments were contested, they were responsible for presenting complaints to the state medical board. The doctors concerned were not allowed to be present and were not allowed to see the programs’ medical reports on them.”
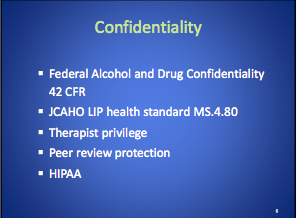
The inability to obtain one’s own medical records or lab reports is the first obstacle one must overcome. The second barrier is that even if documents are obtained there is no one to give them to. The third is the existence of “point people” who deflect, block and otherwise dismiss valid complaints. The only oversight provided to the involved labs is an an accreditation agency, the College of American Pathologists (CAP) They can investigate and correct but do not have the ability to sanction.
 Of the many hundreds of doctors I have spoken to and who have taken my survey not one has been able to obtain evidence of abuse. It was either refused, censored or doctored.
Of the many hundreds of doctors I have spoken to and who have taken my survey not one has been able to obtain evidence of abuse. It was either refused, censored or doctored.
Research on street criminals suggests the certainty of punishment has the strongest deterrent effect (basically will I be caught) and the more people think they will be arrested for a crime the less likely they are to commit it.
Criminals weigh their actions against possible gains and consequences and the risk of consequences in this system have been essentially zero. Diagnosis rigging, coercion, threats and abuse are rampant because they have no fear of punishment.
The Chairman of the commission that examined the causes of the 2008 financial collapse compared the relatively small fines paid by corporations to “someone who robs a 7-Eleven, takes $1,000 and being able to settle for $25 and no admission of wrongdoing.” He added,“Will they do it again? Absolutely, because it pays.”
This misconduct that is seen in this racket is comparable to someone who robs a 7-Eleven for $1,000 and never gets caught so then robs as many 7-Elevens as he can for as much as he can and then realizing there is essentially zero chance of getting caught expands the enterprise to robbing as many convenience stores as he can.
This illegitimate authority of self-proclaimed experts has successfully gained power and removed all accountability. Unethical and unprincipled narcissism has unfortunately become the tone at the top.
Tone at the Top

An expectation of irreproachable ethics and honesty ideally sets the bar for leadership in any organization. Without ethical integrity, falsity will flourish.
Adherence to societal and professional ethical codes is a universal obligation. It excludes all exceptions. Good leadership requires correct moral and ethical behavior of both the individual and the organization. Integrity is necessary for establishing relationships of trust. It requires a true heart and an honest soul. People of integrity instinctively do the “right thing” in any and all circumstances.
“Tone at the top” refers to the ethical atmosphere created by an organization’s leadership as it creates an ethical atmosphere that inevitably cascades throughout the organization – for good or for bad as the case may be. A strong tone at the top is essential to ensure strong internal control and effective governance. It requires that upper management lead by example and action. This includes rewarding ethical behavior and punishing misconduct. An ethical tone at the top holds those below accountable for unethical actions and imposes sanction those who do bad things and improper or unethical conduct is not tolerated, condoned or overlooked.
But when those in top positions set the wrong it will inevitably trickle down as those below follow in their leaders fraudulent footsteps. Unprincipled and unethical leaders create unprincipled and unethical followers and this creates an organizational culture that becomes a breeding ground for corrupt practices such as conflicts of interest, self-dealing, illegal activities and abuse. Such a culture places both the viability of the organization and its stakeholders at risk.
In his book Without Conscience, Dr. Robert Hare notes “If we can’t spot them, we are doomed to be their victims, both as individuals and as a society” and Dr. Clive Boddy in Corporate Psychopaths observes that “unethical leaders create unethical followers, which in turn create unethical companies and society suffers as a result.”
The Federation of State Physician Health Programs (FSPHP) make authoritative pronouncements on professionalism and ethics. In Disruptive Behaviors Among Physicians past president of the organization Dr. Luis Sanchez pontificates on a “culture of safety“ and promotes “clear expectations and standards.” He calls on leaders in the medical profession to “commit to professional behavior” and to lead by example. But truth is comprehended by examining actions not words. One measure of integrity is truthfulness to words and deeds and by that measure Sanchez, Skipper, Teitelbaum, Pendergast and numerous other self-proclaimed “leaders” of the “physician-wellness” movement fall miserably short.
As with Reverend Dr. Elmer Gantry the carney huckster who weaseled himself into becoming the leader of a large Methodist congregation these individuals have managed to weasel themselves into positions of power and the impact has been far reaching and grave. Organizing crusades against immorality while he himself was amoral the unethical and unprincipled power hungry narcissist Gantry contributed to the downfall, injury and even death of those around him. So too have the pious hypocritical opportunists who have reinvented themselves as experts and authority in this arena and unless courage and resistance steps up the noble profession of medicine will be utterly demolished without a brick standing.












 also follow their own
also follow their own  Both the donor ID # and chain of custody are listed as 461430.
Both the donor ID # and chain of custody are listed as 461430.













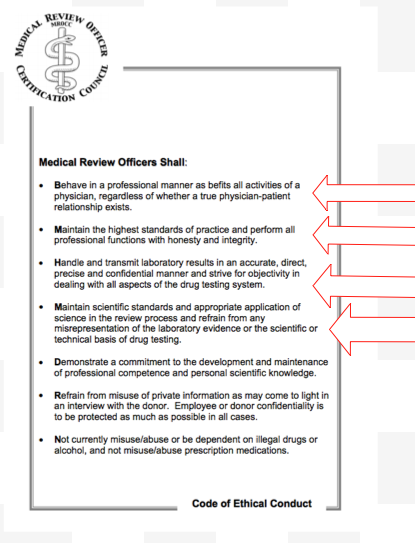









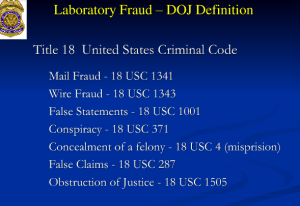


 As a physician-patient relationship renders drug testing “clinical” rather than “forensic” the consequences become “treatment” rather than “discipline.” And that is the real reason behind all of this. A positive “forensic” test in most employee random drug screening programs today will result in an “assessment” for substance abuse. Most EAPs allow a choice in where that assessment takes place. The model this system is based on, Physician Health Programs. do not allow choice as evaluations are mandated to “PHP-approved” assessment centers; a rigged game.A positive “clinical” test will result in the same thing under the ASAM White Paper proposal. But the assessment will be at an ASAM facility and if a Substance Use Disorder (SUD) is confirmed it will result in mandated abstinence of all substances (including alcohol) and lifelong spirituality involving 12-step recovery And by using the healthcare system as a loophole and calling this testing “clinical” rather than “forensic” the ASAM will have successfully introduced widespread testing of a variety of Laboratory Developed Tests (LDTs) of unknown validity while removing the safeguards provided by forensic testing including chain-of-custody and MRO review.
As a physician-patient relationship renders drug testing “clinical” rather than “forensic” the consequences become “treatment” rather than “discipline.” And that is the real reason behind all of this. A positive “forensic” test in most employee random drug screening programs today will result in an “assessment” for substance abuse. Most EAPs allow a choice in where that assessment takes place. The model this system is based on, Physician Health Programs. do not allow choice as evaluations are mandated to “PHP-approved” assessment centers; a rigged game.A positive “clinical” test will result in the same thing under the ASAM White Paper proposal. But the assessment will be at an ASAM facility and if a Substance Use Disorder (SUD) is confirmed it will result in mandated abstinence of all substances (including alcohol) and lifelong spirituality involving 12-step recovery And by using the healthcare system as a loophole and calling this testing “clinical” rather than “forensic” the ASAM will have successfully introduced widespread testing of a variety of Laboratory Developed Tests (LDTs) of unknown validity while removing the safeguards provided by forensic testing including chain-of-custody and MRO review.




 Circa 1995
Circa 1995 
 The Constitution reported that those in charge of the program are often “physicians who themselves have successfully completed Ridgeview’s program.”
The Constitution reported that those in charge of the program are often “physicians who themselves have successfully completed Ridgeview’s program.” The cost of a 28 day program at Ridgeview was $10,000 but far more for the thrice lengthy stay required by healthcare professionals..
The cost of a 28 day program at Ridgeview was $10,000 but far more for the thrice lengthy stay required by healthcare professionals.. Nonsense such as the “four-MDs” and thrice lengthy treatment has been accepted without scrutiny. Logical fallacy is written as science. For example Merlo and Gold use the “appeal to consequences” logical fallacy to justify the extended length of stay stating that “physicians with a substance use disorder are not typical of addicts in general, it is not useful to apply standard professional guidelines… Rather, because of the public health consequences of relapse, most physicians who are addicted are treated more aggressively and for longer periods” than non-physicians.
Nonsense such as the “four-MDs” and thrice lengthy treatment has been accepted without scrutiny. Logical fallacy is written as science. For example Merlo and Gold use the “appeal to consequences” logical fallacy to justify the extended length of stay stating that “physicians with a substance use disorder are not typical of addicts in general, it is not useful to apply standard professional guidelines… Rather, because of the public health consequences of relapse, most physicians who are addicted are treated more aggressively and for longer periods” than non-physicians.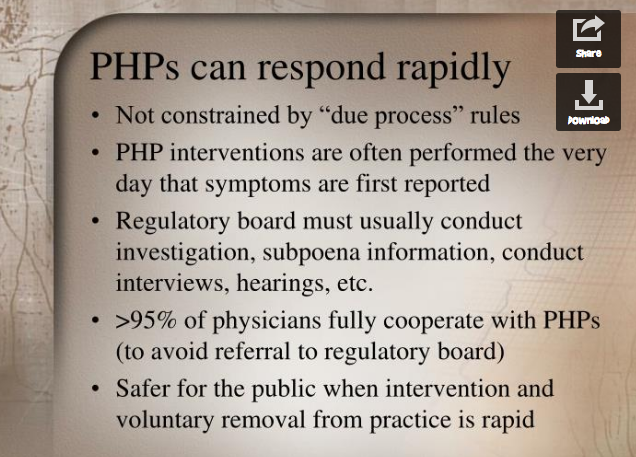 “Process addiction” was added as a potentially impairing illness including compulsive gambling, compulsive spending, compulsive video gaming, and “workaholism.” According to the FSPHP “the presence of a process addiction can be problematic or even impairing in itself, and it can contribute to relapse of a physician in recovery. As such, process addictions should be identified and treated.” They define three levels of relapse. “Relapse without use” is a 12-step concept. G. Douglas Talbott defines it as “stinkin thinkin.”
“Process addiction” was added as a potentially impairing illness including compulsive gambling, compulsive spending, compulsive video gaming, and “workaholism.” According to the FSPHP “the presence of a process addiction can be problematic or even impairing in itself, and it can contribute to relapse of a physician in recovery. As such, process addictions should be identified and treated.” They define three levels of relapse. “Relapse without use” is a 12-step concept. G. Douglas Talbott defines it as “stinkin thinkin.”
 What is so egregious about this is there was absolutely no evidence base. Skipper, who was convicted of a felony in Oregon and had his licenser revoked but got it back by claiming he was redeemed through A.A. read about it and after a study on just 14 patients pitched it to a drug testing company as a Laboratory Developed Test (LDT). The LDT pathway is a shortcut to get lab tests approved (under the premise that it will be used in treating a person medically and is thus of benefit) but Skipper took advantage of this loophole to develop a “forensic” LDT. He then used his position as the Alabama PHP Director to pitch it to the Medical Board before the ink dried.
What is so egregious about this is there was absolutely no evidence base. Skipper, who was convicted of a felony in Oregon and had his licenser revoked but got it back by claiming he was redeemed through A.A. read about it and after a study on just 14 patients pitched it to a drug testing company as a Laboratory Developed Test (LDT). The LDT pathway is a shortcut to get lab tests approved (under the premise that it will be used in treating a person medically and is thus of benefit) but Skipper took advantage of this loophole to develop a “forensic” LDT. He then used his position as the Alabama PHP Director to pitch it to the Medical Board before the ink dried.



 Random drug-testing done in the workplace is also forensic but the consequences are usually quite different. A positive drug-test done in this manner typically results in an assessment, treatment if indicated, and compliance with some sort of monitoring protocol in order to return to work.
Random drug-testing done in the workplace is also forensic but the consequences are usually quite different. A positive drug-test done in this manner typically results in an assessment, treatment if indicated, and compliance with some sort of monitoring protocol in order to return to work.

