Although the current use of these tests is limited to the criminal justice system and professional monitoring programs this may soon change as the American Society of Addiction Medicine is proposing a “new paradigm” of zero-tolerance random widespread drug and alcohol testing. This is outlined in the ASAM White Paper on Drug Testing and described by Robert Dupont in his keynote speech before the Drug and Alcohol Testing Industry Association (DATIA) annual conference in 2012.
The ASAM White paper states drug testing is “vastly underutilized” throughout healthcare and describes the use of drug testing “within the practice of medicine and, beyond that, broadly within American Society.”
As the consequences of a single unregulated “forensic” test result can be grave, far-reaching and even permanent it is critical that these tests be included in the debate on regulation of LDTs.
Evidence based medicine is not restricted to randomized trials and meta-analyses. It involves tracking down the best external evidence with which to answer our clinical questions.11
Expert opinion is the lowest level of evidence available in the EBM paradigm.12,13 Fortunately, the scientific method and Cochrane type critical analysis of the available evidence is a tool to help people progress toward the truth despite their susceptibilities to unconscious confirmatory bias or conscious confirmatory distortion .14 Unfortunately, no one has used these tools address they panoply of tests of unknown validity that have already entered the market ; poised to be used on virtually everyone.
Please donate to DisruptedPhysician.com below
https://www.gofundme.com/PHPReform
Drug Testing
Concealing crimes at the Massachusetts Board of Registration in Medicine: Why is this swamp not being drained?
Some day a real rain will come and wash all the scum off the streets- Robert De Niro
Massachusetts Public Records – House Bill 4333
Collusion between state physician health programs (PHPs) and commercial drug testing labs using non-FDA approved drug and alcohol tests

I recently offered 25,000 dollars in prizes to anyone who could disprove that Dr. Luis Sanchez committed multiple felonies based on documents that provide direct evidence of a chargeable crime. No additional evidence is needed. So far no one has been knocking at my door and nary a call from anyone.
How can we interpret this? Are the prizes not worthy of the time involved in such an endeavor? No, I think there is something for everyone including 2oo volumes of the Classics in Medicine. A current listing on Amazon is listing 187 volumes for almost $5000 and in addition to this I am offering dozens of 1970s skateboards, 2 vintage Schwinn Krate bikes, autographs from polio vaccine pioneers Sabin and Salk, multiple signed and one-of-a-kind items related to Boston politician James Michael Curley, a menu, cocktail menu, matchbook and other very rare items from Boston’s Cocoanut Grove which was the site of the deadliest nightclub fire in history in 1942, signed lithographs and prints from Warhol and Keith Haring and a signed poster from Adam Ant. So the prizes are not chopped liver and burnt toast. The prizes are worthy so in a time or work/benefit analysis the benefits are high. What about the time or work involved? Would the work and time it takes to disprove this claim make it not worth the effort like trying to prove some logic or mathematical theorem? The James Randi Educational Foundation offered 1 million dollars to anyone who could prove that homeopathy works but no one has claimed it yet. Why? Because homeopathy does not work. My challenge is fairly simple as the documents are a quick read and the claims direct and specific. All one has to do is read the documents in search of acts that might be considered crimes and use a legal reference to see if they correspond to criminal code. If your examination of the documents finds everything is on the up-and-up or just one or two acts commensurate with felonies then the prizes are yours. A simple task that should take less than an hour or two. So why is no one knocking at my door? No one is knocking for the same reason the million dollar homeopathy reward hasn’t been claimed. The reason no one is knocking at my door is because Luis Sanchez did in fact commit multiple felonies. I could double the prizes, give you everything I own and offer my very soul but there would still be no one knocking.
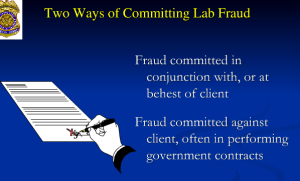
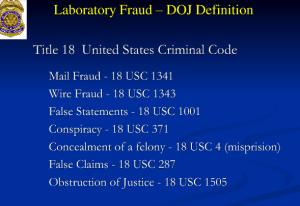
So the question for us is this, how is it possible that an individual contracted by a state agency could commit felony crimes that are documented by direct evidence and not be called on it? The crimes include flagrant forensic fraud no different from Annie Dookhan who faked, forged and fabricated some 60,00 samples at the Massachusetts crime lab. Fabricating evidence is fabricating evidence so how is it possible that this fabrication of evidence has not been identified and addressed by anyone? First of all there is no direct oversight or independent oversight to state physician health programs (PHPs). Not one agency exists that can accept a complaint, investigate it and punish offenders. Second, there is an inability or unwillingness to investigate or punish the offenders for various reasons. PHPs have portrayed themselves as allies to law enforcement and have requested they defer to them any issues related to physicians. When crimes are reported to local and state police and other law-enforcement agencies they are deemed the illusory product of a diseased mind. States Attorneys General legally represent occupation board. Policy dictates they side with medical boards so individual doctors are rebuffed if they ask for help. The FBI will not investigate. I was told unless the AGO requested it or a public outcry ensued they would not address any issues regarding physician health programs including laboratory fraud and diagnosis rigging. This inability or unwillingness to meaningfully investigate the offenders is a pervasive problem and represent a total systems failure. No one is minding the minders and no one wants to mind the minders. The agencies that could and should investigate crimes are taking a “not-my-problem” stance. The medical boards have agreed to absolute deference to PHPs and additionally have individuals or groups within the board who are able to block, deflect and otherwise dismiss information implicating the state PHP. All of the documents seen below were provided to Physician Health and Compliance Board counsel Deb Stoller beginning in 20111 but she apparently kept all the documents to herself. Her ethical obligation when being provided with evidence of forensic fraud and other crimes was to notify the proper authorities. She did not. She suppressed all of the information with direct evidence of crimes, an act that is much more grave and vile than Dookhan as the documents show collusion between the MA PHP and one of the drug testing labs used by almost all state PHPs. The documents provide direct evidence of lab fraud and falsification of evidence that is clear and specific. No alternative explanations exist. Concealing this type of misconduct just allows it to continue and what is seen here is not rare. I have heard from many many doctors who claim they were given bogus tests at this very same lab. Sadly I have heard of many suicides related to these very same tests. Faced with the “not my problem” stance of agencies that could and should do something but did not these doctors became hopeless and helpless and killed themselves out of despair. Their locus of control was completely lost and their was no lifeline. Selective application of the law is the root of government corruption and destroys the moral authority of the government. It inevitably leads to collapse and chaos. The Massachusetts Board of Registration in Medicine has ignored these documents for five years and assert that the PHP has not committed any crimes because they have not been charged with any crimes. Nonsense and logical fallacy. The PHP did commit crimes and so too did Board attorney Deb Stoller when she was given direct evidence of them–misprision of a felony in multiples.
Ignoring misconduct not only allows it to continue it allows it to spread. The plan is to spread these same non-FDA approved of unknown validity and easily manipulated with no accountability to other populations including students and kids. It was also recently suggested that the organization Luis Sanchez is past president of, the Federation of State Physician Health Programs (FSPHP) be put in charge of national public policy for not just doctors but for everyone.
The simple fact is that doctors are being subject to diagnostic rigging and forensic fraud and nobody cares. This is by design and fueled by the anti-doctor sentiment spread by these same groups with propaganda meant to spread the bogus dangers of a hidden cadre of drug addled and besotted doctors. It doesn’t exist but the stature of doctors in the public eye has suffered because of the mythology they created. Don’t get me wrong as any doctor with a substance abuse problem or addiction should be removed from practice and not be able to practice until safe to do so. But that is not what is happening here.
The majority of doctors being monitored by state physician health programs do not have a problem. They have loosened the diagnostic criteria so that essentially anyone referred to them is given a diagnosis and treated. Why? Because it is a money maker. All costs are out-of-pocket and no insurance is involved. The “PHP-approved” assessment centers all charge around $ 4500 for an “assessment” which inevitably leads to a 3-month inpatient stay for treatment to the tune of about $80,000. This is then followed by a five-year monitoring contract with random drug and alcohol testing 1-3 x per week. That is a total of 260 to 780 tests and the laboratory developed tests are not cheap. You do the math. The drug and alcohol assessment and testing industry makes a pretty penny off this operation and they want to bring it to you-It is in fact a Trojan horse.
So by ignoring this type of misconduct it will only get worse. People tend not to get concerned unless it impacts them. This will. Someday you or a family member may be in this same situation. It boggles my mind that doctors can be given diagnoses when they do not meet the criteria for the given diagnosis and this is confirmed by outside independent experts. This occurs because those giving the diagnosis have no accountability. They have removed themselves. But in actual fact this is political abuse of psychiatry. It is egregious.
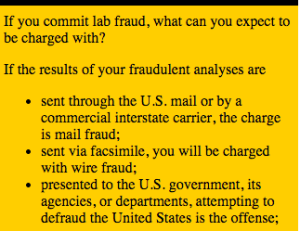
Diagnosing someone with a disease they do not have should be a never event. The perpetrators should not only have their licenses removed but they should be punished for the crime. Forensic fraud should also be a never-event but as seen below it is done without fear of sanction-by fax no less. Giving false diagnoses and fabrication of drug and alcohol tests are actions that should never be tolerated. Not even once. How can this be happening in the United States of America? Unless people speak up this will only escalate. Below is a detailed analysis of the multiple crimes used for the $25,000 challenge. Give it a read and try to disprove the claim that Luis Sanchez committed multiple felonies. If you can you win all the prizes. If you can’t then I ask that you be outraged and do something about it as you or someone you love may be next. Ignoring this type of misconduct is not going to make anything better.
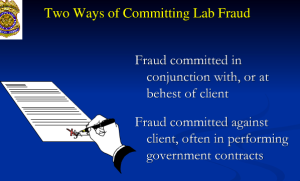
Fraud is distinguished from negligence, ignorance, and error by virtue of the fact that it is intentional. Fraudulent intent is established by examining the documentation of decisions and behaviors of those involved.
Innocent parties don’t normally alter documents or conceal information.
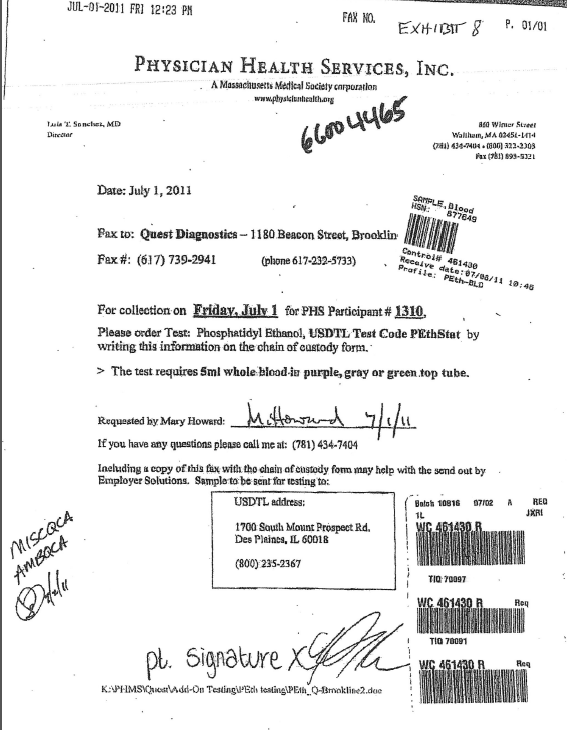
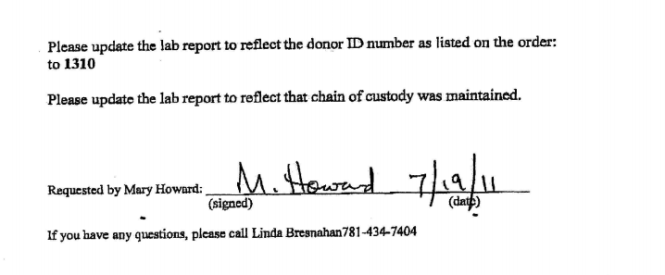
Innocent parties don’t normally “update” donor ID numbers or lab reports to “reflect that chain of custody be maintained as requested in the document below faxed from Physician Health Services, Inc. (PHS) to United States Drug Testing Laboratories (USDTL) on July 19th, 2011.
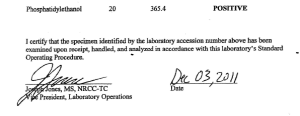
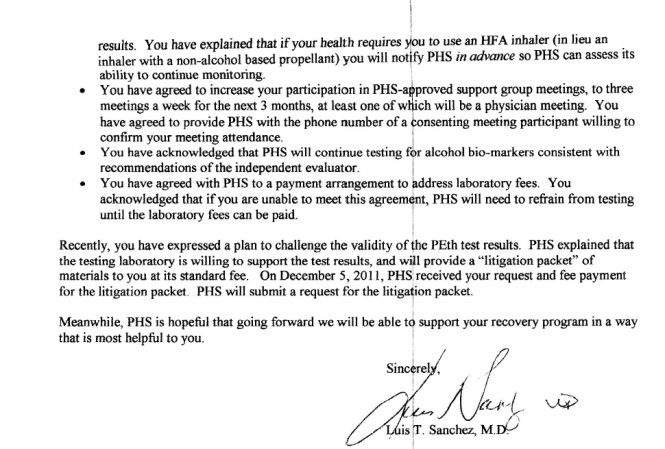
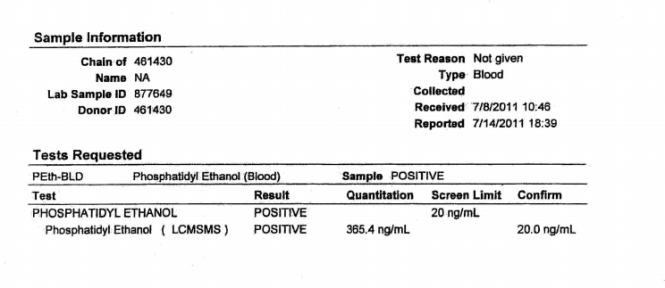
The lab report PHS is referring to is seen below which is positive for the alcohol biomarker phosphatidylethanol at a level of 365.4 ng/ml (cutoff level for a positive test is 20 ng/ml.
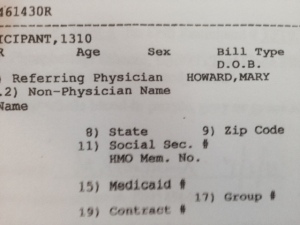
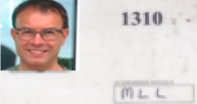
Note both the chain of custody and Donor ID # are listed as 461430 and there is no collection date, collectors name or location listed. The specimen was received on July 8, 2011 and reported on July 14, 2011 according to the document. On July 19th, 2011 Mary Howard requests that a collection date of July 1st, 2011 be added and that the Donor ID # be changed from 461430 to #1310.
What is the significance of this? My unique identifier for for random drug and alcohol testing is #1310 and I had this same test drawn on July 1st, 2011.

The document are from the USDTL “Litigation Packet” received December 3, 2011 which can be seen here: USDTL-LitigationPacket12:2011
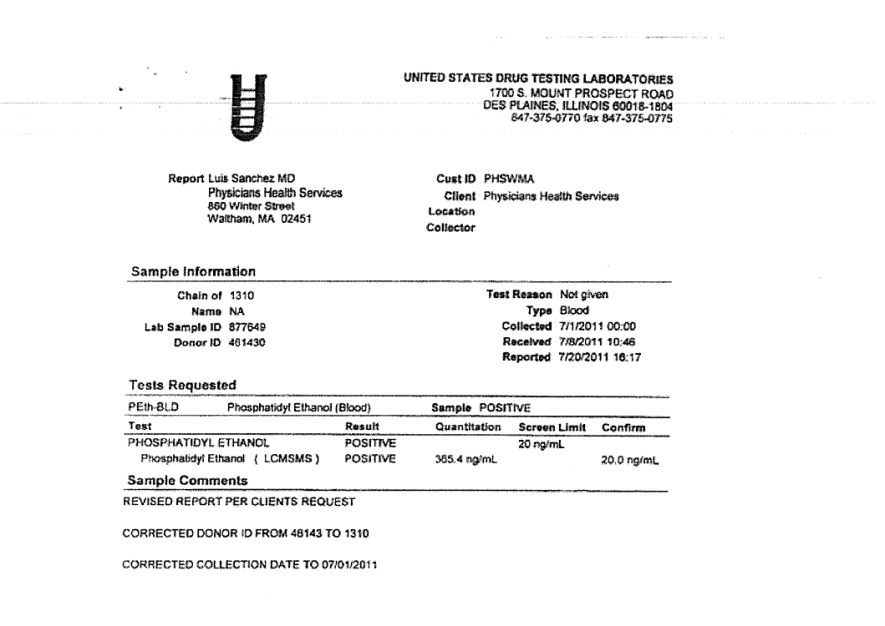
USDTL “updated” the test. The document below shows they added my ID # and a collection date of July 1, 2011.
It is the responsibility of the Medical Review Officer (MRO) to make the final determination as to whether or not the positive result reported by the laboratory is reported to anyone else.
The previous Medical Director of the Massachusetts PHP, Physicians Health Services, Inc. (PHS) for fourteen years, Dr. Luis Sanchez, is also a past President of the FSPHP although PHS did not enter into formal partnership with the FSPHP until 2013. The Director of Program Operations at PHS, Linda R. Bresnahan, MS, is the current Secretary of the FSPHP.
PHS, inc. exclusive use of out of state treatment programs has been challenged. In the past PHS, Inc. has adamantly refused to allow physicians to be evaluated in State despite it being one of the medical hubs of the country. Physicians in Massachusetts who are referred for evaluation in Kansas, Georgia, Alabama, and West Virginia as PHS has convinced the Board that only these facilities are ‘experienced in the assessment and treatment of health care professionals.” In actual fact the medical directors of all of these preferred facilities are also ASAM physicians with the vast majority being in 12-step “recovery” themselves and a close colleague if not friend of the medical director of the state PHP.

“A body of men holding themselves accountable to nobody ought not to be trusted by anybody.”
― Thomas Paine
“Our minds tell us, and history confirms, that the great threat to freedom is the concentration of power. Government is necessary to preserve our freedom, it is an instrument through which we can exercise our freedom; yet by concentrating power in political hands, it is also a threat to freedom. Even though the men who wield this power initially be of good will and even though they be not corrupted by the power they exercise, the power will both attract and form men of a different stamp.”
—Milton Friedman
Dr. Luis Sanchez, M.D. served as the Medical Director of Physician Health Services, Inc. (PHS) for 15-years. Massachusetts state Physician Health Program (PHP) for 15-years. He retired in March 2013 and Dr. Steven Adelman . Sanchez also served as President of the national organization for state PHPS, the Federation of State Physician Health Programs (FSPHP).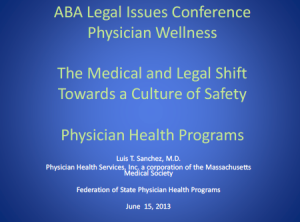
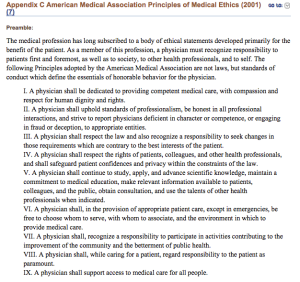
The “PHP-blueprint” is being promoted as a “new paradigm” with a success rate twice that of other treatment programs (80%). With numbers this high, the argument goes, why bother with anything else? The attached slides are from a presentation Sanchez gave at a legal issues conference. His presents the ACGME definition of professionalism that includes competencies in altruism, accountability, excellence, duty, honor and integrity, and respect for others. Sanchez also addressed these topics in an article he wrote for the Journal of the American Medical Association (JAMA) entitled Disruptive Behaviors Among Physicians. In thiis article he discusses a “medical culture of safety” with “clear expectation and standards.” Sanchez affirms the importance of values and codes-of-conduct in the practice of medicine, and calls on physician leaders to “commit to professional behavior.”
PHS Director of Operations Linda R. Bresnahan has also been involved in leadership positions at the FSPHP including acting a Executive Secretary and Interim Executive Director.
PHPs recommend referral of physicians if there are any concerns such as getting behind on medical records. As PHS Associate DirectorJudith Eaton explains “when something so necessary is not getting done, it is prudent to explore what else might be going on.” If the PHP feels that doctor needs an assessment they will send that doctor to a “PHP-approved” facility “experienced in the assessment and treatment of health care professionals.” The physician must comply with any and all recommendations of the assessment center. To assure this the physician must sign a monitoring contract with the PHP (usually five years). USDTL is one of the labs PHPs have contracted with for forensic drug and alcohol testing.
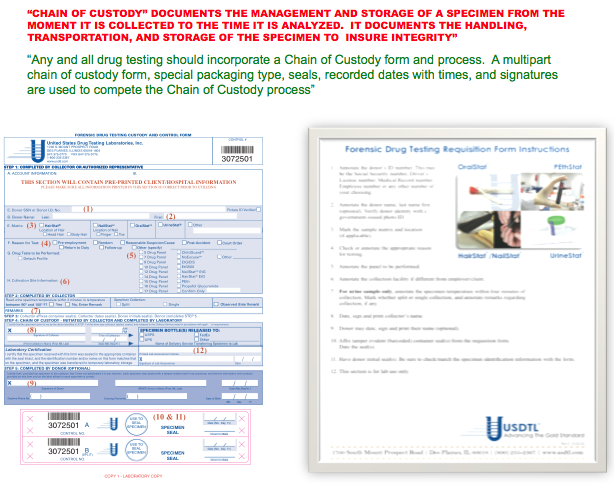
USDTL drug testing laboratory claims to advance the”Gold Standard in Forensic Toxicology.” “Integrity: Results that you can trust, based on solid science” is listed as a corporate value. “Unlike other laboratories, our drug and alcohol testing begins and ends with strict chain of custody.” “When people’s lives are on the line, we don’t skip steps.” Joseph Jones, Vice President of Laboratory Operations explains the importance of chain-of-custody in this USDTL video presentation.
Forensic Drug and Alcohol Tests: The Need For Integrity and Accountability of the Sample
“Forensic” drug-testing differs from “clinical” drug-testing in how the results are used. “Clinical” tests are used for medical purposes in diagnosing and treating a patient.
A “forensic” test is used for non-medical purposes. It is not used for patient care, but for detecting licit and illicit substances in those who should not be using them. Pre-employment and employee assistance and professional monitoring programs are examples.
Forensic testing is held to a higher standards because the consequences of a positive result can be grave and far reaching. A positive forensic test can result in loss of rights of the individual being tested and his or her loved ones. Mistakes are unacceptable.
The Federation of State Medical Boards Policy on Physician Impairment supports this position stating “chain-of-custody forensic testing is critical” (page 14) and the “use of a Medical Review Officer (MRO) for screening samples and confirming sample results” (page 21).
Any and all drug testing requires chain-of-custody. The custody-and-control form is given the status of a legal document because it has the ability to invalidate a test that lacks complete information. Chain-of-custody provides assures specimen integrity. It provides accountability.
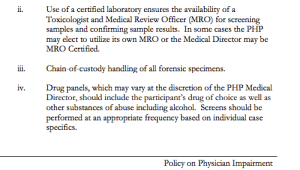 The job of the MRO is to ensure that the drug testing process is followed to the letter and reviews the Custody and Control form for accuracy. The MRO also rules out any other possible explanations for a positive test (such as legitimately prescribed medications). Only then is the test reported as positive.
The job of the MRO is to ensure that the drug testing process is followed to the letter and reviews the Custody and Control form for accuracy. The MRO also rules out any other possible explanations for a positive test (such as legitimately prescribed medications). Only then is the test reported as positive.
The legal issues involved in forensic testing mandate MRO review. According to The Medical Review Officer Manual for Federal Workplace Drug Testing Programs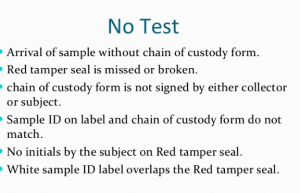
“the sole responsibility of the MRO is to”ensure that his or her involvement in the review and interpretation of results is consistent with the regulations and will be forensically and scientifically supportable.”
“Fatal flaws” such as lack of chain-of-custody form, missing tamper proof seal, missing signatures, or a mismatch of the sample ID and chain of custody ID invalidate the test. It is not reported. Tight chain-of-custody and MRO review is critical for the accountability and integrity of the sample.
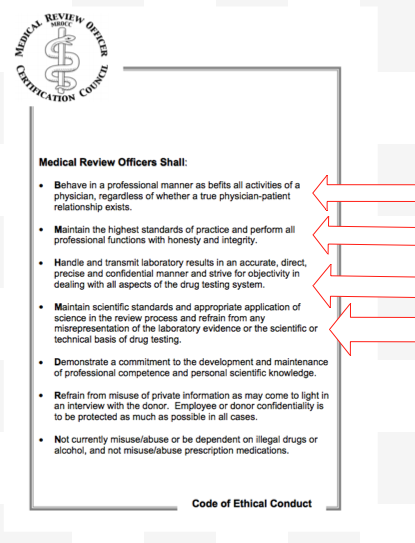
The Medical Review Officer Certification Council provides a certification process for MROs. They also follow their own Code of Ethics. In accordance with these standards PHS has an MRO to review all positive tests. As added assurance the FSPHP guidelines state that all positive tests must be approved by the Medical Director.
also follow their own Code of Ethics. In accordance with these standards PHS has an MRO to review all positive tests. As added assurance the FSPHP guidelines state that all positive tests must be approved by the Medical Director.
Regulation and the Medical Profession–The need for Integrity and Accountability in Physician Leadership and Health Care Policy.
The July 19th, 2011 fax from PHS seen below is in reference to the lab report from USDTL seen above. In it PHS requests the report be “updated”to donor ID number “1310” and to “reflect that the chain of custody was maintained.”
The lab report is a positive test for the alcohol biomarker (Phosphatidyl Ethanol) or PEth, an alcohol biomarker introduced by the Federation of State Physician Health programs and marketed by USDTL and other labs to detect covert alcohol use..
There is no record of where, when or by whom it was collected.
 Both the donor ID # and chain of custody are listed as 461430.
Both the donor ID # and chain of custody are listed as 461430.
The purpose of chain-of-custody is to document the location of a specimen in real time. “Updating” it is not an option. It is prohibited. Updating the “chain of custody to reflect that chain of custody was maintained” is a clear indicator that it was not maintained.
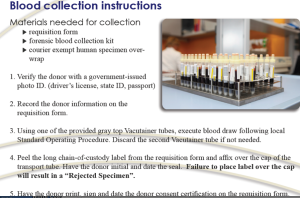
ID #1310 is the unique identifier I was issued by PHS. It is used as a unique identifier, just like a name or social security number, to link me to any sample collected for random drug and alcohol screening. #1310 identifies me as me in the chain-of-custody. On July 1st, 2011 I had a blood test collected at Quest Diagnostics.
The sample was collected at Quest Diagnostics on July 1, 2011 but these documents were not obtained until December 3, 2011 and were included in the “litigation packet” which documents chain-of-custody and is generated on any and all forensic drug testing. It provides proof that the test was done on who it was supposed to have been done and that all required procedure and protocol was followed. It protects the donor form being falsely accused of illicit substance use. In most employee drug-testing programs the litigation-packet is provided on request immediately. It is a transparent process. This is not the case, however, at PHS.
I requested the litigation packet immediately after the positive test was reported on July 19, 2011. PHS first refused, then tried to dissuade me. They finally agreed but warned there would be “unintended consequences. The entire litigation packet can be seen here: Litigation Packet 12:3:2011
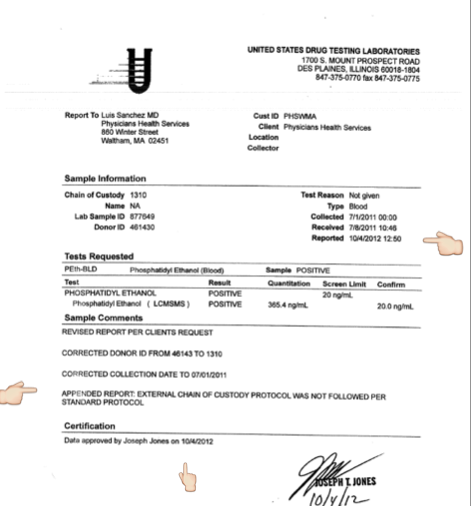
The positive sample has no chain-of-custody linked to me, no date, and no indication where it was collected or who collected it. In addition there was no “external” chain of custody for the sample. The custody-and-control form was missing.
With multiple fatal flaws (6/6) rendering it invalid, USDTL should have rejected it by their own written protocol.
USDTL did not reject it. The document below shows that USDTL added my ID # 1310 and added a collection date of July 1, 2011–the day I submitted the sample.
“REVISED REPORT PER CLIENTS REQUEST”
And in doing so the lab that claims “integrity” and “strict chain of custody” readily, and with no apparent compunction” manufactured a chain-of-custody and added a unique identifier by faxed request.
The litigation packet was signed by Joseph Jones on December 3, 2011. There was no record of where the sample was from July 1st to July 8, 2011. No external chain-of-custody or custody-and-control form was evident in the litigation packet.
The V.P. for Laboratory operations for the lab that claims “strict chain of custody” and that “doesn’t skip steps” “when “peoples lives are on the line” verified a positive test as positive with no custody and control form, no external chain of custody and 6/6 fatal flaws. What is so shocking is that this was done without compunction or pause. As a forensic test ordered by a monitoring program Jones knew full well it would result in significant consequences for someone. He knew that someones “life was on the line,” knew it was wrong, and did it anyway.
A person of conscience would never do this. It is unethical decision making that goes against professional and societal norms. A “moral disengagement” that represents a lack of empathy and a callous disregard for others. I would not consider doing something like this for any price and here it appears to be standard operating procedure.
PHS reported the positive test to the Medical Board on July 19, 2011 Positive PEth July 19, 2011-1. It was used as a stepping-stone to request an evaluation at one of three “PHP-approved” facilities (Marworth, Hazelden and Bradford). The Medical Directors of all three facilities can be seen on this list list called “Like-Minded Docs.” The MRO for PHS, Dr.Wayne Gavryck, whose job was to review the chain-of-custody and validate its integrity before reporting it as positive is also on the list. See this simplified schematic of how it works in Massachusetts. It shows how this is a rigged game.
Expecting to be diagnosed with a non-existent problem and admitted for non-needed treatment I requested an evaluation at a non-12 step facility with no conflicts-of-interest. Both PHS and the Medical Board refused this request in one of four violations of the Establishment Clause of the 1st amendment.
I chose Hazelden. The Medical Director was aware that I had just signed a patent license agreement for an epinephrine auto-injector and he had a child with a peanut allergy. We talked about the device and discussed the problems with current management. I think it was because of this added personal interaction that he did not “tailor my diagnosis” as PHS most certainly requested. Seeing me as a person rather than an object, I believe, enabled his conscience to reject it. My discharge diagnosis found no history of alcohol issues but they could not explain the positive test. Unable to rule out that I drank in violation of my PHS contract they recommended I attend AA.
PHS mandated that I attend 3 12-step meetings per week and requested that I obtain names and phone numbers of fellow attendees so they could contact them to verify my attendance. They also mandated that I discontinue my asthma inhalers (as the propellant contains small amounts of ethanol) that had been controlling my asthma and preventing serious attacks for the previous ten years. I was threatened that if I had to use the inhalers or one day late on the increased payments I would be reported to the Board and lose my license.
Sanchez states that my request for the “litigation packet” was processed on December 5, 2011 (two days after Jones signed off on it) and adds the “testing laboratory is willing to support the test results.”
In the interim I filed a complaint with the College of American Pathologists. I also requested the missing external chain of custody documents from Quest.
I never received the chain of custody from Quest. Instead I received a letter from Nina Tobin, Compliance Manager for Quest documenting all the errors but written to sound as if some sort of protocol was maintained. Tobin claimed the specimen was inadvertently logged as a clinical specimen but sent on to USDTL a week later. (See Quest Letter )
The Chief of Toxicology at MGH wrote a letter to the Board documenting all of the misconduct and irregularities stating that it was an “intentional act” perpetrated by PHS. MLLv3finalJacob_Hafter_Esq_copy.
This letter, as well as the opinions of everyone outside of PHS was ignored. So too were any opinions of my two former Associate Directors at PHS. The e-mail below dated October 10th, 2011 is to to Drs.John Knight and J. Wesley Boyd and I am referring to their article Ethical and Managerial Considerations Regarding State Physician Health Programs that was about to be published. We had hoped that it would draw more attention to the problems with PHPs.
I was subsequently reported as “non-compliant” with AA meetings. They could not give any details of where or when. They then misrepresented a declaration of fact (I stated that I had started going to a specific meeting on a specific date) as an admission of guilt by saying I was referring to a different meeting. 10:23:12 PHS Letter to BORM-noncompliance.
My Chief at MGH, his Chief and others held a conference with PHS and attempted to remove me from PHS and replace the monitoring contract with one of their own. They refused. When confronted with the fabricated test they dismissed it and focused on sending me to Kansas to one of the “disruptive physician” Psikhuskas where they are using polygraphs (despite the AMAs stance that it is junk science) and non-validated neuropsychological instruments that detect “character defects” to pathologize the normal.
I refused. Had I gone to Kansas I would have been given a false diagnosis and my career would be over. This is what they do.
Amy Daniels, the investigator for the College of American Pathologists contacted me in December of 2012 to see how things were going since USDTL “amended” the test. Daniels told me that the College of American Pathologists confirmed my allegations and, as an Accrediting Agency for Forensic Toxicology mandated that USDTL correct it. (Labs can lose accreditation if they do not comply with CAP Standards for Forensic Drug Testing). This was done on October 4, 2012.
PHS denied any knowledge of an amended test. I also wrote an e-mail to Joseph Jones requesting the document but he did not reply.
I contacted CAP. On December 11, 2012 Dr. Luis Sanchez wrote a letter stating “Yesterday, December 10 2012, Physician Health Services (PHS) received a revision to a laboratory test result”
“The amended report indicates that the external chain of custody protocol [for that sample] was not followed per standard protocol]”Sanchez dismisses this test as irrelevant, rationalizing neither PHS nor the Board based any actions on the test and they would “continue to disregard” it.
The logic is that it was my behavior that resulted in any consequences. My “non-compliance” in October led to my suspension and the test had nothing to do with it. The sole reason for reporting me to the Board in 2011 was the positive test. There is no other pretext to use. It is misattribution of blame as without the test, now invalidated, there would have been no AA meetings to say I was non-compliant with.
In response to a civil complaint PHS, Quest and USDTL all took the position that the results of the fraudulent testing had absolutely nothing to do with anything.
And in response to the allegations of forensic fraud the labs claimed there was no forensic fraud because this was not a “Forensic” test but a “clinical” test. The argument was that “clinical” tests do not require chain-of-custody and it was his behavior not these tests that resulted in consequences.
As a “clinical” test I knew it was considered Protected Health Information (PHI) under the HIPAA-Privacy Rule. A patient must give written consent for any outside entities to see it. Obtaining lab tests previously required the consent of both the patient and the ordering provider. What PHS and the labs were apparently unaware of was the changes to the HIPAA-Privacy rule giving patients increased rights to access their PHI. The changes removed the ordering provider requirements. A patient has a right to obtain lab test results directly from the labs and has 30 days to do it. CAP agreed. USDTL sent me all of the documents. They can be seen below:
August 6, 2014 to Langan with health materials.
The documents sent by USDTL are notable for two things:
1. The e-mail from me to Joseph Jones dated December 10, 2012. It can be seen on page 22 of the USDTL documents.
2. USDTL document confirming PHS knew the test was amended 67-days before they said they did.
The document shows PHS and Sanchez were aware of the invalidity of the test on October 4, 2012. Instead of correcting things they initiated machinations to throw me under the bus. They officially reported me to the Board for non-compliance on October 19, 2012.
The December 11, 2012 letter signed by Sanchez states “Yesterday, December 10, 2012, PHS received a “revised report” regarding the test. The documents show he knew about it 67-days prior.
Although USDTL complied with the HIPAA-Privacy Rule and CAP, Quest did not. Quest Diagnostics refused to send me copies of their lab reports claiming it was confidential and protected information that required PHS consent. Quest required I sign a consent form with multiple stipulations regarding PHS. I refused and contacted the Department of Justice -Office of Civil Rights. The DOJ-OCR agreed with me and I received the Quest documents
Remember a “clinical” test can only be ordered by a physician in the course of medical treatment. It requires authorization from the patient to obtain a “clinical” specimen and it requires written authorization as to who sees it. Referring physician was Mary Howard.
And below is the fax from PHS to Quest from July 1, 2011 also requested by Mary Howard. The signature on the front is not mine. In addition I gave the blood at 9:30 and was in my clinic at MGH at 12:23 so it couldn’t be. The WC 461430 R are dated July 2, 2011. This is a “clinical” not “forensic” sticker. The “R” indicates a red top tube. The other sticker is USDTL and indicates it was logged in on July 8, 2011.
What does it all mean? Blood left in a red top tube ferments. This is basic chemistry. The PEth test needs to be refrigerated and shipped overnight to prevent this. In addition it needs to be collected with a non-alcohol wipe in a tube that has an anti-coagulant or preservative so that it does not ferment. It requires strict procedure and protocol.
When I gave my blood on July 1st, 2011 it was as a “forensic” test per my contractual agreement with PHS.
On July 2, 2011 it was changed to “clinical.” Why? because “forensic” protocol would have invalidated it.
The only conceivable reason for doing this was to bypass chain-of-custody procedures. My unique identifier #1310 was removed and the clinical specimen number was used for chain-of-custody. The R in 461430R indicates a red top tube.
By holding on to it for one week the blood fermented. As it was July with an average temperature close to 90 they overshot their mark a bit. My level of 365 is consistent with heavy alcohol use–end stage half-gallon a day type drinking.
Quest then forwarded it to USDTL with specific instructions to process it as a “clinical” sample. USDTL complied and processed it as a clinical specimen which was reported it to PHS on July 14, 2011.
PHS then asked USDTL to add my forensic ID # 1310 and add a collection date of July 1, 2011 so it would appear “forensic” protocol was followed. The reason Jones signed the “litigation packet” on December 3, 2011 was because that was when the “litigation packet” was manufactured. A “clinical” sample does not produce one.
USDTL willingly complied with this request.
PHS then reported this as a “forensic” test to the Medical Board on July 19, 2011 and requested a reevaluation.
The distinction between “forensic” and “clinical” drug and alcohol testing is black and white. PHS is a monitoring program not a treatment provider. The fact that a monitoring agency with an MRO asked the lab to process and report it as a clinical sample and then used it forensically is an extreme outlier in terms of forensic fraud. The fact that they collected it forensically, removed the forensic components and let it sit in a warehouse for a week is abhorrent. The fact they then specifically requested it be processed as a clinical sample deepens the malice. The fact that they then reported it to the Board as a forensic sample and maintained it was forensic up until just recently makes it egregious. But the fact that the test was changed from “positive” to “invalid” on October 4th, 2012 and they then reported me to the Board on October 8th, 2012 for “noncompliance,” suppressed it and tried to send me to Kansas where I would be given a non-existent diagnosis to delegitimize me for damage control makes it wantonly egregious. This is political abuse of psychiatry.
Accountability requires both the provision of information and justification of what was done.
For doctors it is very difficult to obtain the information. As seen here, they put up a gauntlet to prevent the provision of what is immediate in all other drug testing programs. I now have all of the information. What it shows is clear. This was intentional. It was no accident. They knew what they were doing, knew it was wrong but did it anyway.
Accountability also requires that those who commit misconduct suffer consequences. The PHPs have also put up barriers to this. With no regulation or oversight they have no apparent accountability.
My understanding is that it works this way. The Medical Board, Medical Society and Departments of Public Health have no oversight. The MMS has an ethics committee but all they can do is “educate” the person if they feel there was a violation. The DPH won’t even look at it and the Board is complicit.
My understanding is that they have convinced law enforcement that this is a “parochial” issue that is best kept within the medical community. They have also created the impression that they are “friends” of law enforcement. I have heard from many doctors that they have tried to report misconduct, civil rights violations and crimes to the police, AGO, and other law enforcement agencies only to be turned back over to the PHP. By saying the physician is “impaired” it delegitimizes and invalidates the truth. “He’s just a sick doctor, we’ll take care of him.” That physician then suffers consequences effectively silencing the rest.
PHS uses the Board to enforce punitive measures and temporize. The Board puts blind faith in PHS. Blind faith that defies common sense ( mandating phone numbers at anonymous meetings) and disregards the law (Establishment Clause violations that are clear and well established). The Board also temporizes to cause damage.
In my case they required a psychiatric behavioral evaluation. I was given the choice of Kansas and a few other Like-minded assessment centers.
After petitioning for multiple qualified psychiatrists that were summarily rejected months later for no reason one of the Board Attorneys suggested Dr. Patricia Recupero, M.D., J.D. who is Board Certified in Forensic Psychiatry and Addiction Psychiatry. The Board had used her in the past but not recently. Seeing that she had been used by the Board for fit-for-duty evaluations in the past the Board accepted my petition.
Dr. Recupero wrote an 87-page report. She concluded I was safe to practice medicine without supervision, that I had never had an alcohol use, abuse or dependence problem, and that PHS request for phone numbers was inappropriate. She also documented PHS misconduct throughout my contract and concluded it was PHS actions, not mine, that led to my suspension. What she describes is consistent with criminal harassment. She documents the falsification of neuropsychological tests and confirms the forensic fraud. What did the Board do? Ignored their very own recommended and approved evaluator.
One measure of integrity is truthfulness to words and deeds. These people claim professionalism, ethics and integrity. The documents show otherwise. The careers and lives of doctors are in these peoples hands.
Similar fraud is occurring across the country. This is an example of the institutional injustice that is killing physicians. Finding themselves entrapped with no way out, helpless and hopeless they are feeling themselves bereft of any shade of justice and killing themselves. These are nothing more than bullies and accountability is essential. The “disruptive physician” moral panic has harmed the Medical Profession.
Dr. Clive Body in his book Corporate Psychopaths writes that “Unethical leaders create unethical followers, which in turn create unethical companies and society suffers as a result.” And according to Dr. Robert Hare in Without Conscience “If we can’t spot them, we are doomed to be their victims, both as individuals and as a society. ”
Wes Boyd notes that valid complaints from physicians are often dismissed as “bellyaching” by the PHPs. Complacent that these are just good guys helping doctors and protecting the public the complaints are dismissed, tabled, deflected or otherwise ignored. Bellyaching?? Is this bellyaching.
It is my opinion that what you see here is indefensible Procedurally, Ethically, and Legally.
Procedurally it goes beyond negligence and represents fraud. It violates every procedural guideline, regulation and standard of care including their very own.
Ethically it violates everything from the Hippocratic Oath to AMA Medical Ethics to the MRO Code of Conduct.
And where was PHS MRO Wayne Gavryck? By my count he violated at least 4 of the 6 Codes of Ethical Conduct.
What was done here violates the most fundamental ethical principles of Medicine -Autonomy, Beneficence, Nonmaleficence and justice.
Intentionally falsifying a laboratory or diagnostic test to refer for an evaluation or support a diagnosis or give unwarranted “treatment” is unconscionable. Abuse under the utility of medical coloration is especially egregious.
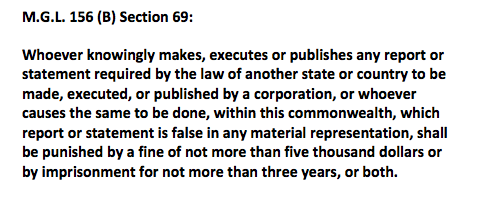
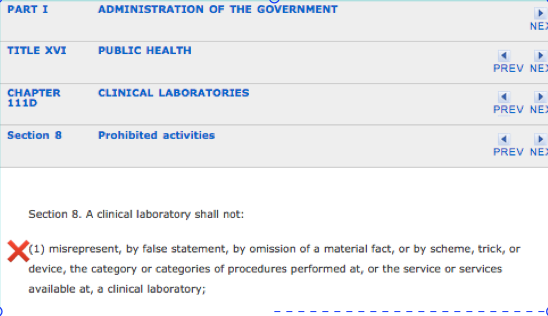
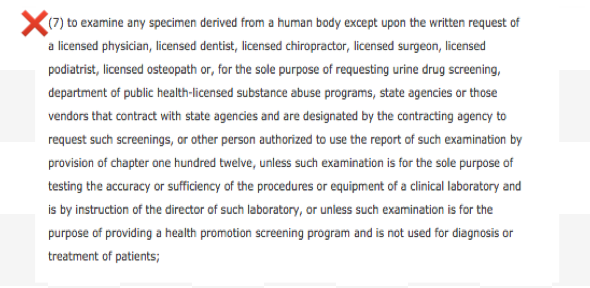
The information provided herein should negate any “peer-review” protection or immunity afforded PHS as it is undeniably and egregiously in “bad faith.” Moreover, the ordering a “clinical” test is outside PHS scope, practice, and function of PHS. According to M.G.L. c. 111, § 203 (c):
An individual or institution, including a licensed or public hospital, physician credentialing verification service operated by a society or organization of medical professionals for the purpose of providing credentialing information to health care entities, or licensed nursing home reporting, providing information, opinion, counsel or services to a medical peer review committee, or participation in the procedures required by this section, shall not be liable in a suit for damages by reason of having furnished such information, opinion, counsel or services or by reason of such participation, provided, that such individual or institution acted in good faith and with a reasonable belief that said actions were warranted in connection with or in furtherance of the function of said committee or the procedures required by this section.
Dr. Luis Sanchez and Dr. Wayne Gavryck need to be held to the same professional standards as the rest of us.
If you can support either of them procedurally, ethically, or legally, any one of them, then I will turn in my medical license with a bow on it. If they did not commit negligent fraud by standards of care and procedural guidelines, egregious moral disengagement in violation of ALL ethical codes for the medical profession and society and break the law then disprove me. Just one will do.
But you can’t do this then I ask that you speak up and take a stand. Either defend them or help me hold them accountable. If a crime is committed it needs to be addressed. Ignoring encourages more of the same.
And if this cannot be supported procedurally, ethically or legally then I want to know what is going to be done about it?
How low does the moral compass have to go before someone takes action?
Doctors are dying across the country because of people just like this. They have set up a scaffold that removes the usual checks and balances and removed accountability. It is this institutional justice that is driving many doctors to suicide.
So the evidence is above. Either defend them or help me draw unwanted attention to this culture of bullying and abuse. So I am asking you to contemplate if what you see here is ethically, procedurally or legally sound. If you can show just one of these then I stand corrected. But if you cannot justify this on any level then I want you to help me expose this criminal enterprise. Either defend it or fight it. Silence and obfuscation are not acceptable.
How your Employee Assistance Program (EAP) is at Risk for Fraud and Abuse: What you need to know about the “PHP-Blueprint” and “New Paradigm”
 Employee Assistance Programs (EAPs)
Employee Assistance Programs (EAPs)
Employee assistance programs (EAPs) evolved from the “industrial” or “occupational” alcohol programs (OAPs) of the 1940s that were developed by companies to address alcohol abuse and its impact on the workplace. The first of these programs was developed by Dupont de Nemours and Company from 1941-1944 followed by Kodak in 1945 (Royce and Scratchley, 1989). These programs were typically staffed by a recovering alcoholic employee working in cooperation with corporate medical departments or a union health clinic and the sole referral source was to the recently formed self-help group Alcoholics Anonymous (AA). The primary intervention was to “confront the alcoholic’s job performance decline and denial using possible job loss as leverage toward seeking help.”
 With time these programs broadened to include other issues that could potentially impact job performance. Worker Assistance Programs (WAPs) emerged in the 1950s when companies such as Consolidated Edison, Standard Oil of New Jersey, and American Cyanamid extended their alcoholism programs to also address mental health issues in their employees (Roman, 1981; Steele, 1995).
With time these programs broadened to include other issues that could potentially impact job performance. Worker Assistance Programs (WAPs) emerged in the 1950s when companies such as Consolidated Edison, Standard Oil of New Jersey, and American Cyanamid extended their alcoholism programs to also address mental health issues in their employees (Roman, 1981; Steele, 1995).
In the 1970s EAP-related legislation was passed and this markedly increased the number of these workplace programs. The Hughes Act ( Public Law 91-616 ) established the National Institute of Alcohol Abuse and Alcoholism (NIAAA) as part of the United States Department of Health and Human Services (USDHHS) and these organizations subsequently developed guidelines applicable to both the public and private sectors. Public Law 92-255 mandated their existence at all federal agencies and military institutions and in 1972 the Hughes Act was amended to also include drug abuse (Public Law 92-255 ). The amendment also required USDHHS Guidelines serve as the model for all federal programs. On September 15, 1986 President Ronald Reagan signed Executive Order 12564 stating a desired goal of achieving a Drug-Free Federal Workplace. This use of drug testing by governmental agencies then led to an increase in drug-testing by private employers and by 1986 more than a quarter of Fortune 500 companies were drug-testing job applicants
 Another significant development was the formation of private EAP firms that began to offer EAP services and drug-testing via contracts with employers. One such example is Bensinger, DuPont & Associates (BDA) which was founded in 1982 by former DEA Chief Peter Bensinger and National Institute on Drug Abuse (NIDA) founding director Robert Dupont. BDA became the sixth largest employee assistance program (EAP) provider in the United States and provided workplace drug testing and other services to some 10-million employees of companies such as Kraft Foods, American Airlines, Johnson & Johnson and the Federal Aviation Administration (FAA). On December 1, 2015 Bensinger, DuPont & Associates was acquired by the Canadian firm of Mourneau Sheppel which employs 4000 plus individuals and has approximately 20,000 clients ranging from small businesses to some of the largest corporations in North America.
Another significant development was the formation of private EAP firms that began to offer EAP services and drug-testing via contracts with employers. One such example is Bensinger, DuPont & Associates (BDA) which was founded in 1982 by former DEA Chief Peter Bensinger and National Institute on Drug Abuse (NIDA) founding director Robert Dupont. BDA became the sixth largest employee assistance program (EAP) provider in the United States and provided workplace drug testing and other services to some 10-million employees of companies such as Kraft Foods, American Airlines, Johnson & Johnson and the Federal Aviation Administration (FAA). On December 1, 2015 Bensinger, DuPont & Associates was acquired by the Canadian firm of Mourneau Sheppel which employs 4000 plus individuals and has approximately 20,000 clients ranging from small businesses to some of the largest corporations in North America.
The company now known as BDA Moreau Sheppel represents the largest employee assistance program (EAP) provider in the entire world.

Ethical Considerations in Workplace Drug-Testing and EAP Management
EAPs can be managed internally by staff employees of a company or organization who contract with outside vendors for drug-testing or externally by an EAP provider such as BDA Moreau Sheppel. The primary goal is to address an employees problem (such as a substance abuse or mental health issue) before that given problem impacts job performance. In this way EAPs are viewed as mutually beneficial; they provide timely help to an employee experiencing a problem in addressing that problem and at the same time potentially avert absenteeism, poor work performance, accidents and termination of a valuable employee. They are designed to help both the employee and the employer in a “win-win” situation. The goals, therefore, should be identical. The goals should be convergent.
Although many of these programs offer mental health counseling and other such services, the core function of EAPs does not include diagnosis or treatment but to facilitate and ascertain diagnosis and treatment. Those referred to EAPs (either through self-referral or by someone else) are assessed and referred to outside sources, either individual practitioners or institutional agencies, that have expertise and experience in assessing and diagnosing the presenting problem. It is the EAP’s function to oversee and make sure that the presenting problem is not only properly assessed, addressed, diagnosed and treated (if indicated) but that the presenting problem remains managed and under control. This requires a period of monitoring or oversight to provide reassurance; progress reports from supervisors, compliance reports from treatment providers, and periodic drug and alcohol testing (if the problem involved substance use) are all part and parcel of a typical EAP.
EAPs have two primary business relationships: 1) a network of individuals and/or programs to which they refer individuals for assessment and treatment, and 2) laboratories capable of performing drug and alcohol testing. The integrity of an EAP is therefore dependent on the integrity and quality of its referral sources and laboratory operations. Those assessing, testing and treating must have education, experience and expertise in assessing, testing and treating the problems presented to them. They must be valid and reliable and it goes without saying that any and all assessment, testing and treatment must be objective, honest and without any conflicts-of-interest.
 This topic is addressed in the book Employee Assistance Programs: What Works and what Doesn’t by Lawrence Mannion in which he discusses the notion of “control” in the context of managed mental health care. For those wishing to control any direction, entity or circumstances pertaining to these types of services Mannion states:
This topic is addressed in the book Employee Assistance Programs: What Works and what Doesn’t by Lawrence Mannion in which he discusses the notion of “control” in the context of managed mental health care. For those wishing to control any direction, entity or circumstances pertaining to these types of services Mannion states:
“..if the ends or purposes of those doing the controlling are in accord with the ends or purposes intrinsic or inherent in the thing being managed there is no conflict.”(page 133).
A 2001 study that looked at EAP professionals perceptions of ethical issues related to their business practices found that 22% of those surveyed identified “referrals” and “ownership structures” as among the most important and critical ethical issues facing the industry (Sharar, White, and Funk, 2001). Many of the respondents expressed concerns that the organizations owning and operating EAPs expected them to generate treatment revenue via a pattern of preferential referral to specific programs or practitioners and were concerned that this financial conflict-of-interest undermined the fundamental obligation of providing “neutral” and “objective” assessments to individuals with problems. To prevent the appearance of unethical conduct the recommendation below were made.
-Fully disclosing (to both employer and client) any affiliations with proposed referral options;
.-Offering an “objective” presentation of more than one referral option to the client;
-Providing clinical justification that the referral is in the best interests of the client;
-Refusing to accept any direct gain or financial remuneration for referring clients;
-Instituting a peer review program to monitor and evaluate the quality and appropriateness of referrals; and
-Developing a utilization/service summary report for employers containing detailed information on patterns of referral for continuing care and treatment.
In 1998 the American Medical Associations Council on Ethical Affairs suggested that incentive programs should be based on quality (rather than quantity) of services or referrals and that linking financial incentives to individual treatment decisions should be avoided (AMA, 1988). In summary any and all referrals need to be objective, honest and fair. They need to be reliable and valid. So too does any and all drug-testing. Most employee drug-testing follows a standardized protocol. Although errors do occur, the procedures followed by the vast majority of employee assistance program providers aim to minimize error. Most programs were implemented and evolved in collaboration with unions or other groups working on behalf of the best interests of the employee.
When drug testing initially entered the workplace many issues had to be worked out. Those in favor of drug-testing insisted that they had the right to demand a drug-free workplace and pointed to decreased productivity, increased accidents and absenteeism as potential consequences of drug abuse. Opponents challenged the constitutionality and reliability of drug-testing and also emphasized the necessity of distinguishing work life from private life. If a person smoked a joint on the weekend, they reasoned, it is no concern of management so long as they performed competently come Monday. Many in the medical community dismissed mandatory drug testing at the time as “chemical McCarthyism.” Nevertheless, drug-testing for better or for worse did enter the workplace. Most of these programs were implemented with the oversight and collaboration of unions or some other group advocating for the rights and interests of those being tested. Procedures and protocols were discussed, deliberated and had to be agreed on before implementation. In his 1984 book Designing Employee Assistance Programs, David Masi emphasizes the need for the close involvement of unions in workplace drug-testing and other EAP services in order to “protect employee rights”as well as the employers responsibilities in doing so (Masi, 1984). Most programs simply followed the already established Federal Workplace Drug Testing Guidelines and this is still the case for most EAPs today. The Mandatory Guidelines for Federal Workplace Drug-Testing Programs provide strict procedure and protocols specifically designed to protect the rights of those being tested. The Department of Transportation (DOT), United States Nuclear Regulatory Commission, and many other safety-sensitive organizations follow these stringent guidelines which include only using certified labs, strict chain-of-custody procedures and Medical Review Officer (MRO) assessment of all positive tests to rule out alternative explanations or “innocent-positives” (such as a prescribed drug). It is also the job of the MRO to verify that strict chain-of-custody was maintained from the collection of the sample to its final analysis. Additionally, only FDA approved drug-testing methods are utilized. This strict protocol assures a high level of validity and reliability (although mistakes can and do occur) to reduce the risk of someone being falsely labeled as a drug or alcohol user. False-positive-tests are absolutely unacceptable as the results of a positive drug-test can be grave, far-reaching and sometimes even permanent.

Physician Health Programs (PHPs)
Physician health programs (PHPs) are basically just employee assistance programs (EAPs) for doctors. They evolved from 1970’s “impaired physicians programs” much like EAPs evolved from the occupational alcohol programs (OAPs) of the 1940s. These programs were designed to both help sick doctors and protect the public in the same manner EAPs were designed to help sick employees and protect a company. The mechanics and mentality should be exactly the same. If the PHP feels a doctor is in need of an assessment he or she is then referred to an outside facility for evaluation (and treatment if that is indicated and in this system “treatment” is virtually guaranteed. The PHP then monitors the doctor for a period of time (typically five-years) to make sure that the problem remains under control. Monitoring inevitably includes at least weekly abstinence based substance abuse testing (including alcohol) using non-FDA approved laboratory developed tests (LDTs) no matter what the presenting problem. As with EAPs, one can self-refer to these programs or be referred by someone else and the latter can be done anonymously and with guaranteed confidentiality for the referrer.
In the context of PHPs being EAPs for doctors, the Federation of State Physician Health Programs (FSPHP) functions in the same manner as an EAP provider. The FSPHP s a non-profit corporation formed in 1990 to promote best-practices in state PHPs and influence policy. This EAP for doctors is being called the “PHP-blueprint”.
Although this model of EAP management is currently just being used on doctors, nurses, and other health care professionals; parts of the criminal justice system; and some areas of the airline industry, the grand plan is to move this model of care to other populations. Moving the “PHP-blueprint” to other occupations and populations is what is being deemed the “New Paradigm.”
The “PHP-blueprint” and the “New Paradigm”
The American Society of Addiction Medicine (ASAM) White Paper on Drug Testing describes the current practice of drug-testing in various contexts and explains how physicians and other healthcare providers can “use drug-testing to discourage non-medical drug use and ‘diversion’ of controlled substances” to “encourage appropriate entry into addiction treatment,” identify relapse and “improve outcomes of addiction treatment” through the use of “long-term post treatment monitoring.” The paper proposes random mandatory drug-testing by medical professionals (pediatricians to obstetricians to geriatricians) using not only urine but blood, oral fluid (saliva), hair, nails, sweat and breath.”
 The White Paper’s writing Committee Chair, Dr. Robert Dupont, described this “New Paradigm” in his keynote speech before the Drug and Alcohol Testing Industry Association (DATIA) in 2012 and claimed this model “sets the standard for effective use of drug testing” (Dupont, Drug Testing and the Future of American Drug Policy 2012) Dupont then proposed the “PHP-blueprint” be expanded to other workplace populations, healthcare students and schools. His audience, the Drug and Alcohol Testing Industry Association (DATIA) represents more than 1,200 companies involved in the drug and alcohol testing industry for profit and even employs their own DC-based lobbying firm, Washington Policy Associates.
The White Paper’s writing Committee Chair, Dr. Robert Dupont, described this “New Paradigm” in his keynote speech before the Drug and Alcohol Testing Industry Association (DATIA) in 2012 and claimed this model “sets the standard for effective use of drug testing” (Dupont, Drug Testing and the Future of American Drug Policy 2012) Dupont then proposed the “PHP-blueprint” be expanded to other workplace populations, healthcare students and schools. His audience, the Drug and Alcohol Testing Industry Association (DATIA) represents more than 1,200 companies involved in the drug and alcohol testing industry for profit and even employs their own DC-based lobbying firm, Washington Policy Associates.
In a 2012 article entitled “Six lessons from state physician health programs to promote long-term recovery” Dupont and co-author Dr. Greg Skipper describe the need to”reach more of the 1.5 million Americans who annually enter substance abuse treatment stating that:
“This model of care management for substance use disorders has been pioneered by a small and innovative group of the nation’s physicians in their determination to help other physicians save their careers and families while also protecting their patients from the harmful consequences of continued substance abuse. In fulfilling the professional admonition “physician: first heal thyself,” these physicians have created a model with wide applicability and great promise.” (Dupont, R., Skipper, G. 2012)
 These six lessons are:
These six lessons are:
(1) zero tolerance for any use of alcohol and other drugs;
(2) thorough evaluation and patient-focused care;
(3) prolonged, frequent random testing for both alcohol and other drugs;
(4) effective use of leverage;
(5) defining and managing relapses; and
(6) the goal of lifelong recovery rooted in the 12-Step fellowships.
 The “PHP-blueprint” is being promoted as “Gold standard” and a “New Paradigm” of recovery. In other words it is being proposed that the model of care management currently being used on doctors and managed by the FSPHP replace your current EAP. And like a faulty smoke-detector or a misfired Epipen you won’t realize or possibly even care about it until it happens.
The “PHP-blueprint” is being promoted as “Gold standard” and a “New Paradigm” of recovery. In other words it is being proposed that the model of care management currently being used on doctors and managed by the FSPHP replace your current EAP. And like a faulty smoke-detector or a misfired Epipen you won’t realize or possibly even care about it until it happens.
The question for us, then, is this:
Are the ends or purposes of those managing physician health programs the same as or in accordance with those being managed by these programs?
Moreover, will the ends and purposes of the physician health model of care be in accordance with the ends and purposes of those who will potentially be managed by this model of care in the “New Paradigm?
The answer to the first question is a resounding “NO.” Complaints of coercion, abuse and other misconduct and fraud are rampant. Doctors are, in fact, being diagnosed with substance use disorder and other problems when they do not meet the diagnostic criteria for substance use disorder or other problems and being forced into unnecessary and unneeded treatment while those who do have substance use disorders and mental illness are being provided cookie-cutter treatment that is often inappropriate and inadequate treatment. Why? The money of course. Do the homework and follow the money.
It is necessary that we conform our thinking and behavior to objective reality rather than an illusion and the version of the physician health model being put forth by those promoting the “PHP-blueprint” and the “New Paradigm”is at marked variance to those being managed by the model and for further reading start with the following:
- British Medical Journal feature “Physician health programs under fire” by Jeanne Lenzer
- The “PHP-Blueprint”–A Trojan Horse for Profit and Wider Social Control: Watching helplessly, as Cassandra did, while the soldiers emerge and wreak their predicted havoc.
- “New Paradigm” is a business model not a medical model
- Physician Suicide and “Physician Wellness” –Time to start talking about the elephant in the room!
In Employee Assistance Programs: What Works and what Doesn’t, Mannion states:
“We need to spend less time making hyperbolic statements about change and entertaining grandiose ideas about strategic alliances and more time developing criteria or standards to determine what does and what does not belong under the canopy of employee assistance. More specifically what is that principle or principles on the basis of which we can develop a criterion or criteria to determine those activities that could legitimately come under the heading of employee assistance?” (page 165-166)
.
REFERENCES
American Medical Association, Council on Ethical and Judicial Affairs. Reports on Ethics in ManagedCare.Chicago, Ill.: American Medical Association Press, 1998
Dupont, R and G. Skipper “Six Lessons from State Physician Health Programs to Promote Long Term Recovery” Journal of Psychoactive Drugs 44 (1) 2012 (72-78)
Dupont, R. “Drug Testing and the Future of American Drug Policy” Presentation at the DATIA Annual Conference. San Antonio, Texas. April 19, 2012.
Jett K. Employee Assistance Programs–Government’s Role in an Expanding Field. In: Mecca AM, ed. Prevention 2000–A Public/Private Partnership: CHRF:69-81.
Manion, L. “Employee Assistance Programs: What Works and What Doesn’t” Praeger, Westport, CT. 2004
Massi, D. Designing Employee Assistance Programs. American Management Associations, New York, NY 1984
Roman P. From Employee Alcoholism to Employee Assistance. Journal of studies on alcohol. 1981;42(3):244-272.
Royce JE, Scratchley D. Alcoholism and Other Drug Problems: A Revised Edition of Alcohol Problems and Alcoholism. New York, NY: Simon & Schuster, Inc.; 1989.
Sharar D, W White, and R. Funk. “Business ethics and employee assistance/managed behavioral healthcare: A national survey of issues and challenges.” Journal of Behavioral Health Services and Research (submitted for peer review and publication April 2001).
Sharar, D., and W. White “Referrals and Ownership Structures: The first of two articles on the need for a revised ethic in employee assistance considers whether ownership structures can improperly influence EAP professionals.”
Steele P, Trice H. A History of Job Based Alcoholism Programs: 1955-1972. Journal of Drug Issues. 1995;19:511-532.
The New Paradigm for Recovery Making Recovery-and Not Relapse-the Expected Outcome of Addiction Treatment. Washington, D.C. March 2014 2014.
Making some serious gains. Let’s not lose the momentum. Please donate to my Gofundme here


The impact of illegitimate authority on regulation of the medical profession: The overdue need for critical analsysis
It is not wisdom but Authority that makes a law—Thomas Hobbes
In Questions of science, the authority of a thousand is not worth the humble reasoning of a single individual— Galileo Galilei
Regulatory Decisions and Public Policy
Making sound decisions about regulation calls for an understanding of the problem it is intended to solve. Legitimate policy must be based on recognized institutions and experts. Regulatory changes demand methodologically sound science and evidence-based facts arrived at through rigorous peer review and professional oversight. The science must be reliable and unbiased. Legitimate policy must be based on legitimate institutions and expert authority grounded in wisdom. Authoritative opinion needs to be assembled with facts and best available evidence guided by science and critical reasoning to best solve a particular problem and benefit the greater good.
If the information regulatory agencies rely on to make regulatory decisions and public policy is unreliable then bad decisions, wrong decisions and flawed public policy are inevitable. Consequences can be far-reaching and grave.
The impact of the close alliance between state medical boards and their state physician health programs (PHPs) and their national organizations on this failure to achieve the public goals with which they have been tasked has not been considered. It needs to be as the consequences of relying on this illegitimate and irrational authority have indeed been far-reaching and grave. Some of the nonsense pushed forth by the PHP movement and given “regulatory sanctification” by state medical boards is beyond belief. It would be comical if the results were not so tragic.
State Medical Boards
A physician’s right to practice medicine is granted by the state medical board in the form of a medical license. Each state has a medical practice act that defines the practice of medicine and used to regulate the medical profession. The medical board is empowered to identify and take action against doctors for substandard care, unprofessional behavior and other violations as defined by the state medical practice act. Given that medical boards are state agencies, their authority is subject to traditional constitutional constraints including equal protection and procedural due process limitations.
State Medical Boards have faced criticisms for being lax in their duty to protect the public from dangerous doctors.1,2 A recent study in the New England Journal of Medicine found that just 1% of physicians accounted for 32% of paid malpractice claims.3 One physician had at least 31 malpractice totaling more than $10 million in damages and nine of those payments were related to “failure to use proper aseptic technique” while another had at least 21 malpractice payments including eight improperly performed surgeries, three unnecessary surgeries and two surgeries on the wrong body part. Neither of these doctors faced disciplinary action from their state medical board.
Failing to recognize the germ theory by failing to meet even the most basic standards of cleanliness and wrong-side surgery are egregious. The fact that these are not isolated one-offs but repeat offenders is reprehensible. There is clearly something wrong with a system that allows such unfettered idiocy to flourish.
On the other hand there are increasing reports of excellent doctors with no history of malpractice or patient harm losing their licenses after one-offs, minor infractions or nothing at all.
The public’s goals would be better served if boards exercised their discretion against physicians who violate the most basic standards of professionalism and competency. They are failing to achieve this task.
The Federation of State Medical Boards (FSMB)
The Federation of State Medical Boards (FSMB) is a national not-for profit organization that gives guidance to state medical boards through public policy development and recommendations on issues pertinent to medical regulation.
Shortly after its founding in 1912, the Federation of State Medical Boards began publishing a quarterly journal addressing issues relating to medical licensing and regulation of doctors. First published in 1913 as the Quarterly of the Federation of State Boards of the United States, the publication has undergone several name changes and publication schedules. The archival organization and availability of full articles published sequentially over the past century is historically invaluable as it provides not only the regulatory by the national organization involved in the medical licensing and regulation of doctors and this archival organization facilitates an unskewed and impartial examination in its historical context. A focus on sound decision-making can be seen in the regulatory and legal medicine literature up until the 1990s.
For example when drug-testing was first introduced questions of validity became a genuine topic of concern.
By the late 1980s almost every state medical board was utilizing random drug and alcohol testing. Noting that “not all testing methods and results are created equal,” South Carolina State Board of Medical Examiners executive director Stephen S. Seeling, J.D. addressed the critical importance of accuracy and reliability in the Federation Bulletin in 1988 and cautioned that “if boards wish to be able to use positive results of drug screens in administrative or legal proceedings, great care must be taken to insure that the results are accurate, reliable and thus legally probative.” 4 Suggesting that board members and board attorneys be familiar with specific testing methodologies Seeling concludes that:
Random drug testing is an important tool for every board in its mission to protect the public and maintain the integrity of the medical profession. Careful attention however must be given to this process to insure the reliability and legal defensibility of testing results. Failure to do so could diminish the board’s credibility in the eyes of the profession and the public, and expose the board to potentially serious legal challenges.”4
This sound decision-making unfortunately took a nasty left turn in 1995. In that year the Federation of State Physician Health Programs (FSPHP) forged a relationship with the Federation of State Medical Boards. They have been going strong ever since.
1995 FSPHP/FSMB Alliance
The Sick Physician: Impairment by Psychiatric Disorders, Including Alcoholism and Drug Dependence, published in JAMA in 1973,5 recommended that state medical societies establish programs to identify and treat “impaired physicians” which the AMA defined as “a physician who is unable to practice medicine with reasonable skill and safety to patients because of mental illness or excessive use or abuse of drugs, including alcohol.”
Physician Health Programs (PHPs) were subsequently developed to assist with the goal of rehabilitating and monitoring doctors as an alternative to disciplinary action by state medical boards. Preferring rehabilitation to probation or license revocation so long as the public was protected from imminent danger, most medical boards accepted the concept with support and referrals.
PHPs existed in almost ever state by 1980. Often staffed by volunteer physicians and funded by the state medical society, these programs served the dual purpose of helping sick doctors and protecting the public. As an alternative to disciplinary action these programs advocated for physicians who developed illness, assured they got proper treatment and provided monitoring to assure they remained healthy. The mechanics and mentality of PHPs were initially quite variable.
The model used today came out of the “impaired physician movement,” which according to British sociologist G. V. Stimson is “characterized by a number of evangelical recovered alcoholic and addict physicians, whose recovery has been accompanied by an involvement in medical society and treatment programs. Their ability to make authoritative pronouncements on physician impairment is based on their own claim to insider’s knowledge.”6
In 1987, the Atlanta Journal and Constitution ran a series of reports after five patients in the “Impaired Professionals” program at Ridgeview Institute created by G. Douglas Talbott in Atlanta killed themselves7 and least 20 more died by suicide after leaving Ridgeview.8 It was reported doctors were coerced into Ridgeview and then threatened and bullied to comply with any and all demands under threat of loss of licensure. All patients were indoctrinated into A.A. and forced to confess they were alcoholics or addicts or threatened with expulsion and with not being certified or advocated for with their Medical Boards.
A “recovering” alcoholic and addict who had previously been a successful cardiologist Talbott created the DeKalb County Impaired Physicians Committee for the Medical Association of Georgia in 1975 and subsequently founded the Georgia Disabled Doctors Program for the assessment and treatment of physicians, in part because “traditional one-month treatment programs are inadequate for disabled doctors.” He created the “Impaired Professionals” program at Ridgeview to provide this specialized treatment. The Constitution reported that doctors entered the program under “threats of loss of licensure even when they would prefer treatment that is cheaper and closer to home,” 9 because Ridgeview “enjoys unparalleled connections with many local and state medical societies that work with troubled doctors,” and “licensing boards often seek recommendations from such groups in devising an approved treatment plan”
 The Constitution reported that those in charge of the program are often “physicians who themselves have successfully completed Ridgeview’s program.”9 The impaired physician movement emphasizes disease and therapy, rather than discipline and punishment. They believe that alcoholism and addiction is a chronic relapsing brain disease requiring lifelong abstinence and 12-step spiritual recovery. The drug or alcohol abuser or addict is a person lacking adequate internal controls over his behavior and for his own protection as well as the protection of society external restraints are required including involuntary treatment.
The Constitution reported that those in charge of the program are often “physicians who themselves have successfully completed Ridgeview’s program.”9 The impaired physician movement emphasizes disease and therapy, rather than discipline and punishment. They believe that alcoholism and addiction is a chronic relapsing brain disease requiring lifelong abstinence and 12-step spiritual recovery. The drug or alcohol abuser or addict is a person lacking adequate internal controls over his behavior and for his own protection as well as the protection of society external restraints are required including involuntary treatment.
“Contingency-management,” or systematic use of reinforcement is a type of treatment used in the mental health field in which patient’s behaviors are rewarded (or less often punished). It has successfully been used in substance abuse treatment by using prizes or vouchers for positive reinforcement by, for example giving prizes or vouchers for negative drug screens or following up for an appointment.10,11. At Ridgeview, a doctor’s medical license was being used as the leverage. This is not contingency management. It is extortion.
Many addiction professionals were highly critical of Talbott’s methods, including LeClair Bissell.7 and Assistant Surgeon General John C. Duffy who said that Ridgeview suffered from a “boot-camp mentality” toward physicians under their care.”8 “”
Talbott justified this length of stay because he claimed doctors were unique because of what he calls the “four-MDs,” ”M-Deity”, “Massive Denial” “Militant Defensiveness” and “More Drugs.”12
 The cost of a 28 day program at Ridgeview was $10,000 but far more for the thrice lengthy stay required by healthcare professionals..8 I would say the impetus behind this is due to just “two-MDs,” “Medical License,” and “More Money.”
The cost of a 28 day program at Ridgeview was $10,000 but far more for the thrice lengthy stay required by healthcare professionals..8 I would say the impetus behind this is due to just “two-MDs,” “Medical License,” and “More Money.”
A jury awarded $1.3 million to the widow of one of the deceased physicians against Ridgeview,13 and other lawsuits initiated on behalf of suicides were settled out of court, but nothing else has changed.14
These suicides did not generate any reaction from the medical community at large and any doctor referred by a PHP for an assessment today will spend at least 3 months in treatment. ” It is inevitable. The Dicto simpliciter argument of “terminal uniqueness” has been cemented as in 1995 this PHP model won the lottery. A 1995 issue of The Federal Bulletin: The Journal of Medical Licensure and Discipline, published by the Federation of State Medical Boards, contains articles outlining PHP programs in 8 separate states. Although these articles were little more than descriptive promotional pieces written by state PHP program directors with no described study-design or methodology the journals Editor proclaimed “the success rate of the programs and others like them approach 90%.” 15 and “cooperation and communication between the medical boards and the physician health programs must occur in an effort to protect the public while assisting impaired physicians in their recovery.” 15 The 8 state PHPs were all based on Talbott’s methodology.
 Nonsense such as the “four-MDs” and thrice lengthy treatment has been accepted without scrutiny. Logical fallacy is written as science. For example Merlo and Gold use the “appeal to consequences” logical fallacy to justify the extended length of stay stating that “physicians with a substance use disorder are not typical of addicts in general, it is not useful to apply standard professional guidelines… Rather, because of the public health consequences of relapse, most physicians who are addicted are treated more aggressively and for longer periods” than non-physicians.
Nonsense such as the “four-MDs” and thrice lengthy treatment has been accepted without scrutiny. Logical fallacy is written as science. For example Merlo and Gold use the “appeal to consequences” logical fallacy to justify the extended length of stay stating that “physicians with a substance use disorder are not typical of addicts in general, it is not useful to apply standard professional guidelines… Rather, because of the public health consequences of relapse, most physicians who are addicted are treated more aggressively and for longer periods” than non-physicians.
According to Merlo and Gold “Physicians will lobby for a level of care that minimizes the disruption of their daily life. However, it is generally not advisable to grant the physician’s request for treatment in the least restrictive environment, but rather to maximize the treatment dose and duration to improve effectiveness and reduce the likelihood of relapse and further damage to health, family, and the ability to practice. Depending on the response to treatment, physicians typically undergo 3 to 6 months of intensive treatment in a structured program and 5 years of urine testing with controlled, contingency-managed outpatient follow-up.16 This gibberish has no basis in reality. It is made up out of whole cloth. No evidence-base exists and it is propaganda based fear that defies not only reason but common sense.
“Potentially Impairing Illness” “Relapse Without Use” “Dumb and Dumber”
The Federation of State Medical Boards House of Delegates adopted an updated Policy on Physician Impairment at their 2011 annual meeting approved the concept of “potentially impairing illness.”
According to the Federation of State Physician Health Programs …”physician illness and impairment exist on a continuum with illness typically predating impairment, often by many years. This is a critically important distinction. Illness is the existence of a disease. Impairment is a functional classification and implies the inability of the person affected by disease to perform specific activities.”
 “Process addiction” was added as a potentially impairing illness including compulsive gambling, compulsive spending, compulsive video gaming, and “workaholism.” According to the FSPHP “the presence of a process addiction can be problematic or even impairing in itself, and it can contribute to relapse of a physician in recovery. As such, process addictions should be identified and treated.” They define three levels of relapse. “Relapse without use” is a 12-step concept. G. Douglas Talbott defines it as “stinkin thinkin.”
“Process addiction” was added as a potentially impairing illness including compulsive gambling, compulsive spending, compulsive video gaming, and “workaholism.” According to the FSPHP “the presence of a process addiction can be problematic or even impairing in itself, and it can contribute to relapse of a physician in recovery. As such, process addictions should be identified and treated.” They define three levels of relapse. “Relapse without use” is a 12-step concept. G. Douglas Talbott defines it as “stinkin thinkin.”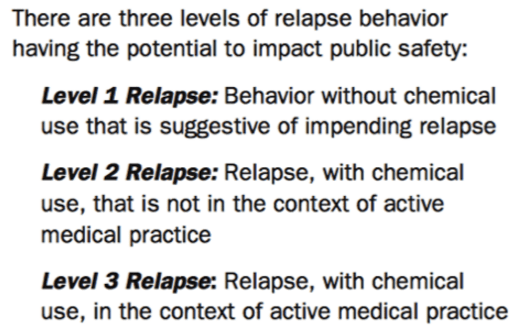
According to Judith Eaton of the Massachusetts PHP, Physician Health Services, Inc. (PHS), not having “complete, accurate, and up-to-date records” could be a red flag for such a potentially impairing illness as “when something so necessary is not getting done, it is prudent to explore what else might be going on.”
The FSMB and state medical boards have gone on to condone polygraph testing and non-validated neuropsychological testing pseudoscience in their “disruptive physician” exams. Is the magic 8 ball and tea leaves next? How low does the credibility compass have to go before someone stands up and calls bullshit on this carnival? The most egregious of indiscretions has been the introduction and acceptance of junk-science.
“Medical Sanctification of Junk-science”
Those behind the Inquisition knew they did not have to convince everyone to get what they wanted, just Ecclesiastical and political authority. The same applies here. Ethyl Glucuronide (EtG) was introduced in 1999 as a biomarker for alcohol consumption,17 and subsequently suggested as a tool to monitor health professionals by Dr. Gregory Skipper because of its high sensitivity to ethanol ingestion.
 What is so egregious about this is there was absolutely no evidence base. Skipper, who was convicted of a felony in Oregon and had his licenser revoked but got it back by claiming he was redeemed through A.A. read about it and after a study on just 14 patients pitched it to a drug testing company as a Laboratory Developed Test (LDT). The LDT pathway is a shortcut to get lab tests approved (under the premise that it will be used in treating a person medically and is thus of benefit) but Skipper took advantage of this loophole to develop a “forensic” LDT. He then used his position as the Alabama PHP Director to pitch it to the Medical Board before the ink dried.
What is so egregious about this is there was absolutely no evidence base. Skipper, who was convicted of a felony in Oregon and had his licenser revoked but got it back by claiming he was redeemed through A.A. read about it and after a study on just 14 patients pitched it to a drug testing company as a Laboratory Developed Test (LDT). The LDT pathway is a shortcut to get lab tests approved (under the premise that it will be used in treating a person medically and is thus of benefit) but Skipper took advantage of this loophole to develop a “forensic” LDT. He then used his position as the Alabama PHP Director to pitch it to the Medical Board before the ink dried.
As an LDT the FDA has no control over advertising so the lab can make any claims they want and in this case they claimed a positive EtG (> 100) was definitive proof of drinking. The State PHPs started using them on physicians. As PHPs were using them, the labs were able to sell it to other groups seeing they were “medically sanctified.” The test was subsequently found to be so sensitive that it could measure incidental exposure to alcohol in foods, over the counter cold medications, mouthwash18,19, hand sanitizer gel20, and nonalcoholic wine.21 Sauerkraut and bananas have even been shown to cause positive EtG levels.
After a Wall Street Journal Article came out debunking the test most monitoring programs abandoned it. PHPs did not. Talbott puts out a list of literally hundreds of products doctors need to avoid including colognes, mouthwashes, and foods.
Skipper simply kept raising the cutoff point from 100 to 250 to 500. It is now known hand sanitizer alone can cause a level of 2000. He subsequently introduced other tests as confirmatory tests.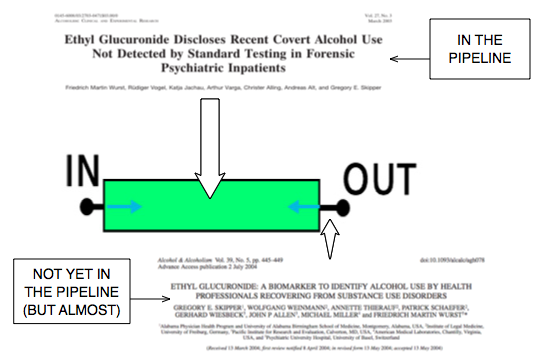
Many people had licenses revoked, loss of custody of their children, went back to jail, and suffered multiple other losses. If you look at the evidence base it is absent. There is nothing. The emperor has not clothes. This is a racket and the damage has been grave.
These same people are trying to sell the “PHP-blueprint” and its array of non-validated test to other populations as the “new paradigm” just as they did with the snake oil tests. The same carney hucksters are promoting the whole enchilada as a package deal. In “Six lessons from state physician health programs to promote long-term recovery” Robert Dupont and Dr. Greg Skipper attribute a high success rate to the following factors:22
(1) Zero tolerance for any use of alcohol and other drugs;
(2) Thorough evaluation and patient-focused care;
(3) Prolonged, frequent random testing for both alcohol and other drugs;
(4) Effective use of leverage;
(5) Defining and managing relapses; and
(6) The goal of lifelong recovery rooted in the 12-Step fellowships.22
Caveat emptor people. Caveat emptor! Any argument should be based on its own merits and methodology and evidence must be examined to discern its validity. Hopefully other agencies will look at this with a more jaundiced eye and less obtusity than the FSMB and state medical boards.
Unfortunately the position of the regulatory agencies towards this illegitimate authority and irrational authority has been one of uncritical acceptance and blind faith. It is the absence of objective assessment and critical analysis that has enabled the FSPHP and PHPs to gain tremendous sway in the medical profession and cause tremendous harm to the medical profession. By confusing ideological opinions with professional knowledge the medical boards have rubber stamped whatever’s been thrown their way and for this they should be ashamed. The impact of this close alliance between state medical boards and their state physician health programs (PHPs) and their national organizations on the current state of medicine has not been examined. It needs to be.

- Jost TS, Mulcahy L, Strasser S, Sachs LA. Consumers, complaints, and professional discipline: a look at medical licensure boards. Health matrix. Summer 1993;3(2):309-338.
- Galusha BL. Quality initiatives. The role of medical licensing and disciplinary boards. Quality assurance and utilization review : official journal of the American College of Utilization Review Physicians. Aug 1988;3(3):66-70.
- Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and Characteristics of Physicians Prone to Malpractice Claims. The New England journal of medicine. Jan 28 2016;374(4):354-362.
- Seeling SS. Thoughts on the reliability of drug testing. Federation bulletin / Federation of State Medical Boards of the United States. Aug 1988;75(8):230-234.
- The sick physician. Impairment by psychiatric disorders, including alcoholism and drug dependence. JAMA : the journal of the American Medical Association. Feb 5 1973;223(6):684-687.
- Stimson GV. Recent developments in professional control: the impaired physician movement in the USA. Sociology of health & illness. Jul 1985;7(2):141-166.
- King M, Durcanin C. The suicides at Ridgeview Institute: A Doctor’s treatment program may be too tough, some say. Atlanta Journal and Constitution. December 18, 1987a, 1987: A12.
- Durcanin C, King M. The suicides at Ridgeview Institute: Suicides mar success at Ridgeview with troubled professionals. Atlanta Journal and Constitution. December 18, 1987, 1987: A13.
- King M, Durcanin C. The suicides at Ridgeview Institute: Many drug-using doctors driven to Ridgeview by fear of losing licenses. Atlanta Journal and Constitution. December 18, 1987b, 1987: A1.
- Petry NM, Alessi SM, Hanson T, Sierra S. Randomized trial of contingent prizes versus vouchers in cocaine-using methadone patients. Journal of consulting and clinical psychology. Dec 2007;75(6):983-991.
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. Feb 2006;101(2):192-203.
- Gonzales L. When Doctors are Addicts: For physicians getting Drugs
is easy. Getting help is not. Chicago Reader. July 28, 1988, 1988.
- Ricks WS. Ridgeview Institute loses $1.3 million in suit over suicide. Atlanta Journal and Constitution. October 11, 1987, 1987: A1.
- Durcanin C. The suicides at Ridgeview Institute: Staff members didn’t believe Michigan doctor was suicidal. Atlanta Journal and Constitution. December 18, 1987, 1987: A8.
- Schneidman B. The Philosophy of Rehabilitation for Impaired Physicians. The Federal Bulletin: The Journal of Medical Licensure and Discipline. 1995;82(3):125-127.
- Merlo LJ, Gold MS. Successful Treatment of Physicians With Addictions: Addiction Impairs More Physicians Than Any Other Disease. Psychiatric Times. 2009;26(9):1-8.
- Wurst FM, Kempter C, Seidl S, Alt A. Ethyl glucuronide–a marker of alcohol consumption and a relapse marker with clinical and forensic implications. Alcohol Alcohol. Jan-Feb 1999;34(1):71-77.
- Costantino A, Digregorio EJ, Korn W, Spayd S, Rieders F. The effect of the use of mouthwash on ethylglucuronide concentrations in urine. Journal of analytical toxicology. Nov-Dec 2006;30(9):659-662.
- Reisfield GM, Goldberger BA, Pesce AJ, et al. Ethyl glucuronide, ethyl sulfate, and ethanol in urine after intensive exposure to high ethanol content mouthwash. Journal of analytical toxicology. Jun 2011;35(5):264-268.
- Rosano TG, Lin J. Ethyl glucuronide excretion in humans following oral administration of and dermal exposure to ethanol. Journal of analytical toxicology. Oct 2008;32(8):594-600.
- Hoiseth G, Yttredal B, Karinen R, Gjerde H, Christophersen A. Levels of ethyl glucuronide and ethyl sulfate in oral fluid, blood, and urine after use of mouthwash and ingestion of nonalcoholic wine. J Anal Toxicol. Mar 2010;34(2):84-88.
- Dupont RL, Skipper GE. Six lessons from state physician health programs to promote long-term recovery. Journal of psychoactive drugs. Jan-Mar 2012;44(1):72-78.

ASAM plan to have doctors drug test Almost everyone using non- FDA approved testing
The Plan to… Require Doctors to Drug-Test all Patients.
The MRO looks for what are called “fatal flaws” and, should one be present, invalidates the test. A fatal flaw requires the test be rejected as it were never drawn. It invalidates it and it cannot be used.
Forensic versus Clinical Drug Testing
Forensic drug testing is done for medico-legal purposes. It is used for testing people for substances of abuse or substances in those who should not be using them. Forensic drug testing results in consequences. These consequences can be grave and far-reaching if the drug-testing is being done by a regulatory agency or some other body given the power to sanction or punish. Loss of careers, of child-custody, and of rights and freedoms can all depend on results of a single test.
 Random drug-testing done in the workplace is also forensic but the consequences are usually quite different. A positive drug-test done in this manner typically results in an assessment, treatment if indicated, and compliance with some sort of monitoring protocol in order to return to work.
Random drug-testing done in the workplace is also forensic but the consequences are usually quite different. A positive drug-test done in this manner typically results in an assessment, treatment if indicated, and compliance with some sort of monitoring protocol in order to return to work.
Forensic drug testing follows more stringent guidelines than clinical testing because of these consequences. Some are more stringent than others, requiring split-specimen samples and the use of only certified labs. But the minimum requirements for any and all drug testing include strict chain-of-custody procedures and review by a certified MRO.

Clinical drug testing, on the other hand, occurs in the course of a doctor caring for a patient. It is done to diagnose and treat and cannot be used outside this purview. The results of a clinical test are part of the medical record and deemed ‘Protected Health Information’ (PHI). The results are protected by HIPPA and cannot be disclosed to anyone not directly involved in your direct medical care without your written consent. There are no additional guidelines in place for clinical drug-testing as patient autonomy is preserved. A positive result could result in a recommended course of action by the physician but it is still up to the patient whether or not to follow that recommendation. It is not imposed. But there are some groups who want to change that by blurring the lines between “forensic” and “clinical” drug testing.
The ASAM White Paper on Drug Testing
According to the ASAM White Paper on Drug Testing, clinical drug-testing “employs the same sound procedures, safeguard, and systems of information management that are used for all other health-related laboratory tests, tests on which life-and-death medical decisions are commonly made.” In the box above they describe the multiple safeguards in place and requirements demanded of “forensic” drug testing, but do not mention the reason these uncompromising and multiple specifications exist is to protect the donor from a false accusation of drug or alcohol use. They proceed to define “clinical drug testing” as “part of a patient examination performed for the purposes of diagnosis, treatment, and the promotion of long-term recovery”, noting that clinical testing “must meet the established standards of medical practice and benefit the therapeutic relationship, rather than meeting the formal legal requirements of forensic testing.” The authors then state that the “majority of drug testing done today” includes both forensic and clinical elements, using individuals on parole and probation as examples.
The logical fallacy here is striking. It is comparing apples and oranges. After detailing the specific quality-assurance safeguards designed to prevent the donor of a drug or alcohol test from being falsely accused of illicit use, the authors give a general definition and purpose of “clinical” testing then state that when testing for drugs the systems in place are up to snuff as it is already being used to make life-and-death medical decisions. The take-home message is that “forensic” testing is unnecessary hyperbole designed for legal challenges. The clinical lab systems in place are used for critically important testing so it can be used for drug-testing. After all, parolees and probationers don’t require it.
Forensic guidelines developed in collaboration with occupational and environmental medicine specialist, clinical and forensic toxicologists, pathologists and others, and each of these requirements exists to assure the validity and accuracy of the testing process and protect the donor. If “clinical” testing context had fit the bill then “forensic” testing would not have evolved. Labs ordered clinically in the course of patient care are interpreted within the context of multiple other pieces of data. Lab errors occur all the time and are interpreted in that context.
Chain-of-custody and MRO review are critical and that is why most drug-testing programs follow the forensic protocol. And the example of non-forensic drug-testing parolees and probationers is misleading. Any Employee Assistance Program that has a union or some other group looking out for their best interests uses strict “forensic” guidelines. Parolees and probationers have no power and have no choice. Besides, the National Association of Drug Court Professionals uses the Laboratory Developed Tests these same people introduced to test individuals on probation or parole in the criminal justice system just as they do in the PHPs.
The ASAM White Paper:
“Encourages wider and ‘smarter’ use of drug testing within the practice of medicine and, beyond that, broadly within American society. Smarter drug testing means increased use of random testing* rather than the more common scheduled testing,* and it means testing not only urine but also other matrices such as blood, oral fluid (saliva), hair, nails, sweat and breath when those matrices match the intended assessment process.
In addition, smarter testing means testing based upon clinical indication for a broad and rotating panel of drugs.”
ent

The Proposed Expansion of “physician health programs” (PHPs)and the urgent need for a critical analysis of irrational and illegitimate authority

Physician Health Programs (PHPs) claimed “gold standard” for addiction treatment. “80% success rate” being used to promote “new paradigm” to other populations.

1. National Physician Health Program Blueprint Study Publications List
2. Setting the Standard for Recovery: Physicians’ Health Programs
————————————————————————-
PHPs are essentially Employee Assistance Programs (EAPs) for doctors. The vast majority of people know little or nothing about Physician Health Programs (PHPs).
Physician Health Programs (PHPs) are being called the “gold-standard” for EAPs. Claims of unparalleled success are being used to promote PHPs to other populations as a “replicable model of recovery.”
Drs. Robert Dupont and Gregory Skipper are promoting PHPs as “A New Paradigm for Long-Term Recovery” claiming an 80% success rate in doctors.
An article entitled “What Might Have Saved Philip Seymour Hoffman,” claims PHPs “ought to be considered models for our citizenry” and the “best evidence-based addiction treatment system we have going.” The author repeats the 80% success rate for doctors and claims Philip Seymour Hoffman might still be alive if he had been treated using the PHP model.
The basis for these claims is a 2009 study published in the Journal of Substance Abuse Treatment entitled Setting the Standard for Recovery: Physicians’ Health Programs and authored by Robert Dupont, A. Thomas McLellan, William White, Lisa Merlo and Mark Gold.
This study is the cornerstone of the “PHP-blueprint.” It is the very foundation on which everything else is based, a Magnum opus used to lay claim to supremacy that has been endlessly repeated and rehashed in a plethora of self-promotion and treatment community blandishment.
To date there has been no academic analysis of the “PHP-Blueprint.” There has been no Cochrane type analysis or critical review. There has been no opposition to its findings or conclusions which are paraded as fact and truth without challenge or question and there is a general lack of concern from those both within and outside the medical profession.
The Expansion of Physician Health Programs (PHPs) to Other Populations
1. Although these programs claim to help doctors they may actually be harming many and contributing to suicide.
2. The plan is to greatly expand these programs to other populations and you could be next.
In 2012 Robert Dupont delivered the keynote speech at the Drug and Alcohol Testing Industry Association annual conference and described a “new paradigm” for addiction and substance abuse treatment and proposed expansion of this paradigm to other populations including workplace, healthcare, and schools.
It is therefore critical that the “PHP-blueprint” be examined using critical reasoning and evidence base. All of this needs to be assessed in terms of legitimacy and intent.
Lack of Evidence-Base and Conflicts of Interest
A cursory analysis of the study on which this success rate is based reveals very little evidence base.
The claim of 80% success rate in physicians is based on Setting the Standard for Recovery: Physicians’ Health Programs is unfounded. The study is a poorly designed using a single data set (a sample of 904 physician patients consecutively admitted to 16 state PHP’s).
It is non-randomized and non-blinded rendering the evidence for effectiveness of the PHP treatment model over any other treatment model (including no treatment) poor from a scientific perspective. The study contains multiple flaws in both reasoning (type I and type II errors) and statistical analysis that render its conclusions invalid.
In addition the impact of undeclared but substantial financial conflicts-of-interest (including funding by drug testing and addiction treatment industries) and personal ideological biases (including personal 12-step recovery from addictions) in the authors of this study also needs to be considered.
Moreover the misdiagnosis and over-diagnosis of addiction in physicians in this paradigm incentivized by lucrative self-referral dollars for expensive 90-day treatment programs is a significant factor.

False Endpoints and High Mortality Rate
The mean age of the 904 physicians was 44.1 years. They report that 24 of 102 physicians were transferred and lost to follow “left care with no apparent referral.”
What happened to them? These are physicians with multiple identifiers (state license, DEA, UPIN, etc) not transient drifters.
More importantly what happened to those 48 who were reported to the Medical Board for noncompliance and had their licenses revoked–that would be the critical time when this population would be at most risk for completing a suicide. That would be when hope was lost and the coerced physician, knowing that the fight was over, would take that step.
The outcomes they used were the last reported status of the PHP participant enrolled in the program. Measuring success of program completion in doctors compared to the general population is meaningless as the short-term outcomes are quite different in terms of the external consequences imposed. The consequence of not completing a PHP is the invariably career ending. So what happened to the 24 of who “left care with no apparent referral,” the 85 who “voluntarily stopped or retired,” and the 48 who “involuntarily stopped or license revoked.”
Whether you leave a PHP voluntarily, involuntarily, or with no apparent referral it is the end game and your career is over. Comparing this to other populations where the consequences of failing to complete the program are not so final is inappropriate. Claiming superiority over programs with a 40% success rate is unfounded because for most of those people the consequences are not so final and may mean nothing more than an increase in testing frequency.
The big question is what happened to the 157 physicians who left or stopped? How many of them killed themselves. With an average age of 44 there were 6 reported suicides 22 deaths, and another 157 no longer doctors. I would venture to say the number of suicides is a lot higher than they claim. But using the last recorded PHP status as the final outcome obfuscates this.
Due to the severity of the consequences a 20% failure rate is quite concerning. This is of particular concern because many doctors (if not most) monitored by PHPs are not addicts.
As noted above, PHPs are essentially Employee Assistance Programs (EAPs) for doctors. Most EAPs, however, were developed in the presence of trade unions and other organizations working on behalf of the best interests of the employee. This collaborative effort led to EAPs that were more or less “organizationally just” with procedural fairness and transparency.
Imposed 12-step ideology and use of non-FDA Approved Drug and Alcohol Testing
 No such organizations exist for doctors. Due to the absence of oversight and accountability PHPs have been able to use non-FDA approved laboratory developed tests of unknown validity on doctors without any opposition.
No such organizations exist for doctors. Due to the absence of oversight and accountability PHPs have been able to use non-FDA approved laboratory developed tests of unknown validity on doctors without any opposition.
The distinction between professional and private life as a fundamental value of our society and the importance of this boundary was also upheld by these groups.
In the PHP paradigm no procedural fairness or transparency exists and the boundary between professional and private life has eroded.
PHPs impose 12-step ideology on all doctors referred to these programs. State Medical Boards enforce this in violation of the Establishment Clause of the 1st Amendment yet there is little recourse for doctors as they are threatened with non-compliance and loss of licensure.
Selling the PHP Paradigm
The use of 12-step is most likely not ideologically driven but profit driven.
Abstinence based 12-step programs justify the use of frequent drug and alcohol testing with ongoing lifelong assessment and treatment. As with drug-courts, PHPs provide a lucrative model to the drug and alcohol testing, assessment and treatment industry.
The plan to expand this to other populations is outlined in the ASAM White Paper.
This concerns all of us. The first step needs to be a critical appraisal of Setting the Standard for Recovery: Physicians’ Health Programs, the foundation of their claims of an 80% success rate and a conflict-of-interest analysis of its authors. The legitimacy of the study and its claims needs to be questioned.
It does not take a Cochrane review to see that the emperor has no clothes. This is not difficult. It is straightforward and simple.
As an illegitimate and irrational authority it is necessary that this opinion remain unchallenged. We need to challenge it.
Historical, political, economic and social analysis reveals that the “PHP-blueprint” is a false-construct built on circumnavigation and obfuscation. An evidence-based scrutiny of the literature would reveal it to be invalid and of little probative value.
But if nobody speaks up it is inevitable that they will expand the “PHP blueprint” to other employee assistance programs and schools.
This is not just about doctors. You too are at risk for coercion, control, conformity and forced adherence to a lifetime of abstinence and 12-step indoctrination and if you do not speak up now it won’t be a risk but a certainty.


Request Medical School Administrators Question PHP Authority to Prevent Future Medical Profession Brain Drain

Physician Health Programs (PHPs) now targeting medical students–More sheep for the slaughter
The attached article entitled “Medical school drug testing is a moral and scientific failure” opposes testing medical students for drugs and alcohol but things are going to get a whole lot worse.
In the past six-months I have been contacted by an increasing number of medical students searching for help after being trapped in quagmire of their state physician health program (PHP). Each of them had either been referred to a “PHP-approved” assessment center or had already had an evaluation recommending inpatient treatment.
Some of these students were subjected to non-FDA approved laboratory developed tests including hair testing for marijuana metabolites and the alcohol biomarker EtG. These typeof tests can detect substances that were used days, weeks and even months prior to testing.
Medical students and physicians are just as likely to have experimented with illicit substances in their lifetimes as their age and gender matched peers.1
Although medical students as a group drink slightly more alcohol than the general population, the pattern and prevalence of alcohol, dependence is consistent with their age mates in the general population.1 2
Like it or not recreational and experimental drug use is widespread in young adults and most of them “grow out of it” and the 21st Amendment repealed the Volstead Act in 1933. Alcohol is legal and those that can handle it have a right to a round of beers after a long day or imbibe a cocktail with a dinner date. But according to the prohibitionist profiteers and moral preeners any drug or alcohol use is a sign of “potentially impairing illness” that must be addressed and treated early to prevent an inexorable slide into a chronic relapsing brain disease and abstinence and lifelong adherence to the principles 12-step spirituality are the only way to do so.
An old joke asks “How does a doctor define an alcoholic?” Answer–“anybody who drinks more than he does.” How does a PHP define an alcoholic? Answer –anybody who walks through the front door.
In reality, a zero-tolerance paradigm utilizing this type of testing would be ruinous. With recreational and experimental drug use common in young adults a profession that refuses to accept anyone who tests positive for drugs will exclude large numbers of brilliant, talented individuals. Dismissing highly talented people in medicine for what might be a one-off recreational non problematic drug experience would retard its advance.
The use of these non-FDA approved tests of unknown validity should not be allowed to begin with but there needs to be a concerted direct attack on their use on medical students or the brain-drain on the profession will bring it back to the dark ages. The ASAM White Paper on Drug Testing proposes imposing this system with mandatory drug testing by the healthcare system from childhood to old age. College loans are proposed as “leverage” for college students in this “contingency management” paradigm so a lot of promising students could be weeded out before even applying to medical school. Forget GPA and MCATS as the primary criteria for medical school admission will be sobriety and clean urine screens..
Diagnosing disease without meeting the diagnostic criteria for that disease.
None of the students who contacted me seemed to fit the diagnostic criteria for the diagnosis given to them stories which were articulate, detailed and sincere. All cases involved either a naive mistake or isolated incident.
One student made the disastrous revelation to a PHP director who had just given a class lecture that she had smoked marijuana with her high school friends in her home state of Colorado. She was then called in by the PHP and referred for an evaluation at an out of state facility where she was diagnosed with “marijuana dependence” based on a positive low level THC metabolite on a hair follicle test. She was told she was in denial and inpatient treatment was recommended. Although she admitted to occasional weekend marijuana use there were absolutely no problems in any realm of her life. It is self-evident that impairment due to drugs or alcohol impacting someones capacity to work or function needs to be addressed but the penalty imposed on her for her private behavior was to end her career in medicine before it even started. The medical school administration mandated she either complete the treatment required by the PHP or she would not be able to enroll the following semester and not being able to come up with the up-front out-of-pocket cost for treatment she was not able to return to the medical school and has decided to pursue a different career.
Another student was anonymously reported to the PHP for smoking marijuana at a weekend party which resulted in a similar assessment and recommendation for inpatient treatment. After spending 3 months at a facility in Alabama he is now under monitoring contract with his PHP but returned to school.
Healthy student asks for help in his organizational skills–ends up with a psychiatric and substance abuse diagnosis
After reading an advertisement in the state medical society newsletter promoting work-life balance a second-year medical student contacted his state PHP to obtain advice on his problem with “procrastination.” Classes and working part time in the endocrinology lab left him with little time and he found himself slacking off on his exercise routine and burning the midnight oil before test nights. He told the PHP director about his history of depression after his father died immediately before his freshman year at college. That October he became overwhelmed with sadness and missed his dad and hometown. He sought help from the campus physician who prescribed prozac which was discontinued in a years time without return of any symptoms.
Realizing there were no classes in work-life balance but only a support group for “burnout” the student declined the PHP directors offer of an assessment of his “mental health.” Much to his surprise he was called in the following week by a medical school administrator and told that the PHP was requiring an assessment at one of two out of state “PHP-approved” assessment centers in Lawrence Kansas. He was at first confused at the nonsense he was hearing and then became indignant at the nonsensical and illogical request without rhyme or reason and the betrayal of trust and ethics. “Surely this must be a HIPPA violation.” He obtained an outside consultation from a psychiatrist and contacted the campus physician who confirmed his diagnosis was acute situational depression and bereavement but the PHP disregarded the information. He bartered for a local evaluation but this was refused. He arranged for the 96-hour assessment in Kansas. His mother paid the requisite out-of-pocket up-front $4,500.00 to the facility and she told him not to worry as his life would get back to normal after they confirmed he had no psychological problems. “Dysthymia, Major depressive disorder, severe, in remission and alcohol use disorder” were given as diagnoses. “Alcohol use disorder” was based on a hair test for EtG which was the result of his drinking an occasional beer or two with friends after school and on the weekends. He was told he may be “self-medicating” and playing “Russian roulette” given his history of depression. Recommendations included inpatient treatment followed by a “structured aftercare program” of abstinence and monitoring by for alcohol and drugs of abuse. Forced to sign a contract with the PHP he was understandably upset at the serious and unfounded sequelae that was the result of asking for help.
Another fourth-year student got into a bit of a shoving match with his buddy at the bar on a Saturday night and was reported to his PHP anonymously. He is awaiting evaluation.
This brings up another potential problem–sham peer review. As PHPs accept anonymous referrals what is in place to prevent inappropriate referrals based on removing a competitor and improving your academic standing.
A legitimately prescribed stimulant for ADHD bought a third year student into a PHP contract. He was forced to discontinue the medication prescribed by a psychiatrist specializing in childhood ADHD by a family practitioner in “recovery” from abusing intravenous fentanyl who had been monitored by the PHP himself for ten years then became medical director after getting board certified as an addiction medicine specialist.
This student got 99th percentile across the Board on his MCATs and may one day cure cancer but now faces an uncertain future as he recently got a positive EtG on a urine test and they are currently “sorting this out.”
The most bizarre story was from a student who sought help for sleep troubles after reading about the PHP as a referral source. He subsequently saw a sleep-specialist and was diagnosed with an oversized uvula which was surgically corrected. His sleep troubles improved but his troubles with the PHP remained. A triathlete and excellent student the PHP determined he had a “thought disorder” and discussions of “schizophrenia” were entertained by the PHP and they recommended an out of state evaluation at one of the three gulags used by the FSPHP for “disruptive physician” and behavioral exams–Vanderbilt, Acumen and the Professional Renewal Center. All of these facilities come with a guaranteed diagnosis. Polygraphs and unvalidated neuropsychological instruments designed to detect “character defects” cast a pretty wide net.
Question FSPHP with direct questions to undermine a “culture of professionalism.
It is important that medical school administrators refuse to engage in blind deference to the authority of the state PHP. Authority must always be questioned and to not do so is irresponsible. Unquestioning allegiance to an authority does not comport with the history of the medical profession or science. Faith in institutions demands mass adherence to faith in that authority and direct challenges to the status quo are needed to undermine that faith. They have bamboozled the medical boards into implementing bad policy, approving bad science and making bad decisions. They have duped state legal authorities into deference to their expertise and integrity under the notion that questioning these attributes undermines a culture of professionalism. Fact of the matter is they have no expertise, no integrity and no professionalism.
PHPs have been contaminated with an outside influence and support an agenda that has nothing to do with protecting the public or helping medical students. They are an illegitimate authority that has become an irrational authority and their recommendations mandate direct answers and justification.
If the PHP has concerns about a student then the first step should be to obtain an independent second opinion. PHPs discourage second these second opinions and disregard all outside expert opinion no matter how well qualified and experienced that expert is. Anyone outside this brood of addiction addicts is scoffed at as biased or unenlightened to the simplistic belief system with which they have contaminated the medical profession. Look into the assessment centers to which they are mandating referral. Ask what qualitative factors and quantitative measurements were used to approve that facility and why no one in Massachusetts has the ability come to a competent diagnosis. The yarn that doctors and medical student have an ability to dissemble and appear normal while harboring a “potentially impairing condition” is one of the medical urban legends they started. Ask to see the evidence base. There is none and it defies common sense, logic and science.
An increasingly bright light is being shed towards the malfunctions and corrupt practices of this unaccountable confederacy of “authorities” and at some point soon their jig will inevitably be up. In the interim, if you are referred to a PHP it would be a good idea obtain independent lab tests and two second opinions. Although the PHP will disregard this documentation it would be wise to obtain it to prove both your normality and the discrepancy between your independent evaluation results and the cherry-picked pulled out of a hat multiple diagnoses confabulated and misrepresented by the PHP.
- Hughes PH, Brandenburg N, Baldwin DC, Jr., et al. Prevalence of substance use among US physicians. JAMA : the journal of the American Medical Association. May 6 1992;267(17):2333-2339.
- Flaherty JA, Richman JA. Substance use and addiction among medical students, residents, and physicians. The Psychiatric clinics of North America. Mar 1993;16(1):189-197.

Medical school drug testing is a moral and scientific failure
ANONYMOUS | EDUCATION | MAY 11, 2014
Before the 1980s, drug testing was uncommon. It was widely viewed as an invasion of privacy and an infringement on fourth amendment rights. Today, a medical student is likely to be drug tested before entering medical school, before clinical rotations, and/or before residency. If preventing drug use among medical students is the goal of these tests, they have failed miserably. Urinalysis drug tests are ineffective. But more importantly, they are immoral.
Drug tests are ineffective for two reasons. First, they basically just test for marijuana. A 10 panel urinalysis technically tests for 10 different drugs, but marijuana is one of the only drugs that can be detected for more than 30 days. Cocaine can be detected for 4 days. Amphetamine, methamphetamine, ecstasy, heroin, and codeine all can be detected in urine for only 2 days. This means that a user of drugs far more dangerous than marijuana needs to abstain for just a couple of days. Psilocybin mushrooms, as well as several other mind-altering drugs, are not tested for at all.
For a marijuana user, a drug test might seem like a nightmare. But here we arrive at the second reason why drug tests are ineffective, they are easily beaten. A marijuana user may choose to drink a lot of water before his drug test to dilute his urine. Alternatively, he may choose to use a friend’s urine who he knows does not use marijuana. Either one of these options might work. But fortunately for such a marijuana user, there is another option that is essentially risk free, synthetic urine. There are several companies that make synthetic urine capable of beating drug tests. The word on the Internet is that Quick Fix is a safe bet. I personally know some people who would agree. At just $30 for a bottle, it looks like the drug test is no match for the free market.
Do not just take my word for it though. In 2003, the University of Michigan conducted a study on the effectiveness of drug testing students. From nearly 900 schools, the study found that drug testing, whether routine, random, or based on suspicion, had no measurable effect on drug use among students. Put simply, drug testing accomplishes nothing.
The most important concern I have about drug testing medical students is a moral one. Regardless of their effectiveness, or ineffectiveness, the endgame of drug testing is to prevent drug users from becoming doctors. Users, not addicts; and there is a big difference. A marijuana user might use on weekends or at night to relax, much like an alcohol user. A marijuana addict, although rare, is the type of person who might show up to important occasions intoxicated. The statistics on marijuana addiction vary. They usually show that less than 10% of users become addicts, but they always show that alcohol users have higher rates of addiction. A urinalysis detects alcohol for no more than 12 hours after use. This means that medical students who use alcohol are more likely to be addicted, and they face basically no risk of failing a drug test.
Should we be worried about medical students being drunk in clinical settings? Of course. And we should also be worried about medical students being high in clinical settings. Intoxication could be disastrous and it needs to be prevented. The good news is that this is done naturally. It is highly unlikely to find medical students who are addicts of marijuana, alcohol, or any mind-altering drug. I believe it is safe to say that the rigor of medical school itself prevents drug addicts from becoming doctors. There are, however, drug users who will make it into medical school or other rigorous scientific careers. Actually, many of them thrive. Richard Feynman, Kary Mullis, and Francis Crick used marijuana and LSD, Carl Sagan used marijuana, and Oliver Sacks used several illicit drugs. When drug tests are required for every medical student, the casual drug user, no matter how much potential he has, is bullied for no reason. The potentially dangerous drug addict has already been weeded out long ago.
Medical school is supposed to be based on science. The science shows that drug testing does not work. If it did work, then many great scientists would have been removed from their professions. These facts alone should be enough to settle the issue, but it is important to look at two more moral objections we should all have.
First, drug tests are not free. Before entering medical school, I paid about $30 for one. This does not sound like much. But charging students even one penny is unacceptable, for there is not even a fraction of a penny in benefit from these tests. The nearest drug testing facility for me was a 20 minute drive from my house. I could have driven anywhere for 20 minutes and just handed $30 to any random person. Surely, that $30 would bring more value to society than $30 wasted on a drug test. Imagine if a police officer searched a person’s car for drugs against his will, found none, and then charged this person $30. That is the reality of drug testing.
Second, drug tests are an invasion of privacy. Medical students should not be forced to prove their innocence. This creates a guilty until proven innocent environment. It immediately creates resentment among students, and rightfully so. Furthermore, what about people with paruresis? The International Paruresis Association estimates that 7% of people suffer from this condition, also known as shy bladder. Type “paruresis drug test” into a search engine and spend some time reading through the horror stories that are shared. These people suffer from a medical condition, and of all places, their medical school is completely inconsiderate.
Drug testing is a moral and scientific failure. Medical schools should be too embarrassed to take part in such nonsense.
The author is an anonymous medical student who blogs at unchainedmedical.
TAGGED AS: MEDICAL SCHOOL
Reefer Madness Redux: Is your doctor a marijuana user? Maybe you should ask.

The article below was recently published on “social media’s leading physician voice” KevinMD.com. A previous piece by the same author attempted to connect marijuana to heroin use. Interestingly, this type of archaic rigid paternalistic chatter is becoming more and more common in the articles and social media of healthcare. How, and more importantly why, is this type of tripe and rabble getting past editorial review? It is 2016 not 1958! Disappointingly, this absurd and sexist rant has generated a mere 20 comments thus far with the majority being negative. I do agree with the apt and accurate observations of “FEDUP MD” who states the following:
“The answer is not that cut and dried.
Do I want a surgeon who is clinically impaired from marijuana operating on me at the time, who just smoked a joint before entering the OR? No.
Do I care if a surgeon two weeks ago went to Aspen on vacation, smoked a perfectly legal joint at his hotel, and now is operating on me two weeks later? No.
Both come up the same on a drug test.”

Is your doctor a marijuana user? Maybe you should ask.
Marijuana use today is not limited to the poor, the marginalized among us; nor is it kept in the inner city, as it pretty much was when I was a kid. Now it is widespread, even legal in some states. One might even make the argument it has become a substantial part of the life of the elite, the affluent of America. And when we think of elite and powerful individuals among us, do we rule out doctors? I think not.
So when I read a reader’s comment to a piece I wrote recently about marijuana and its possible connection to heroin, I was not surprised when one person rejected my ideas 100 percent. He went on to say why, and used the term “weed” once or twice in doing so. I said to myself, “Now here is a person who knows firsthand a bit about marijuana use. ” His use of the term, “weed,” told me this. He no doubt possesses more than a passing interest in the subject. Others who commented seemed to share his opinion — but not all.
My understanding of drugs and their impact on lives comes largely from my lifelong occupation as a social worker. Lots of years of doing social work in many settings including a couple of years working among the Sioux of South Dakota. In those mid-sixties, years alcohol abuse on the reservation was rampant, and hardly a new story. Drugs had not yet arrived. Drugs are there now big time and the situation is horrendous, awful, drugs and alcohol together. And I believed the conditions could not become worse than what I witnessed. Well, they could, and they have.
There is another side to my experience, however. As a much younger person, I dated, while living in Boston, a heavy user of marijuana. She also took LSD regularly, which tells you how long ago this happened. I didn’t meet the woman in the conventional way, a bar or some sort of social gathering (no Internet or on-line dating services then). No, I met the lady at an airport north of Boston: Plum Island Airport, quite near the ocean. I am a private pilot, and I had landed my two-seater Piper J3, and struck up a conversation with her, and offered her a ride, which she immediately accepted, and thereupon our romance began. Straightforward enough, I hope you agree.
The J3 is a wonderful airplane, old and slow, but lots of fun to fly. There is no starter. You have to get out and spin the prop to start the engine — very old school. Women seemed to love my J3, except that it wasn’t mine; it was a loaner.
Pilots incidentally are often a fairly conservative lot. Not a great deal of alcohol or drug abuse among us. Of course, there are glaring exceptions, but most pilots I know learned quickly that mistakes in aviation can and often are deadly. There are no dented fenders. I noticed too that doctors seem drawn to flying in considerable numbers. They often have the best equipment — I never saw a doctor in a J3 — which I gather they can well afford. And I should add that I never met a woman pilot/doctor, by the way.
They also were involved in many accidents. Why? It is complicated, I suppose, but doctors are busy fellows who might find a couple hours of free time, rush to the airport and were soon airborne. Not a lot of time to practice, as in practicing takeoffs and landings. No time for that, but in aviation as in medicine, practice makes perfect, or near perfect. Also, I think confidence is an issue. For doctors, at least the ones I was acquainted with, were seldom lacking in confidence, and were, therefore, capable of getting into flight situations they may have been completely unprepared for and untrained to deal with.
So my new friend, Ellen, and I dated. She was open and very upfront with me about her heavy marijuana use. She claimed she drove better when she was high, reminding me repeatedly of this as she weaved in and out of traffic on the Mystic River Bridge leading into Boston. I’d hold my breath, and occasionally recommended she slow down. She seldom did. But still, I enjoyed Ellen’s company, and went along for the ride for easily a year or more. I won’t say her drug use drove us apart, but it did not bring us closer together either, which leads me to this (likely unpopular) observation, and query: How many doctors entering the workplace these days have more than a casual connection to marijuana? I know the same question can be asked regarding alcohol, but I am not asking that question here, and it is, after all, my essay.
My friend and I parted after a time. She never said as much, but I suspected she found me a bit dull. She eventually moved back to Virginia, and last I heard, she had wed and had a family. Good for her. So no bad ending here. Maybe that’s what everybody was expecting — what I was leading up to — but you don’t get that.
But I will say this much. I continue to be a fussy pilot, and when I travel on an airliner, which these days happens less often — I always peek into the cockpit upon entering to see who is sitting in the left-hand seat. That’s where the pilot in command sits. I like to see an older man there, a bit stout and maybe balding or gray-haired. (Please don’t ask me about female pilots.) I know such a fellow is likely experienced. He has survived a long time, is my guess.
If I were to find a young Robert Redford-type in that left-hand seat, I would become uneasy and not fully sure of what I was getting myself into.
So the point I am making here is this: I am clearly discerning as to the skill and condition of an airline pilot, someone I seldom see, so why should I not be really picky when it comes to doctors I select, and whether or not they use marijuana regularly, or even at all?
Raymond Abbott is a social worker.
Image credit: Shutterstock.com
Looking for an Investigative Reporter to Question MRO—-Procedural, Ethical and Legal Justification Needed
As the Medical Review Officer (MRO) for the Massachusetts state Physician Health Program (PHP), Physician Health Services, Inc. (PHS, inc.), Dr. Wayne Gavryck’s responsibility is simple. He is supposed to verify that the chain-of-custody in any and all drug and alcohol testing is intact before reporting a test as positive.
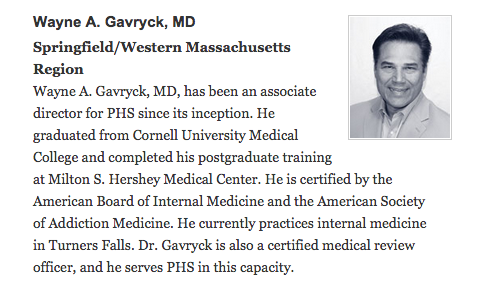
Note Dr Gavryck is: 1. Certified by ASAM; 2. A .Certified Medical Review Officer (MRO) who “serves PHS in this capacity.” Although Dr. Gavryck serves PHS I would beg to differ on the MRO function. Accessed from PHS Website 1/15/2015 http://www.massmed.org/Physician_Health_Services/About/PHS_Associate_Directors/#.VM1dZlXF-hY
Dr. Gavryck evidently did not do that here. In fact for more than a year he helped cover up an alcohol test that was intentionally fabricated at the behest of PHS Director of Operations Linda Bresnahan (who told me when I confronted her with the fact that I have never had or ever even been suspected of having an alcohol problem “you have an Irish last name–good luck finding anyone who will believe you!”
It took a formal complaint with the College of American Pathologists to get the truth out. The whole fiasco can be seen here and here.
What Gavryck and his co-conspirators did is egregious and ethically reprehensible. It shows a complete lack of moral compass and personal integrity. What was done from collection to report to coverup and everything in-between is indefensible on all levels (procedurally, ethically, and legally).
The documentary evidence shows with clarity that this was not accident or oversight. It was intentional and purposeful misconduct. I think everyone would agree that there should be zero-tolerance for forensic fraud in positions of power. Any person of honor and civility would agree.
Transparency, regulation, and accountability are necessary for these groups. It is an issue that needs to be acknowledged and addressed not ignored and covered up.
If Dr. Gavryck can give a procedural, ethical, or legal explanation of what was done then I stand corrected. Just one will suffice. I’ll erase my blog and vanish into the woodwork. But If he cannot then this needs to be addressed openly and publicly. And whether he was involved in the original fraud or not is irrelevant. As the MRO for PHS it is his responsibility to correct it–however late the hour may be.
Perhaps Dr. Gavryck needs to see some of the damage he has caused in order to take this responsibility. Known as a “bag man” who simply rubber stamps positive tests at the request of Sanchez and Bresnahan (much like Annie Dookhan) he does not see the damage that is caused. Forensic fraud has grave and far reaching effects and in this case has severely impacted many people and include patient deaths.
Perhaps Dr. Gavryck needs to take a “moral inventory” and see that this this type of behavior causes real damage to real people and put a face on it.
Perhaps Gavryck needs to be asked these questions directly from an investigative reporter.
It is people just like this who are killing physicians across the country. The body count is vast and multiple. This has recently been underscored by the horror stories mounting in recent Medscape and KevinMD articles associating PHP programs like this one with the recent epidemic of suicides in doctors.
These people have removed themselves from accountability. One way they do this is by withholding information and suppressing the truth. This is facilitated by willing sympathizers and apologists who refuse to acknowledge or investigate wrongdoing. Gavryck believes he is beyond reproach and is complacent that his friends will protect him and insulate him from harm. The evidence, however, is not going away. Neither am I.
Those who are caught doing dirty deeds such as this need to be held accountable. This requires the provision of information, justification for actions and the ability to be punished by outside groups.
I have the information. Gavryck needs to provide justification for his actions and held accountable for them. Perhaps an investigative journalist could interview him and ask him directly.
Help me get this exposed, corrected, and rectified. The doctors of Massachusetts and the doctors of this entire country deserve better than this.
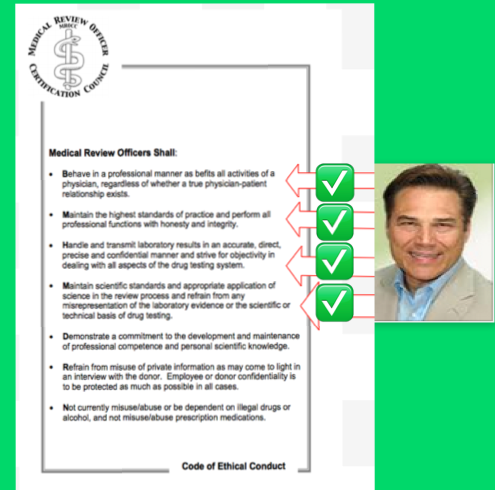
The MRO Code of Ethics–Seems like Dr. Gavryck’s breaking them in sequential order!




 These documents were requested to determine if they were ever entered into evidence as none of them had ever been addressed. The date-stamps confirm they were not. Requests to clarify the illegible dates have been curtailed and rebuffed with the last response being June 17, 2016 when Katy Condon E-mailed me that she was “currently working on it.”
These documents were requested to determine if they were ever entered into evidence as none of them had ever been addressed. The date-stamps confirm they were not. Requests to clarify the illegible dates have been curtailed and rebuffed with the last response being June 17, 2016 when Katy Condon E-mailed me that she was “currently working on it.” None of the sleazy misconduct here has ever been addressed. This is not just evidence withheld but crimes concealed and the seriousness and severity of this needs to register somewhere. The fact of the matter is a state attorney was made aware of felony crimes that were committed by identifiable individuals in obvious conspiratorial collusion to falsely create evidence. The intentions are clear. This is not accidental but deliberate. The documents were provided to a state employee who instead of reporting what they revealed, concealed them and never brought them up again. Sanchez is a Board of Registration in Medicine licensee. He must abide by the same rules and regulations and laws as everyone else. Allowances and selective application of the law are not part of good governance.
None of the sleazy misconduct here has ever been addressed. This is not just evidence withheld but crimes concealed and the seriousness and severity of this needs to register somewhere. The fact of the matter is a state attorney was made aware of felony crimes that were committed by identifiable individuals in obvious conspiratorial collusion to falsely create evidence. The intentions are clear. This is not accidental but deliberate. The documents were provided to a state employee who instead of reporting what they revealed, concealed them and never brought them up again. Sanchez is a Board of Registration in Medicine licensee. He must abide by the same rules and regulations and laws as everyone else. Allowances and selective application of the law are not part of good governance. The crimes here are not Annie Dookhan level misconduct isolated to just Massachusetts either. The documents sho collusion between a state physician health program and its drug-testing lab, a pattern that appears to be standard operating procedure as allegations of laboratory fraud as well as diagnosis fraud are coming in all across the country and the consequences of these tests can be grave. These tests end careers and can end lives. I know of multiple suicides due to allegedly false tests; many using this same test. The fact that the falsified test was requested by fax and complied with without hesitation shows a chilling absence of empathy. It is unconscionable. These are more murders than suicides as it is an institutional injustice with no lifeline. No outside agency exists with authority to both investigate lab misconduct and provide punishment if it is found.
The crimes here are not Annie Dookhan level misconduct isolated to just Massachusetts either. The documents sho collusion between a state physician health program and its drug-testing lab, a pattern that appears to be standard operating procedure as allegations of laboratory fraud as well as diagnosis fraud are coming in all across the country and the consequences of these tests can be grave. These tests end careers and can end lives. I know of multiple suicides due to allegedly false tests; many using this same test. The fact that the falsified test was requested by fax and complied with without hesitation shows a chilling absence of empathy. It is unconscionable. These are more murders than suicides as it is an institutional injustice with no lifeline. No outside agency exists with authority to both investigate lab misconduct and provide punishment if it is found. These documents show crimes. I have re-requested these records under HB 4333 as well as documents that Bertram claims “puts the matter to rest.” He claims they reviewed their “records” and “minutes’ for the December 21, 2011 hearing and all of this was “carefully considered.” This begs the question has anyone else outside this circle ever even looked at these documents? They were never considered and if the Board complies with HB 4333 the uncensored documents will add to the already overwhelming evidence that this is the case. It is certain that every illegible date uncovered will reveal a date sometime after the hearing for which it was submitted. The documents retrieved from “off-site storage” does not exist. The Board has not used off-site storage since 2004 when they installed the Document Imaging Unit. This fact can be found in multiple annual reports and other documents. The question are they trying to cover-up a cover-up of a cover-up? Why is he going to such great lengths to protect criminals, allow this racket to continue and inevitably cause a great deal of harm to many? Rules of professional conduct forbid attorney’s from being complicit in fraud. The obvious cannot be ignored. These are crimes and both the commission and concealment of them are egregious. This is not simply a matter of withholding evidence but of concealing crimes and it puts both doctors and the public in immediate or eventual danger.
These documents show crimes. I have re-requested these records under HB 4333 as well as documents that Bertram claims “puts the matter to rest.” He claims they reviewed their “records” and “minutes’ for the December 21, 2011 hearing and all of this was “carefully considered.” This begs the question has anyone else outside this circle ever even looked at these documents? They were never considered and if the Board complies with HB 4333 the uncensored documents will add to the already overwhelming evidence that this is the case. It is certain that every illegible date uncovered will reveal a date sometime after the hearing for which it was submitted. The documents retrieved from “off-site storage” does not exist. The Board has not used off-site storage since 2004 when they installed the Document Imaging Unit. This fact can be found in multiple annual reports and other documents. The question are they trying to cover-up a cover-up of a cover-up? Why is he going to such great lengths to protect criminals, allow this racket to continue and inevitably cause a great deal of harm to many? Rules of professional conduct forbid attorney’s from being complicit in fraud. The obvious cannot be ignored. These are crimes and both the commission and concealment of them are egregious. This is not simply a matter of withholding evidence but of concealing crimes and it puts both doctors and the public in immediate or eventual danger.