The Medical Profession, Moral Entrepreneurship, and Social Control
The Medical Profession, Moral Entrepreneurship, and Social Control
Sociologist Stanley Cohen used the term “”moral panic” to characterize the amplification of deviance by the media, the public, and agents of social control.1 Labeled as being outside the central core values of consensual society, the deviants in the designated group are perceived as posing a threat to both the values of society and society itself. Belief in the seriousness of the situation justifies intolerance and unfair treatment of the accused. The evidentiary standard is lowered.
Howard Becker describes the role of “moral entrepreneurs,” who crusade for making and enforcing rules that benefit their own interests by bringing them to the attention of the public and those in positions of power and authority under the guise of righting a society evil. 2
And according to cultural theorist Stuart Hall, the media obtain their information from the primary definers of social reality in authoritative positions and amplify the perceived threat to the existing social order. The authorities then act to eliminate the threat.3 The dominant ideas or ideologies are reproduced by relying on the opinions of the defining authority and then spread through the media. The communal good has been assailed.
As a society governed by organizations, associations, institutions and regulatory bodies, the medical profession is not immune to “moral panics.” A threat to patient care or the values of the profession can be identified and amplified. A buildup of public concern fueled by media attention ensues creating a need for governing bodies to act. Medical Professionalism and the Public Health has been assailed.
Unbeknownst to the general public and most members of the medical profession at large, certain groups have gained tremendous sway within medical society. Through moral entrepreneurship they have gained authority and become the primary definers of the governance of the medical profession and the social control of doctors. To benefit their own interests they have fostered and fueled “moral panics” and “moral crusades. ” Exhorting authorities to fight these threats by any means necessary they have successfully made and enforced rules and regulations and introduced new definitions and tools with no meaningful resistance or opposition.
The Inquisition did not have to convince individual citizens or the general public of their beliefs to advance an agenda; just Ecclesiastical and Political Authority. Similarly, the “impaired physicians movement” did not have to convince individual doctors or the medical profession of their beliefs to further a self-serving agenda; just regulatory and administrative authority.
Addiction Medicine Monopoly, False Authority and Conflicts of Interest
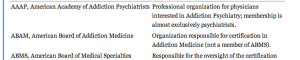
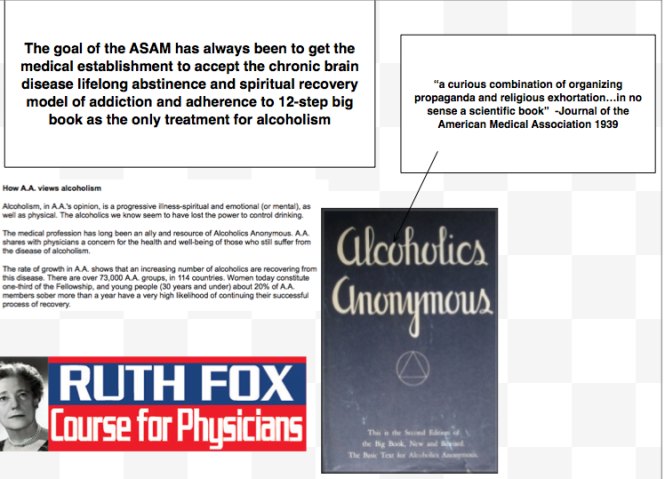
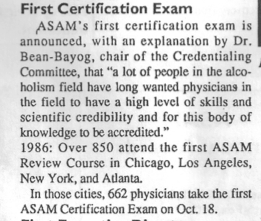
The “impaired physicians movement” can be defined as a group of physicians with alcohol and substance abuse problems who, having found sobriety through 12-step spirituality, banded together to promote the ideology behind their personal “recovery” to other doctors and the medical community at large. In the 1980s the movement gained momentum and as their numbers grew began calling themselves specialists in “addiction medicine.” The American Society of Addiction Medicine (ASAM) is not a true specialty, but a Self-Designated-Practice-Specialty, which simply means that is what they are calling themselves. It reflects neither knowledge nor expertise.. “Board certification” by the American Board of Addiction Medicine (ABAM) is not recognized by the American Board of Medical Specialties (ABMS).
ABAM certification requires only a medical degree, a valid license to practice medicine, and completion of residency training in ANY specialty. Addiction Psychiatry, a subspecialty of psychiatry under the American Board of Neurology and Psychiatry is the only specialty recognized by the ABMS. and their specialty society is the American Academy of Addiction Psychiatry.
The ASAM is schooled in just one one uncompromising model of addiction with the majority attributing their very own sobriety to that model–the chronic relapsing “brain disease” with lifelong abstinence and 12-step spiritual recovery model. As the “voice of addiction medicine,” the ASAM has nevertheless defined the dominant treatment paradigm in the United States. ASAM doctors outnumber addiction psychiatrists by 4:1 and the movement is well funded. Because addiction is defined as a “disease”, addicts must be “treated” (more often coercive than voluntary), and “cured” (defined as abstinent). The billion dollar assessment and treatment industry and the drug and alcohol testing industry lucratively profits from this model which has grown to monopolize addiction treatment in the United States.
The goal of the ABAM Foundation is to “gain recognition of Addiction Medicine as a medical specialty by the American Board of Medical Specialties (ABMS).” A monopoly defined by self-appointed experts without recognized specialty training will soon likely Robber baron their way to being accepted as a true specialty.
Physician Health Programs, Regulatory Agencies, and Treatment Centers
Physician Health Programs (PHPs) meet with, assess, and monitor doctors who have been referred to them for substance use or other mental or behavioral health problems. Unless being monitored by one, PHP practices are unknown to most physicians and operate outside the scrutiny of the medical community. Initially funded by State Medical Societies and staffed by volunteer physicians, PHPs served the dual function of helping sick doctors and protecting the public.
As the populations of ASAM physicians proliferated in the 1980s, many joined their state Physician Health Programs. PHP doctors who did not agree with the ASAM groupthink were gradually removed and they organized under the Federation of State Physician Health Programs (FSPHP). Other ASAM physicians found employment at treatment centers as staff physicians and medical directors.
The FSPHP cultivated a relationship with the Federation of State Medical Boards (FSMB) and the state PHPs formed alliances with their state medical boards. Promoting themselves as offering “treatment” rather than”punishment” they offered an alternative to disciplinary action. They then began promoting their successful outcomes in rehabilitating “impaired physicians”, and this history can be seen by examining the archives of the Journal of Medical Regulation and similar publications. In 1995 the Washington PHP claimed a success rate of 95.4%, Tennessee claimed 93% and Alabama 90%.
Part of this success was attributed to the specialized treatment centers for doctors directed by their ASAM colleagues such as Ridgeview Institute in Atlanta created by G. Douglas Talbott. Talbott, who helped organize and serve as past president of the ASAM claimed a 92.3 percent recovery rate. He also put forth a Medical Urban Legend–the proposition that doctors were a different species, separate from the rest of society, who needed special treatment three times longer than anyone else. Amazingly, this dicto simpliciter argument that can, in fact, be refuted simply by pointing it out was allowed to enter regulatory medicine unopposed. Simply because, sadly, no one ever pointed out the logical fallacy. It is now entrenched. Three months or more of treatment is standard of care for our profession. They did this by getting medical boards and the FSMB to accept fantasy as fact by relying on board members tendency to accept expert evidence at face value.
A 1995 issue of the FSMB publication The Federal Bulletin: The Journal of Medical Licensure and Discipline contains reports on eight separate state PHPs. The “almost 90% success rate” was applauded by the editor, who added “cooperation and communication between the medical boards and the physician health programs must occur in an effort to protect the public while assisting impaired physicians in their recovery.” And more recent reports suggest PHPs reduce malpractice claims. They are now being promoted as a replicable model to be used in other populations.
The problem is no one bothered to examine the methodology to discern the validity of these claims. There has been no critical analysis or Cochrane type review of any of these studies which are invariably small, methodologically flawed, and biased.
The FSMB has accepted them as expert authority and their authoritative opinion as fact. It is this acceptance of faith without objective assessment that has allowed the ASAM and FSPH to advance their agenda. By confusing ideological opinion with professional knowledge, the FSMB and state Medical Boards have acted as willing gulls each step of the way. No counter-forces existed. And they still don’t. Junk science and unvalidated neuropsychological testing is used by these groups unconstrained and willfully. There is no regulation, oversight, or accountability. They are using polygraph testing (despite the AMA’s previous public policy statement deeming it junk) to both condemn “disruptive” surgeons and deem convicted pedophiles fit to return to work. They have introduced junk-science in drug and alcohol testing and unvalidated “neuropsychological” testing to detect “character-defects” by getting regulatory agencies to accept the validity of these tests not by the Scientific Method or Evidence Based Research but by (to coin a term) “Regulatory Sanctification”
To paraphrase one FSPHP member, “Who needs evidence-based medicine when the boards have already accepted these tests as valid?” Who indeed?
The ideological bias and financial conflicts of interest between PHPs and the treatment centers was also not recognized. It still isn’t. The spotlights are apparently all on Big Pharma in this regard. Some sunlight needs to be exposed in the direction of the billion dollar drug and alcohol testing and assessment industry as well.
Doctors were held at Ridgeview three times longer than the rest of the population (and at three times the cost) under threat of loss of licensure. Although there is no evidence base or plausible explanation why an entire profession would have a three-times longer length of stay than the rest of the population this continues to be the reality. There is no choice.
in 2011 The ASAM issued a Public Policy Statement on coordination between PHPs, regulatory agencies, and treatment providers recommending that only “PHP approved” treatment centers be used in the assessment and treatment of doctors. It specifically excludes non “PHP -recognized” facilities. And what defines a “PHP approved” treatment center? In addition to finding essentially no oversight by the state medical society and medical board, a recent audit of the North Carolina PHP found financial conflicts of interest and no documented criteria for selecting the out of state treatment centers they used. The common denominator the audit missed was that the 19 “PHP-approved” centers were all ASAM facilities just like Ridgeview whose medical directors can be seen on this list.
The appeal to authority logical fallacy has enabled the FSPHP to become the expert authority on physician impairment through the eyes of the medical boards. It has also allowed them to increase their scope.
The FSMB House of Delegates adopted an updated Policy on Physician Impairment at their 2011 annual meeting distinguishing “impairment” and “illness” stating that:
“Regulatory Agencies should recognize the PHP as their expert in all matters relating to licensed professionals with ‘potentially impairing illness.'”
According to the FSPHP, physician illness and impairment exist on a continuum with illness typically predating impairment, often by many years.”
The policy extends PHP authority to cover physical illnesses affecting cognitive, motor, or perceptive skills, disruptive physician behavior, and “process addiction” (compulsive gambling, compulsive spending, video gaming, and “workaholism”). It also defines “relapse without use” as “behavior without chemical use that is suggestive of impending relapse.”
G. Douglas Talbott defines “relapse without use” as “emotional behavioral abnormalities” that often precede relapse or “in A A language –stinking thinking.” AA language has entered the Medical Profession and no one even blinked. It will get worse.
The ASAM has monopolized addiction treatment in the United States. It has imposed it on doctors through the FSPHP. The FSPHP political apparatus exerts a monopoly of force. It selects who will be monitored and dictates every aspect of what that entails. It is a, in fact, a rigged game.
Inherent in this model is the importance of external control. It gives them power to exert control over the individual regardless of whether they need to be treated.
By bamboozling regulatory medicine this was accomplished. And the maintenance of this relationship is necessary as this presentation by an FSPHP physician warns, “guard this relationship jealously.”

Moral Panics and Moral Crusades
By introducing and fueling moral panics the ASAM/FSPHP political apparatus has been able to expand in both scope and power.
The Medscape article “Drug Abuse Among Doctors: Easy, Tempting, and Not Uncommon” published in the “Business of Medicine” section in January 2014 is characteristic example of the authoritative opinion, propaganda, and misinformation spun to maintain a pervasive climate of fear. Proof by anecdote. Physicians are “5 times as likely as the general public to misuse prescription drugs” according to Lisa Merlo, PhD. “Given the epidemic of prescription addiction sweeping the nation, that’s a grim statistic.”
Described as a “researcher at the University of Florida’s Center for Addiction Research and Education,” Merlo’s research involving 55 doctors being monitored by their state Physician Health Program published in the Journal of Addiction Medicine in October 2013 found “most physicians who abuse prescription drugs” do so to “relieve stress and physical or emotional pain.” Nowhere is it mentioned on Medscape that Merlo is the Director of Research for the Florida state PHP Professionals Research Network. Physician access to medications through prescriptions, “networks of professional contacts, and proximity to hospital and clinic supplies” gives them “rare access to powerful, highly sought-after drugs” says Marvin D. Seppala, chief medical officer at Hazelden. This access “sets them apart” and “not only foment a problem” but”perpetuate it” says Seppala. “Access “becomes an addict’s top priority” and they “will do everything in their power to ensure it continues.”
“They’re often described as the best workers in the hospital,” he says. “They’ll overwork to compensate for other ways in which they may be falling short, and to protect their supply. They’ll sign up for extra call and show up for rounds they don’t have to do.”-Dr. Marvin D. Seppala
Physicians are intelligent and skilled at hiding their addictions, he says. Few, no matter how desperate, seek help of their own accord.” In reality this is absurd. And if you look at any of the current “moral panics” that are being used to suggest random suspicion-less drug testing of all doctors or promoting the Physician Health Programs as the “New Paradigm” you will inevitably find a doctor, just like Marv Seppala who is on this list as an author or interviewee. It is a given.
The terms “impaired physician” and the “disruptive physician” are used as labels of deviancy. As deviants who allegedly threaten the very core of medicine (patient care) and the business of medicine (profit) they must be stopped at all costs. Belief in the seriousness of the situation justifies intolerance and unfair treatment. The evidentiary standard is lowered. Aided by a “conspiracy of silence” among doctors in which impaired colleagues are not reported necessitates identification of them by any means necessary. Increase the grand scale of the hunt.
In this way these front-groups have successfully acted as moral entrepreneurs to make and enforce rules and put forth new definitions and mandates that serve their own interests. A retrospective non -blinded non-randomized cohort study with serious underlying methodological errors involving 904 physicians being monitored by PHPs is now being used to “set the standard for recovery.”
Across the Country doctors are going to the media, law enforcement, the AGO, and the ACLU only to be turned a deaf ear. Many consider this a “parochial” issue best handled by the medical community. Doctors reporting crimes are turned back over to the very perpetrators of the crimes. The Medical Societies and professional organizations contribute to the problem by willful ignorance. Accusations are used to disregard the claims of the accused. It is a system of institutional injustice that is driving many doctors to suicide. Hopeless, helpless, and feeling entrapped many are taking this route. And no one is talking about it. This cannot be avoided any longer.
The next target is the “aging physician.” And as they have done with the “impaired” and “disruptive” physician” the FSPHP and their affiliates are setting the stage for another “moral crusade.”
- Cohen S. Folk Devils and Moral Panics: The Creatio of the Mods and Rockers (New Edition). Oxford, U.K.: Martin Robertson; 1980.
- Becker H. Outsiders: Studies in the Sociology of Deviance. New York: Free Press; 1963.
- Hall SC, Critcher C, Jefferson T, Clark J, Roberts B. Policing the Crisis: Mugging, the State, and Law and Order. London: Macmillan; 1978.