Below images link to podcast.

They can be a terror to your mind and show you how to hold your tongue
They got mystery written all over their forehead
They kill babies in the crib and say only the good die young
They don’t believe in mercy
Judgement on them is something that you’ll never see
They can exalt you up or bring you down main route
Turn you into anything that they want you to be–Bob Dylan, Foot of Pride
Although no reliable statistics yet exist, anecdotal reports suggest a marked rise in physician suicide in recent years. From the reports I am receiving it is a lot more than the oft cited “medical school class” of 400 per year.
This necessitates an evaluation of predisposing risk factors such as substance abuse and depression, but also requires a critical examination of what external forces may be involved in the descent from suicidal ideation to suicidal planning to completed suicide. What are the cumulative situational and psychosocial factors in physicians that make suicide a potential option and what acute events precipitate the final act?
Depression and Substance Abuse no Different from General Population
The prevalence of depression in physicians is close to that of the general population 1,2 and, if one looks critically at the evidence based literature, substance abuse in medical professionals approximates that of the general population. Controlled studies using DSM diagnostic criteria indicate that physicians have the same rates (8-14%) of substance abuse and dependence as the general population,3 and slightly lower rates compared to other occupations.4,5 Epidemiological surveys reveal the same. Hughes, et al.6 reported a lifetime prevalence of drug or alcohol abuse or dependence in physicians of 7.9%, markedly less than the 14.6% prevalence reported in the general population by Kessler.7
Job Stress and Untreated Mental Illness Risk Factors
Job stress coupled with inadequate treatment for mental illness may be factors contributing to physician suicide according to one recent study. Using data from the National Violent Death Reporting System, Gold, Sen, & Schwenk, 2013 8 compared 203 physicians who had committed suicide to more than 31,000 non-physicians and found that having a known mental health disorder or a job problem that contributed to the suicide significantly predicted being a physician. Physicians were 3.12 times more likely to have a job problem as a contributing factor. In addition, toxicology testing showed low rates of medication treatment. The authors concluded that inadequate treatment and increased problems related to job stress are potentially modifiable risk factors to reduce suicidal death among physicians. They also warned that the database used likely underestimated physician suicides because of “underreporting and even deliberate miscoding because of the stigma attached.”8
Few studies have evaluated the psychosocial stressors surrounding physician suicide but there is no reason to believe they are any different from the rest of the population. Although the triggering life events and specific stressors may vary outside, the inner psyche and undercurrent of thoughts and feelings should remains the same. Perhaps the same drivers of suicide identified in other populations are contributing to physician suicide.
Perceived Helplessness, Hopelessness, Bullying and Defeat
Perceived helplessness is significantly associated with suicide as is9 Hopelessness10,11 Bullying is known to be a predominant trigger for adolescent suicide12-14 One study found that adolescents in custody who were bullied were 9.22 times more likely to attempt suicide than those were not bullied.15
Heightened perceptions of defeat and entrapment are known to be powerful contributors to suicide.16,17 The “Cry of Pain” model 18,19 specifies that people are particularly prone to suicide when life experiences are interpreted as signaling defeat which is defined as a sense of “failed struggle” or loss of social position and resources.. The person is unable to identify an escape from or resolution to a defeating situation, a sense of entrapment proliferates with the perception of no way out, and this provides the central impetus for ending ones life. There is a helplessness and hopelessness that precipitates the descent from ideation, to planning, and then to finality.
Organizational Justice Important Protective Factor
In a study on Italian and Swedish female physicians, degrading experiences and harassment at work were found to be the most powerful independent variables contributing to suicidal thoughts.20 Degrading work experiences harassment, and lack of control over working conditions were found to be associated with suicidal thoughts among Italian and Swedish male university physicians.21
Evidence exists for the role of rescue factors (i.e. social support) as buffers against suicide in the face of varying degrees of life stress.22,23 The study of female physicians revealed meetings to discuss stressful work experiences as a potential protective factor, 20 and support at work when difficulties arose appeared to be a protective factor for the male physicians.21 In line with this, studies of Finnish physicians found that control over one’s work and organizational justice were the most important determinants of work-related wellbeing.24,25 Organizational justice has been identified as a psychosocial predictor of health and wellbeing26 27 Low organizational justice has been identified as a notable risk factor for psychological distress and depression.28,29
Historical Precedent-the Suicides at Ridgeview
Could these factors be playing a role in physician suicide? They evidently did at the Ridgeview Institute, a drug and alcohol treatment program for impaired physicians in Metropolitan Atlanta created by G. Douglas Talbott. Talbott helped organize and served as past president of the American Society of Addiction Medicine (ASAM) and was a formative figure in the American Medical Association’s (AMA’s) Impaired Physician Program. He has owned and directed a number of treatment facilities for impaired professionals, most recently the Talbott Recovery Campus in Atlanta, one of the preferred referrals for physicians ordered into evaluation and treatment by licensing boards.
After creating the DeKalb County Impaired Physicians Committee for the Medical Association of Georgia, Talbott founded the Georgia Disabled Doctors Program in 1975 in part because “traditional one-month treatment programs are inadequate for disabled doctors.” According to Talbott, rehabilitation programs that evaluate and treat the rest of the population for substance abuse issues are incapable of doing so in doctors as they are unlike others. He bases this uniqueness on “incredibly high denial”, and what he calls the “four MDs,” “M-Deity”, “Massive Denial” “Militant Defensiveness”, and “More Drugs.”30
Contingency Management = Extortion Using Medical License
According to Talbott, “impaired doctors must first acknowledge their addiction and overcome their ‘terminal uniqueness’ before they can deal with a drug or alcohol problem.” “Terminal uniqueness “ is a phrase Talbott uses to describe doctors’ tendency to think they can heal themselves. “M-Deity” refers to doctors “being trained to think they’re God,”31 an unfounded generalization considering the vast diversity of individuals that make up our profession. This attitude, according to some critics, stems from the personal histories of the treatment staff, including Talbott, who are recovering alcoholics and addicts themselves. One such critic was Assistant Surgeon General under C. Everett Koop John C. Duffy who said that Ridgeview suffered from a “boot-camp mentality” toward physicians under their care and “assume every physician suffering from substance abuse is the same lying, stealing, cheating, manipulating individual they were when they had the illness. Certainly some physicians are manipulative, but it’s naïve to label all physicians with these problems.”32
American Society of Addiction Medicine (ASAM) President (1981-1983) LeClair Bissell was also highly critical of Talbott’s approach. Bissell, co-author of the first textbook of ethics for addiction professionals33 when asked if there was any justification to the claim that doctors are sicker than other people and more vulnerable to addiction replied:
“Well, based on my treatment experience, I think they are less sick and much easier to treat than many other groups. I think one reason for that is that in order to become a physician…one has to have jumped over a great many hurdles. One must pass the exams, survive the screening tests and the interviews, be able to organize oneself well enough to do examinations and so on, and be observed by a good many colleagues along the way. Therefore I think the more grossly psychotic, or sicker, are frequently screened out along the way. The ones we get in treatment are usually people who are less brain-damaged, are still quite capable of learning, are reasonably bright. Not only that, but they are quite well motivated in most cases to hang on to their licenses, the threat of the loss of which is frequently what puts them in treatment in the first place. So are they hard to treat? No! Are they easy patients? Yes! Are they more likely to be addicted than other groups? We don’t know.”34
“I’m not much for the bullying that goes along with some of these programs,” Bissell commented to the Atlanta Journal and Constitution in 1987.31 The constitution did a series of reports after five inpatients committed suicide during a four-year period at Ridgeview.35 In addition there were at least 20 more who had killed themselves over the preceding 12 years after leaving the treatment center.32
Bissell, the recipient of the 1997 Elizabeth Blackwell Award for outstanding contributions to the cause of women and medicine remarked: “When you’ve got them by the license, that’s pretty strong leverage. You shouldn’t have to pound on them so much. You could be asking for trouble.”31According to Bissell: “There’s a lot of debate in the field over whether treatment imposed by threats is worthwhile…To a large degree a person has to seek the treatment on his own accord before it will work for him.”31
A jury awarded $1.3 million to the widow of one of the deceased physicians against Ridgeview,36 and other lawsuits initiated on behalf of suicides were settled out of court.35
The Constitution reported that doctors entered the program under threats of loss of licensure “even when they would prefer treatment that is cheaper and closer to home.” 37 The paper also noted that Ridgeview “enjoys unparalleled connections with many local and state medical societies that work with troubled doctors,” “licensing boards often seek recommendations from such groups in devising an approved treatment plan,” and those in charge are often “physicians who themselves have successfully completed Ridgeview’s program.”37
The cost of a 28-day program for nonprofessionals at Ridgeview in 1987 was $10,000 while the cost was “higher for those going through impaired-health professionals program,” which lasted months rather than 28 days.32
In 1997 William L. White interviewed Bissell whom he called “one of the pioneers in the treatment of impaired professionals.” The interview was not published until after hear death in 2008 per her request. Noting her book Alcoholism in the Professions38 “remains one of the classics in the field”, White asked her when those in the field began to see physicians and other professionals as a special treatment population. She replied:
“When they started making money in alcoholism. As soon as insurance started covering treatment, suddenly you heard that residential treatment was necessary for almost everybody. And since alcoholic docs had tons of money compared to the rest of the public, they not only needed residential treatment, they needed residential treatment in a special treatment facility for many months as opposed to the shorter periods of time that other people needed.”39
Talbott claimed a “92.3 percent recovery rate, according to information compiled from a five-year follow-up survey based on complete abstinence and other treatment.”40
“There is nothing special about a doctor’s alcoholism,” said Bissel
“these special facilities will tell you that they come up with really wonderful recovery rates. They do. And the reason they do is that any time you can grab a professional person by the license and compel him or her into treatment and force them to cooperate with that treatment and then monitor them for years, you’ll get good outcomes—in the high 80s or low 90s in recovery rates—no matter what else you do.”39
“The ones I think are really the best ones were not specialized. There were other well-known specialty clinics that claimed all the docs they treated got well, which is sheer rot. They harmed a great many people, keeping them for long, unnecessary treatments and seeing to it that they hit their financial bottom for sure: kids being yanked out of college, being forced to sell homes to pay for treatment, and otherwise being blackmailed on the grounds that your husband has a fatal disease. It’s ugly.”39
Stanton Peele’s “In the Belly of the American Society of Addiction Medicine Beast” describes the coercion, bullying, threats and indoctrination that are standard operating procedure in Talbott’s facilities.41 Uncooperative patients, “and this covers a range of sins of commission or omission including offering one’s opinion about one’s treatment,” are “threatened with expulsion and with not being certified-or advocated for with their Boards.”41 The cornerstone of treatment is 12-step spiritual recovery. All new patients are indoctrinated into A.A. and coerced to confess they are addicts or alcoholics. Failure to participate in A.A. and 12-step spirituality means expulsion from the program with the anticipated result being loss of one’s medical license.
Fraud, Malpractice, False Diagnoses and False imprisonment
In May 1999 Talbott stepped down as president of the American Society of Addiction Medicine (ASAM) as a jury awarded Dr. Leonard Masters a judgment of $1.3 million in actual damages and an undisclosed sum in punitive damages for fraud, malpractice, and the novel claim of false imprisonment.42 The fraud finding required a finding that errors in the diagnosis were intentional. After being accused of excessive prescribing of narcotics to his chronic pain patients, Masters was told by the director of the Florida PHP that he could either surrender his medical license until the allegations were disproved or submit to a four-day evaluation. Masters agreed to the latter, thinking he would have an objective and fair evaluation, but was instead diagnosed as “alcohol dependent” and coerced into the Talbott recovery program. He was forced to stay in the program under threat of his medical license as staff would routinely threaten to report any doctor who questioned any aspect of their diagnosis or treatment to their state medical boards “as being an impaired physician, leaving necessary treatment against medical advice”42 which would mean the loss of his licensure. However, Masters was not an alcoholic. According to his attorney, Eric. S. Block, “No one ever accused him of having a problem with alcohol. Not his friends, not his wife, not his seven children, not his fellow doctors, not his employees, not his employers, No one.” 43 He was released 4 months later and forced to sign a five-year “continuing care” contract with the PHP, also under continued threat of his medical license. Talbott faced no professional repercussions and no changes in the treatment protocols were made. Talbott continued to present himself and ASAM as the most qualified advocate for the assessment and treatment of medical professionals for substance abuse and addiction up until his death last year.44
Same System Imposed on Doctors Today—Institutional Injustice Worse due to Laboratory Developed Tests. Fortified Scaffold and Tightened the Noose.
In almost all states today any physician referred for an assessment for substance abuse will be mandated to do so in a facility just like Ridgeview. There is no choice. There is one difference however. When the Ridgeview suicides occurred the plethora of laboratory developed tests were not yet introduced. A decade ago Dr. Gregory Skipper introduced the first laboratory developed test for forensic testing and used it on doctors in physician health programs. These non-FDA approved tests of unknown validity presented a new unpredictable variable into the mix with a positive test necessitating another assessment at an out of state treatment facility—a “PHP-approved” assessment facility. The addition of this laboratory Russian Roulette renders the current system much worse than it was at the time of the Ridgeview suicides.
And if a positive test occurs there are no safeguards protecting the donor. LDTs are unregulated by the FDA. There is no oversight and no one to file a complaint with.
In addition the PHPs have no oversight by the medical boards, departments of health or medical societies. They police themselves. The PHPs have convinced law enforcement that when it comes to doctors it is a “parochial issue” best handled by the medical community. I have been hearing from doctors all over the country who have tried to report crimes to the local police, the state Attorney General and other law enforcement agencies only to be turned back over to the very perpetrators of the crimes. “He’s a sick doctor, we’ll take care of him.” The “swift and certain consequences” of this are an effective means of keeping the rest of the inmates silent. Likewise doctors have been going to the media only to have the door slammed in their faces because the media has generally bought in to the “impaired” and “disruptive” physician construct these same people developed through propaganda, misinformation and moral panics and crusades.
Urgent Need to Admit to the Problem
There has been an increase in physician suicide in the past decade. By my estimate the numbers are going to be far higher than the oft-cited 400 per year. The speculation as to cause has been unenlightening and in fact frustrating. Knowledge of anatomy, access to dangerous drugs, increased workload and even student loans have been proposed as contributing factors. Although there has been some tangential mention of physician health programs it has been indirect. Direct and defined discussion is necessary and state PHPs need to be named as a possible contributor to suicide. Admitting the possibility there is a problem is the first crucial step in defining and addressing the problem. The 1980s historical precedent is correlated with physician suicide. The current system is not only based on Ridgeview but has been fortified in scope and power. The physician health movement has effectively removed due process from doctors while removing answerability and accountability from themselves. And they have not only fortified the scaffold but widened it from substance abusing doctors to all doctors. “Potential impairment” and “relapse without use” were introduced without any meaningful resistance and they are now using a panoply of non-FDA approved laboratory developed tests of unknown validity to test for substances of abuse in a zero-tolerance abstinence based monitoring program. With no regulatory oversight the stage is set not only for error but misuse as witch-pricking devices for punishment and control. Doctors across the country are complaining of the very same abuses Leonard Masters did–false diagnoses, misdiagnosis, unneeded treatment and fraud.
In summary, any doctor who is referred to their state PHP today is required to have any assessment and treatment at a “PHP-approved” facility based on Ridgeview. It is mandated. There is no choice. Coercion, control and abuse at Ridgeview was associated with multiple suicides in doctors in the 1980s. The use of non-FDA approved tests of unknown validity worsens the abuse and fits the “cry of pain” model of hopelessness, helplessness and despair. Locus of control is lost. Organizational justice is absent.
The temporal relationship is clear.
Why is this still the elephant in the room?
This needs to be named, defined and openly discussed and debated. How many more must die before we speak up?
Please help me get the conversation going.

They can be a terror to your mind and show you how to hold your tongue
They got mystery written all over their forehead
They kill babies in the crib and say only the good die young
They don’t believe in mercy
Judgement on them is something that you’ll never see
They can exalt you up or bring you down main route
Turn you into anything that they want you to be–Bob Dylan, Foot of Pride
Although no reliable statistics yet exist, anecdotal reports suggest a marked rise in physician suicide in recent years. From the reports I am receiving it is a lot more than the oft cited “medical school class” of 400 per year.
This necessitates an evaluation of predisposing risk factors such as substance abuse and depression, but also requires a critical examination of what external forces may be involved in the descent from suicidal ideation to suicidal planning to completed suicide. What are the cumulative situational and psychosocial factors in physicians that make suicide a potential option and what acute events precipitate the final act?
Depression and Substance Abuse no Different from General Population
The prevalence of depression in physicians is close to that of the general population 1,2 and, if one looks critically at the evidence based literature, substance abuse in medical professionals approximates that of the general population. Controlled studies using DSM diagnostic criteria indicate that physicians have the same rates (8-14%) of substance abuse and dependence as the general population,3 and slightly lower rates compared to other occupations.4,5 Epidemiological surveys reveal the same. Hughes, et al.6 reported a lifetime prevalence of drug or alcohol abuse or dependence in physicians of 7.9%, markedly less than the 14.6% prevalence reported in the general population by Kessler.7
Job Stress and Untreated Mental Illness Risk Factors
Job stress coupled with inadequate treatment for mental illness may be factors contributing to physician suicide according to one recent study. Using data from the National Violent Death Reporting System, Gold, Sen, & Schwenk, 2013 8 compared 203 physicians who had committed suicide to more than 31,000 non-physicians and found that having a known mental health disorder or a job problem that contributed to the suicide significantly predicted being a physician. Physicians were 3.12 times more likely to have a job problem as a contributing factor. In addition, toxicology testing showed low rates of medication treatment. The authors concluded that inadequate treatment and increased problems related to job stress are potentially modifiable risk factors to reduce suicidal death among physicians. They also warned that the database used likely underestimated physician suicides because of “underreporting and even deliberate miscoding because of the stigma attached.”8
Few studies have evaluated the psychosocial stressors surrounding physician suicide but there is no reason to believe they are any different from the rest of the population. Although the triggering life events and specific stressors may vary outside, the inner psyche and undercurrent of thoughts and feelings should remains the same. Perhaps the same drivers of suicide identified in other populations are contributing to physician suicide.
Perceived Helplessness, Hopelessness, Bullying and Defeat
Perceived helplessness is significantly associated with suicide as is9 Hopelessness10,11 Bullying is known to be a predominant trigger for adolescent suicide12-14 One study found that adolescents in custody who were bullied were 9.22 times more likely to attempt suicide than those were not bullied.15
Heightened perceptions of defeat and entrapment are known to be powerful contributors to suicide.16,17 The “Cry of Pain” model 18,19 specifies that people are particularly prone to suicide when life experiences are interpreted as signaling defeat which is defined as a sense of “failed struggle” or loss of social position and resources.. The person is unable to identify an escape from or resolution to a defeating situation, a sense of entrapment proliferates with the perception of no way out, and this provides the central impetus for ending ones life. There is a helplessness and hopelessness that precipitates the descent from ideation, to planning, and then to finality.
Organizational Justice Important Protective Factor
In a study on Italian and Swedish female physicians, degrading experiences and harassment at work were found to be the most powerful independent variables contributing to suicidal thoughts.20 Degrading work experiences harassment, and lack of control over working conditions were found to be associated with suicidal thoughts among Italian and Swedish male university physicians.21
Evidence exists for the role of rescue factors (i.e. social support) as buffers against suicide in the face of varying degrees of life stress.22,23 The study of female physicians revealed meetings to discuss stressful work experiences as a potential protective factor, 20 and support at work when difficulties arose appeared to be a protective factor for the male physicians.21 In line with this, studies of Finnish physicians found that control over one’s work and organizational justice were the most important determinants of work-related wellbeing.24,25 Organizational justice has been identified as a psychosocial predictor of health and wellbeing26 27 Low organizational justice has been identified as a notable risk factor for psychological distress and depression.28,29
Historical Precedent-the Suicides at Ridgeview
Could these factors be playing a role in physician suicide? They evidently did at the Ridgeview Institute, a drug and alcohol treatment program for impaired physicians in Metropolitan Atlanta created by G. Douglas Talbott. Talbott helped organize and served as past president of the American Society of Addiction Medicine (ASAM) and was a formative figure in the American Medical Association’s (AMA’s) Impaired Physician Program. He has owned and directed a number of treatment facilities for impaired professionals, most recently the Talbott Recovery Campus in Atlanta, one of the preferred referrals for physicians ordered into evaluation and treatment by licensing boards.
After creating the DeKalb County Impaired Physicians Committee for the Medical Association of Georgia, Talbott founded the Georgia Disabled Doctors Program in 1975 in part because “traditional one-month treatment programs are inadequate for disabled doctors.” According to Talbott, rehabilitation programs that evaluate and treat the rest of the population for substance abuse issues are incapable of doing so in doctors as they are unlike others. He bases this uniqueness on “incredibly high denial”, and what he calls the “four MDs,” “M-Deity”, “Massive Denial” “Militant Defensiveness”, and “More Drugs.”30
Contingency Management = Extortion Using Medical License
According to Talbott, “impaired doctors must first acknowledge their addiction and overcome their ‘terminal uniqueness’ before they can deal with a drug or alcohol problem.” “Terminal uniqueness “ is a phrase Talbott uses to describe doctors’ tendency to think they can heal themselves. “M-Deity” refers to doctors “being trained to think they’re God,”31 an unfounded generalization considering the vast diversity of individuals that make up our profession. This attitude, according to some critics, stems from the personal histories of the treatment staff, including Talbott, who are recovering alcoholics and addicts themselves. One such critic was Assistant Surgeon General under C. Everett Koop John C. Duffy who said that Ridgeview suffered from a “boot-camp mentality” toward physicians under their care and “assume every physician suffering from substance abuse is the same lying, stealing, cheating, manipulating individual they were when they had the illness. Certainly some physicians are manipulative, but it’s naïve to label all physicians with these problems.”32
American Society of Addiction Medicine (ASAM) President (1981-1983) LeClair Bissell was also highly critical of Talbott’s approach. Bissell, co-author of the first textbook of ethics for addiction professionals33 when asked if there was any justification to the claim that doctors are sicker than other people and more vulnerable to addiction replied:
“Well, based on my treatment experience, I think they are less sick and much easier to treat than many other groups. I think one reason for that is that in order to become a physician…one has to have jumped over a great many hurdles. One must pass the exams, survive the screening tests and the interviews, be able to organize oneself well enough to do examinations and so on, and be observed by a good many colleagues along the way. Therefore I think the more grossly psychotic, or sicker, are frequently screened out along the way. The ones we get in treatment are usually people who are less brain-damaged, are still quite capable of learning, are reasonably bright. Not only that, but they are quite well motivated in most cases to hang on to their licenses, the threat of the loss of which is frequently what puts them in treatment in the first place. So are they hard to treat? No! Are they easy patients? Yes! Are they more likely to be addicted than other groups? We don’t know.”34
“I’m not much for the bullying that goes along with some of these programs,” Bissell commented to the Atlanta Journal and Constitution in 1987.31 The constitution did a series of reports after five inpatients committed suicide during a four-year period at Ridgeview.35 In addition there were at least 20 more who had killed themselves over the preceding 12 years after leaving the treatment center.32
Bissell, the recipient of the 1997 Elizabeth Blackwell Award for outstanding contributions to the cause of women and medicine remarked: “When you’ve got them by the license, that’s pretty strong leverage. You shouldn’t have to pound on them so much. You could be asking for trouble.”31 According to Bissell: “There’s a lot of debate in the field over whether treatment imposed by threats is worthwhile…To a large degree a person has to seek the treatment on his own accord before it will work for him.”31
A jury awarded $1.3 million to the widow of one of the deceased physicians against Ridgeview,36 and other lawsuits initiated on behalf of suicides were settled out of court.35
The Constitution reported that doctors entered the program under threats of loss of licensure “even when they would prefer treatment that is cheaper and closer to home.” 37 The paper also noted that Ridgeview “enjoys unparalleled connections with many local and state medical societies that work with troubled doctors,” “licensing boards often seek recommendations from such groups in devising an approved treatment plan,” and those in charge are often “physicians who themselves have successfully completed Ridgeview’s program.”37
The cost of a 28-day program for nonprofessionals at Ridgeview in 1987 was $10,000 while the cost was “higher for those going through impaired-health professionals program,” which lasted months rather than 28 days.32
In 1997 William L. White interviewed Bissell whom he called “one of the pioneers in the treatment of impaired professionals.” The interview was not published until after hear death in 2008 per her request. Noting her book Alcoholism in the Professions38 “remains one of the classics in the field”, White asked her when those in the field began to see physicians and other professionals as a special treatment population. She replied:
“When they started making money in alcoholism. As soon as insurance started covering treatment, suddenly you heard that residential treatment was necessary for almost everybody. And since alcoholic docs had tons of money compared to the rest of the public, they not only needed residential treatment, they needed residential treatment in a special treatment facility for many months as opposed to the shorter periods of time that other people needed.”39
Talbott claimed a “92.3 percent recovery rate, according to information compiled from a five-year follow-up survey based on complete abstinence and other treatment.”40
“There is nothing special about a doctor’s alcoholism,” said Bissel
“these special facilities will tell you that they come up with really wonderful recovery rates. They do. And the reason they do is that any time you can grab a professional person by the license and compel him or her into treatment and force them to cooperate with that treatment and then monitor them for years, you’ll get good outcomes—in the high 80s or low 90s in recovery rates—no matter what else you do.”39
“The ones I think are really the best ones were not specialized. There were other well-known specialty clinics that claimed all the docs they treated got well, which is sheer rot. They harmed a great many people, keeping them for long, unnecessary treatments and seeing to it that they hit their financial bottom for sure: kids being yanked out of college, being forced to sell homes to pay for treatment, and otherwise being blackmailed on the grounds that your husband has a fatal disease. It’s ugly.”39
Stanton Peele’s “In the Belly of the American Society of Addiction Medicine Beast” describes the coercion, bullying, threats and indoctrination that are standard operating procedure in Talbott’s facilities.41 Uncooperative patients, “and this covers a range of sins of commission or omission including offering one’s opinion about one’s treatment,” are “threatened with expulsion and with not being certified-or advocated for with their Boards.”41 The cornerstone of treatment is 12-step spiritual recovery. All new patients are indoctrinated into A.A. and coerced to confess they are addicts or alcoholics. Failure to participate in A.A. and 12-step spirituality means expulsion from the program with the anticipated result being loss of one’s medical license.
Fraud, Malpractice, False Diagnoses and False imprisonment
In May 1999 Talbott stepped down as president of the American Society of Addiction Medicine (ASAM) as a jury awarded Dr. Leonard Masters a judgment of $1.3 million in actual damages and an undisclosed sum in punitive damages for fraud, malpractice, and the novel claim of false imprisonment.42 The fraud finding required a finding that errors in the diagnosis were intentional. After being accused of excessive prescribing of narcotics to his chronic pain patients, Masters was told by the director of the Florida PHP that he could either surrender his medical license until the allegations were disproved or submit to a four-day evaluation. Masters agreed to the latter, thinking he would have an objective and fair evaluation, but was instead diagnosed as “alcohol dependent” and coerced into the Talbott recovery program. He was forced to stay in the program under threat of his medical license as staff would routinely threaten to report any doctor who questioned any aspect of their diagnosis or treatment to their state medical boards “as being an impaired physician, leaving necessary treatment against medical advice”42 which would mean the loss of his licensure. However, Masters was not an alcoholic. According to his attorney, Eric. S. Block, “No one ever accused him of having a problem with alcohol. Not his friends, not his wife, not his seven children, not his fellow doctors, not his employees, not his employers, No one.” 43 He was released 4 months later and forced to sign a five-year “continuing care” contract with the PHP, also under continued threat of his medical license. Talbott faced no professional repercussions and no changes in the treatment protocols were made. Talbott continued to present himself and ASAM as the most qualified advocate for the assessment and treatment of medical professionals for substance abuse and addiction up until his death last year.44
Same System Imposed on Doctors Today—Institutional Injustice Worse due to Laboratory Developed Tests. Fortified Scaffold and Tightened the Noose.
In almost all states today any physician referred for an assessment for substance abuse will be mandated to do so in a facility just like Ridgeview. There is no choice. There is one difference however. When the Ridgeview suicides occurred the plethora of laboratory developed tests were not yet introduced. A decade ago Dr. Gregory Skipper introduced the first laboratory developed test for forensic testing and used it on doctors in physician health programs. These non-FDA approved tests of unknown validity presented a new unpredictable variable into the mix with a positive test necessitating another assessment at an out of state treatment facility—a “PHP-approved” assessment facility. The addition of this laboratory Russian Roulette renders the current system much worse than it was at the time of the Ridgeview suicides.
And if a positive test occurs there are no safeguards protecting the donor. LDTs are unregulated by the FDA. There is no oversight and no one to file a complaint with.
In addition the PHPs have no oversight by the medical boards, departments of health or medical societies. They police themselves. The PHPs have convinced law enforcement that when it comes to doctors it is a “parochial issue” best handled by the medical community. I have been hearing from doctors all over the country who have tried to report crimes to the local police, the state Attorney General and other law enforcement agencies only to be turned back over to the very perpetrators of the crimes. “He’s a sick doctor, we’ll take care of him.” The “swift and certain consequences” of this are an effective means of keeping the rest of the inmates silent. Likewise doctors have been going to the media only to have the door slammed in their faces because the media has generally bought in to the “impaired” and “disruptive” physician construct these same people developed through propaganda, misinformation and moral panics and crusades.
Urgent Need to Admit to the Problem
There has been an increase in physician suicide in the past decade. By my estimate the numbers are going to be far higher than the oft-cited 400 per year. The speculation as to cause has been unenlightening and in fact frustrating. Knowledge of anatomy, access to dangerous drugs, increased workload and even student loans have been proposed as contributing factors. Although there has been some tangential mention of physician health programs it has been indirect. Direct and defined discussion is necessary and state PHPs need to be named as a possible contributor to suicide. Admitting the possibility there is a problem is the first crucial step in defining and addressing the problem. The 1980s historical precedent is correlated with physician suicide. The current system is not only based on Ridgeview but has been fortified in scope and power. The physician health movement has effectively removed due process from doctors while removing answerability and accountability from themselves. And they have not only fortified the scaffold but widened it from substance abusing doctors to all doctors. “Potential impairment” and “relapse without use” were introduced without any meaningful resistance and they are now using a panoply of non-FDA approved laboratory developed tests of unknown validity to test for substances of abuse in a zero-tolerance abstinence based monitoring program. With no regulatory oversight the stage is set not only for error but misuse as witch-pricking devices for punishment and control. Doctors across the country are complaining of the very same abuses Leonard Masters did–false diagnoses, misdiagnosis, unneeded treatment and fraud.
In summary, any doctor who is referred to their state PHP today is required to have any assessment and treatment at a “PHP-approved” facility based on Ridgeview. It is mandated. There is no choice. Coercion, control and abuse at Ridgeview was associated with multiple suicides in doctors in the 1980s. The use of non-FDA approved tests of unknown validity worsens the abuse and fits the “cry of pain” model of hopelessness, helplessness and despair. Locus of control is lost. Organizational justice is absent.
The temporal relationship is clear.
Why is this still the elephant in the room?
This needs to be named, defined and openly discussed and debated. How many more must die before we speak up?
Please help me get the conversation going.
Mainstream Media, Societal Beliefs and Perceived Authority
Iris Martyn’s article below concerns mainstream media bias and the powerful role social media can play in combatting it. Tangential dissident voices often go unheard (or are silenced) when they oppose perceived authority or mainstream societal beliefs and majority mores.
Martyn gives the example of Suffragettes who were frequently accused of “having ‘magnificently succeeded … in their intention of making themselves a nuisance’, a dismissive claim that covers up the threat” and downplays both the validity of the cause and the character of those behind it.
According to cultural theorist Stuart Hall, the media obtain their information from the primary definers of social reality in authoritative positions and amplify those opinions irrespective of the foundation or veracity of those opinions.
Dissenting voices are all too frequently met with a wall of blinkered apathy or openly dismissed or opposed by mainstream media.
As a result valid complaints and concerns are either unreported, underreported or reported as invalid or misguided hyperbole.

Medscape Article Critical of Physician Health Programs (PHPs) Opens Door to a more focused attack
The importance of a recent article published in Medscape and critical of state Physician Health Programs (PHPs) cannot be overemphasized.
Physician Health Programs- More Harm Than Good? by Pauline Anderson breaks new ground as it is the first mainstream medical publication to address serious and pervasive concerns of the unregulated and unchecked power of these monitoring programs for doctors as an increasing number of reports involving threats, intimidation and fraud come in from doctors across the country.
Originally funded by medical societies and staffed by volunteers, these programs existed in every state by 1980. PHPs are the equivalent of Employee Assistance Programs (EAPs) for other occupations and meet with, assess and monitor doctors who have been referred for substance use or other mental or behavioral health problems.
Over time these programs have been subverted. They have become a power unto themselves. They no longer represent doctors or the public but the interests of the “recovery related racket.” Doctors are being diagnosed with illnesses they don’t have to provide treatment they don’t need all to line the purses of the drug and alcohol testing, assessment and treatment industry and their associates. At the same time doctors who are ill and do need help are not getting the proper treatment. They don’t get better but worse and never return to practice. How many doctors who are perfectly healthy or recovered from illness properly treated are we losing each year to suicide? How many suffer in silence out of fear of being ensnared by these punitive, rigid and one-size fits all programs that claim to exist to protect the public?
PHPs are needed. Doctors who develop problems with addiction or psychiatric problems need to be removed from practice and protect the public, receive treatment until they are healthy enough to return to practice and monitored for a period of time to make sure they remain health. But under current management by the Federation of State Physician Health Programs (FSPHP) this is not happening. PHPs have become Frankenstein’s of coercion, control and abuse that help a few doctors and cause a great deal of harm to the rest. Doctors across the country have been going to local media, law enforcement, the state’s Attorney General, the ACLU and other agencies only to be turned a deaf ear. With the PHP as perceived authority these doctors have been labeled “impaired” and the delegitimization and stigma has prevented their truth from being heard.
To date there have been 187 comments on this article and 301 comments on Dr. Pamela Wible’s related piece entitled “Do Physician Health Programs Increase Physician Suicides?” which was published August 28, 2015 on Medscape and subsequently on KevinMD where it has become the most popular article this week with 243 comments to date. And the consensus so far from reading the more than 700 comments is that PHPs are not only causing harm but serious harm on a large scale. This is by a landslide. The comments raise specific and serious questions that are not being answered by the FSPHP or their sympathizers and apologists.
The FSPHP is tongue-tied in the face of facts and reason as the individual horror stories mount. The testimonials and criticisms are articulate, specific and remarkably similar. It appears to be a rigged game in which all outside opinion is dismissed and no due process exists. Coercion, control, threats, abuse, intimidation and abuse of power are seen crystal clear.
Minor infractions, one-offs, situational problems, anonymous referrals and even false-reports have led doctors into a system in which they have absolutely no control that includes fabricated drug and alcohol tests, diagnosis rigging and unneeded treatment for three months or longer in “PHP-approved” cash only inpatient facilities with close ideological and financial ties to the PHPs. This is political abuse of psychiatry and institutional injustice and it is undoubtedly the cause of the marked increase in physician suicide.
So hats off to Pauline Anderson and Caroline Cassels for having the perspicacity. persistence and courage to shine a light on what was previously ignored or deflected. As a perceived authority the FSPHP and state PHPs believe they are beyond reproach. Specific serious concerns accumulating testimonials of doctors across the country with similar stories are being met with silence and mainstream media need take note of this. We need to shine a larger light in this direction and with dispatch. Sunshine is after all the best disinfectant

By Iris Martyn, Form 6 •
In 1903, outspoken suffragettes “defaced” thousands of one-penny coins by stamping “Votes for Women” onto them and releasing them back into circulation. In fact, ever since complex human social structures came into existence, those who have suffered under their dividing, categorising, and often somewhat arbitrary rules have sought to express themselves in ways that bring to light their humanity and the harsh reality of oppressive conditions.
This occurs at the expense of dissident voices. To continue the earlier example, “Suffragettes on the War Path” were frequently accused of having “magnificently succeeded … in their intention of making themselves a nuisance”, a dismissive claim that covers up the threat felt by male politicians at the thought of universal suffrage, and also downplays the aim of the Suffragettes’ cause, reducing them to nothing more than rowdy troublemakers as far as the media is concerned.
However, this is not a carefully preserved historical phenomenon from the bad old days when societal inequality was present, as opposed to our shining, gender-equal, race-blind present. We cannot describe the times when the oppressed spoke out against the status quo, armed with today’s perfect values and the smugness of hindsight.

When the media outlets cease to present an accurate and unbiased account of events, today’s protestors rely on social media to organise demonstrations, collect evidence of bias, unfair treatment, and eyewitness accounts of injustice.
On the 8th of June, 2014, two right-wing white Neo-Nazis entered a restaurant in Las Vegas, shot two policemen dead, and left a swastika on one of the bodies. This went unreported by Fox News, a major US “news” programme.
On the 9th of August, 2014, an 18-year-old named Michael Brown was shot six times in Ferguson, Missouri, by a police officer in broad daylight. His body lay in the street for several hours. A grand jury chose not to indict his killer. Multiple Fox News hosts were “outraged” at the public anger towards the murderer of an innocent, unarmed boy, as the officer was “doing his job”. The resulting protests from Ferguson’s Black community, during which many civilians were illegally arrested, tear-gassed and shot with rubber-coated metal bullets, were dismissed as having nothing to do with Michael’s murder. Fox News correspondent Rudolph Giuliani, former New York City mayor, claimed that “the racial arsonists … have worked these people up so much with propaganda that facts don’t matter”.
Meanwhile, as support from nearby politicians was lacking, support for Ferguson protestors came, over the internet, from victims of attacks in Palestine. They sent messages of solidarity to the city’s inhabitants, along with advice on how to protect oneself, and recover, from the effects of canisters full of tear gas that were thrown into peaceful protests. As local schools that usually provide a daily meal for schoolchildren closed, a crowdfunding campaign raised $155,000 for the Ferguson foodbank, another raised $130,000 to help Michael Brown’s parents with legal fees, and yet another raised nearly $25,000 to provide college education for his siblings.

Social media was not only used to provide support for the Ferguson community, but to create eyewitness reports on police brutality and racism and to raise public awareness of injustice. In the shooting of yet another young black man, Antonio Martin, witnesses with camera phones documented the mysterious appearance of a gun at the crime scene nearly three hours after his death – planted by the police department. On one tumultuous night of protests, demonstrators moved aside respectfully to allow an ambulance to pass through. As multiple witnesses assert, the ambulance was full of armed police officers, in defiance of international law.
Yet even this is not the most shocking demonstration of the power of the US police force in recent times. In July 2014, a 43-year-old asthmatic black man was put into an illegal chokehold by a police officer in New York City. His head was hit against the pavement multiple times by another officer. Eric Gartner, described as “just a big teddy bear” by his family, shouted “I can’t breathe” six times as he was choked to death. Despite video evidence from multiple bystanders who filmed his murder, unable to do anything else for fear of attack from the police, again a grand jury chose not to indict his killers. The slogan “I can’t breathe” swept the world when the details of this murder were posted on Twitter, sparking worldwide protests.
When national news outlets focused on the possibility that Michael Brown had just robbed a corner store before his death, or that Eric Gartner was a drug addict, in an attempt to justify their deaths, those who were close to the victims used social media, primarily Facebook and Twitter, to speak out against these character assassinations. Michael Brown’s mother spoke about her son’s kind nature, and her difficulty in persuading him to finish high school – black children are much more unlikely to succeed in the US education system.
Eric Gartner’s friends and family spoke about their disappointment in the judicial system, while photographs of his mother wearing an “I can’t breathe” t-shirt to the grand jury hearing circulated quickly over the internet. When a 13-year-old Black boy was shot dead in North California for carrying a BB gun, a white former robber recalled his aspirations to crime on Tumblr, where the police underwent an hour of patient negotiation to convince him to put down his very real firearm, which contrasts with the utter lack of communication with the friendly, innocent, eighth-grader, Andy Lopez.
One image in widespread online circulation is a composition of two different edited versions of a New York Daily News article which describes a violent incident in a subway. In the first version, a woman was “grabbed” by a “hulking brute” who “shoved her onto the platform and began choking her in an unprovoked attack, authorities said”. When the attacker turned out to be a police officer, details of the victim, that provoke sympathy in readers, were removed. Now she was “allegedly put into a bear hug, thrown to the floor, and choked”. The addition of the word “allegedly”, the description of the assault as a “bear hug”, and the use of the passive voice all disassociate the officer from his crime.
The majority of people tend to see social media as a harmless diversion from reality, a way of boasting about one’s achievements or reconnecting with old friends.
It allows them to support one another, collect evidence of injustices that go unreported, humanise the victims of violent crimes, and bring light to the bias and agenda of news corporations.
I can think of nothing more institutionally unjust than an unregulated zero-tolerance monitoring program with no oversight using unregulated drug and alcohol testing of unknown validity. But that is what is occurring. Some of us are trying to expose this corrupt system but barriers exist. As with the Laboratory Developed Tests (LDTs), those involved have intentionally taken steps to remove both answerability and accountability. Both the tests and the body of individuals administering these tests are notable for their lack of transparency, oversight and regulation. This renders them a power unto themselves.
Doctors (and others coerced into Professional Health Programs) across the country have reported going to law enforcement and state agencies only to be turned away. The Federation of State Physician Health Programs (FSPHP) has convinced these outside agencies that this is a “parochial” issue best handled by the medical profession.. Those reporting crimes are turned back over to the very people committing the crimes.
—There is no place in science for consensus or opinion, only evidence.-Claude Bernard
Dear Senator Warren,
Thank you for your reply regarding laboratory developed tests (LDTs) and the need for regulatory oversight. As you mention, LDTs are developed without FDA approval—a pathway in which is not even necessary to prove validity of a test (that it is actually testing what it claims to be testing for) to bring it to market. With no FDA oversight or regulation a commercial lab can claim any validity they want in marketing these tests. The regulation debate has focused on the reliability and validity of a number of clinical tests marketed with unverified claims of accuracy such as prenatal screening and Lyme disease and this lack of oversight is a direct threat to patient safety.
I am sure you would agree with me that the importance of tests diagnostic accuracy is directly proportional to its potential to cause patient harm if reported inaccurately. Sensitivity and specificity are important components of any diagnostic test as there are consequences associated with both false-positive and false negative results.
A test falsely indicating the absence of a condition in someone who truly has it can delay or prevent needed treatment wile a test falsely indicating the presence of a condition in someone who does not truly have it can result in unnecessary testing and treatment.
Incorrect treatment and false labeling of patients can also occur. Therefore diagnostic accuracy is paramount if a test is being used as the basis for further tests and treatment. Any test being used as a basis for further tests or treatment needs to be accurate. It needs to be reliable and valid. Moreover, if the consequences of a test can result in significant patient harm (such as unneeded chemotherapy) it needs to be either 100% accurate or be combined with other tests to confirm the true diagnosis.
“Forensic” vs. “Clinical” Laboratory Testing
“Forensic” testing differs from “clinical” testing because of the consequences and the process is tightly controlled because false-positive results are unacceptable as the consequences can be grave, far-reaching and even permanent.
Forensic testing demands special handling and safeguards to protect the donor such as validated tests, certified labs, strict chain-of-custody procedures and MRO (Medical Review Officer) review. These safeguards of quality control assure the validity and integrity of the specimen. The LDT pathway was not designed for forensic tests.
Forensic Laboratory Developed Tests (LDTs)
Paradoxically, laboratory developed tests with the potential to cause life-changing and possibly irreparable harm have been absent from the regulatory debate; LDT drug and alcohol tests used for “forensic” monitoring purposes.
A panoply of tests using urine, blood, hair, fingernails breath and saliva have been developed and brought to market since 2003 when the first one was introduced by Gregory Skipper, then Medical Director of the Alabama Physicians Health Program, who “convinced the initial lab in the USA, NMS near Philadelphia to start performing EtG testing.” 1
Developed as an LDT, Skipper and NMS then claimed the alcohol biomarker (which was discovered in the 1950s) “appeared to be 100 percent specific” in detecting covert use of alcohol based on a study he coauthored that involved a mere 35 forensic psychiatric inpatients in Germany, all male. 2 With this “evidence-base” and a not yet published paper in the pipeline,3 Skipper then pitched the test to the Federation of State Medical Boards (FSMB) as an accurate and reliable tool detect covert alcohol use in health care professionals.
Policy Entrepreneurship
In “Agendas, Alternatives, and Public Policies,”4 John W. Kingdon describes the problem, policy and political streams involved in public policy making. When these three streams come together a specific problem becomes important on the agenda, policies matching the problem get attention, and then policy change becomes possible.
Kingdon also describes “policy entrepreneurs’ who use their knowledge of the process to further their own policy ends. They ‘lie in wait… with their solutions at hand, waiting for problems to float by to which they can attach their solutions, waiting for a development in the political stream they can use to their advantage.”4
And due to a perfect confluence of streams ( Institute of Medicine report that 44,000 people die each year due to medical error,5 media reports of “impaired physicians,” the the war-on-drugs, etc.) the FSMB was swayed into accepting not just the validity but the necessity of using an alcohol biomarker of unknown reliability and validity on doctors referred to or monitored by state Physician Health Programs (PHPs) .
As the national organization that gives guidance to state medical boards through public policy development and recommendations, the individual state medical boards adopted use of the test without critical appraisal and no meaningful opposition.
Shortly after its founding in 1912, the FSMB began publishing a journal called the Quarterly of the Federation of State Boards of the United States. Now known as the Journal of Medical Regulation, the publication has archived all issues with full articles dating back to 1967 and, as the official journal of the national organization involved in medical licensing and regulation this facilitates an unskewed and impartial examination of how and when specific issues and problems were presented and who presented them and, in doing so, the “policy entrepreneurship” Kingdon describes can be seen quite clearly. For example a 1995 issue containing articles written by the program directors of PHPs in 8 different states contains an FSMB editorial acknowledging the reported 90% success rate claimed of these programs (in part attributed to the 90-day inpatient treatment programs) that concludes:
“Cooperation and communication between the medical boards and the physician health programs must occur in an effort to protect the public while assisting impaired physicians in their recovery.” 6
No one bothered to examine the methodology of these reports to discern the validity of the claims and it is this acceptance of faith without objective assessment that has allowed the passage of flawed public policy in medical regulation.
Nowhere is “policy entrepreneurship” more glaringly displayed as it is in a 2004 issue promoting the use of EtG in monitoring doctors as under the same cover is an article identifying both the need7 for such a test and an article providing the solution.8
“Detection of Alcohol Use in Monitored Aftercare Programs: A National Survey of State Physician Health Programs,” a survey of state Physician Health Programs (PHPs) concludes that “surreptitious alcohol use” is a significant concern” for PHPs, there is no current “best method” for detection, but a promising new test with “exceptional specificity (100 percent) and sensitivity” in detecting small amounts of alcohol for up to 18 hours has recently become available.7
This same issue contains an article authored by Skipper about a new marker “not detectable unless alcohol has been consumed” recently introduced in the United States and now commercially available.”8
Notably absent from both of these articles is Skipper’s role in the commercial availability of the test. This conflict-of-interest is nowhere mentioned in this display of “creating a market then filling it.”
This “regulatory sanctification” of the test implied its tacit approval by the medical profession (i.e. “if they are using it on doctors it must be valid”) and facilitated its marketing to other monitoring agencies (nurses, airline pilots) as well as Courts and Probation Departments where those doing the monitoring had absolute power while those being monitored had no voice.
In Bending Science: How Special Interests Corrupt Public Health Research9, Thomas McGarity and Wendy Wagner describe how special interest groups scheme to advance their own economic or ideological goals by using carefully crafted distorted or “bent” science to influence legal, regulatory and public health policy. The authors describe how those making these decisions often assume the information that reaches them has been sufficiently vetted by the scientific community as it flows through a pipeline of rigorous peer-review and professional oversight and that the final product that exits the pipeline is unbiased and produced in accordance with the norms and procedures of science.
McGarity and Wagner note the serious and sometimes horrific consequences of bent science and provide examples involving Tobacco and Big Pharma . The authors call for:
“..immediate action to reduce the role that bent science plays in regulatory and judicial decision making” and the need for the scientific community to be involved in “designing and implementing reform.”
“Shedding even a little light on how advocates bend policy -relevant science could go a long way toward remedying these problems. Indeed, precisely because the advocates have overtaken the law in this area, heightened attention to the social costs of bending science could itself precipitate significant change.”
In the case of EtG this shedding of light is not very hard as no “carefully crafted” studies bending science were used to sway opinion. None existed. The only items in the pipeline were directly related to Skipper. If anyone dare to look, the Emperor has no clothes.
Lack of Answerability and Accountability
There are difficulties in challenging bent science including a general lack of recognition of the problem and an absence of counter-studies to oppose deliberately manufactured ends-oriented research. This has proven true with the myriad LDTs introduced into the marketplace as no counter-forces or competing economic interests producing counter-studies exist.
Multiple lawsuits, including a class-action, have been decided in favor of the labs who have taken a stand-your-ground approach supported by a body of industry-related “research” they or their affiliates produced to support the validity and reliability of the tests.
Those affected by these tests either have no power or have had their power removed. Most do not have the resources to mount a defense let alone produce counter-studies questioning the reliability and validity of the tests.
Most employee drug testing follows Department of Health and Human Services (DHHS) guidelines using FDA-approved tests that have specific cutoff levels defining a positive-result in an effort to eliminate false-positive results.10 Procedural safeguards are in place in these programs to protect the donor. Forensic testing programs using LDTs provide no such safeguards as the testing is unregulated and there is no oversight from outside actors.
Unlike clinical LDTs “forensic” LDTs are even exempt from CLIA oversight. The only avenue for complaint is through the College of American Pathologists (CAP) and, as an accrediting agency, they can only address problems by ensuring compliance with CAP guidelines. If an investigation concludes lab error or misconduct CAP can mandate the lab correct the test result and come into compliance with their guidelines under threat of loss of accreditation but no other consequences exist. Accountability has been removed yet the consequences to those harmed by these are significant and without remedy.
State Physician Health Programs
As is the case with the LDTs they introduced, Physician Health Programs have no oversight or regulation. A 2013 Audit of the North Carolina PHP 11 prompted by complaints from doctors and performed by State Auditor Beth Woods found absolutely no oversight of the program by either the state medical board or medical society and that “abuse could occur without being detected.”
The Audit also found that doctors were predominantly referred to the same “PHP-approved” out-of-state facilities to which they in part attribute their high success rates in treatment. Interestingly the PHP could not identify what quality indicators or quantitative measurements were used by the PHP to “approve” the “PHP-approved” facilities.
In January of 2015 a Federal class action lawsuit was filed in the Eastern District of Michigan against the state PHP program and found health care providers were subject to the same referral system using these out-of-state facilities. The suit alleges constitutional violations related to the forced medical treatment of health care professionals and the “callous and reckless termination of professional licenses without due process.” 12
As with North Carolina, the Michigan PHP will be unable to provide what quality indicators and quantitative measurements are being used to “qualify” and “approve these facilities. None exist. The sole indicators for approving these assessment centers are ideological and economic. In fact, the medical directors of most, if not all, of these facilities can be seen on this list of “like-minded docs.”
You once said “People feel like the system is rigged against them. And here’s the painful part: they’re right. The system is rigged.”
As the Michigan lawsuit notes: “Unfortunately, a once well-meaning program has turned into a highly punitive and involuntary program where health professionals are forced into extensive and unnecessary substance abuse/dependence treatment under the threat of the arbitrary application of pre-hearing deprivations.”
This has become the rule not the exception. The Federation of State Physician Health Programs (FSPHP), the same group to which Dr. Skipper belongs, has systematically taken over these programs state by state by removing competent and caring doctors not agreeing with the groupthink and silenced them under threat of litigation if they violate their confidentiality agreements and “peer review” statutes.
The same system of coercion, control and abuse exists in Massachusetts. In the past week alone I have heard from a medical student, a resident and two doctors who complained of misconduct misconduct involving fraudulent testing and falsified diagnoses.
In “Ethical and Managerial Considerations Regarding State Physician Health Programs,” published in the Journal of Addiction Medicine in 2012, Drs. John Knight, M.D. and J. Wesley Boyd, M.D., PhD who collectively have more than 20 years experience with the Massachusetts Physician Health Program (PHP) state that:
“Because PHP practices are unknown to most physicians before becoming a client of the PHP, many PHPs operate out- side the scrutiny of the medical community at large. Physicians referred to PHPs are often compromised to some degree, have very little power, and are, therefore, not in a position to voice what might be legitimate objections to a PHP’s practices.”13
Noting that “for most physicians, participation in a PHP evaluation is coercive, and once a PHP recommends monitoring, physicians have little choice but to cooperate with any and all recommendations if they wish to continue practicing medicine,” Knight and Boyd raise serious ethical and managerial questions about current PHP policies and practice including conflicts of interest in referrals for evaluation and treatment, lack of adherence to standards of care for forensic testing of substances of abuse, violations of ethical guidelines in PHP research, and conflicts of interest with state licensing boards.
Knight and Boyd recommend “the broader medical community begin to reassess PHP’s as a whole” and that “consideration be given toward the implementation of independent ethical oversight and establish and appeals process for PHP clients who feel they are being treated unfairly.” 13
They recommend the relationship between PHP’s and the evaluation and treatment centers and licensing boards be transparent and that national standards be developed “that can be debated by all physicians, not just those who work within PHPs.”13
Accountability, or answerability, is necessary to prevent corruption. This requires both the provision of information and justification for actions. What was done and why? Accountability also requires that consequences be imposed on those who engage in misconduct.
In discussing the financial conflicts-of-interest between PHPs and “PHP-approved” assessment centers Knight and Boyd state:
“..if a PHP highlights a physician as particularly problematic, the evaluation center might–whether consciously or otherwise–tailor its diagnosis and recommendations in a way that will support the PHP’s impression of that physician.”
To “consciously tailor a diagnosis” is fraud. It is political abuse of psychiatry. And it is not only the assessment and treatment centers willing to “tailor” a diagnosis; so too are the labs involved.
Physician Suicide
I can think of nothing more institutionally unjust than an unregulated zero-tolerance monitoring program with no oversight using unregulated drug and alcohol testing of unknown validity. But that is what is occurring. Some of us are trying to expose this corrupt system but barriers exist. As with the Laboratory Developed Tests (LDTs), those involved have intentionally taken steps to remove both answerability and accountability. Both the tests and the body of individuals administering these tests are notable for their lack of transparency, oversight and regulation. This renders them a power unto themselves.
Doctors (and others coerced into Professional Health Programs) across the country have reported going to law enforcement and state agencies only to be turned away. The Federation of State Physician Health Programs (FSPHP) has convinced these outside agencies that this is a “parochial” issue best handled by the medical profession.. Those reporting crimes are turned back over to the very people committing the crimes.
The Massachusetts Medical Society and Massachusetts DPH claim no oversight of the Massachusetts PHP, PHS.inc. The Massachusetts Board of Registration in Medicine (BORM) will not address ethical or even criminal complaints about the doctors involved in the PHP and there is good evidence that some members of the BORM are in fact complicit in unethical and even criminal behavior. As the Massachusetts AGO represents the BORM they defer issues back to them and dig no deeper.
Drs. Knight and Boyd have suggested State Audits and we are hoping that MA State Auditor Suzanne Bump will investigate the MA PHP and the Board of Registration in Medicine’s Physician Health and Compliance Unit shortly.
One major problem is that barriers have been put in place to prevent information from getting to the right people.
The majority of people at medical societies, boards, departments of public health and other organizations are individuals of integrity and honesty but the system has been erected so that valid complaints are deflected, delayed, dismissed or otherwise tabled by sympathizers, apologists and those complicity. The criminal activity the Massachusetts PHP is engaging in is undeniable and indefensible but who is going to hold them to account?
It is going to take a while to reform this system of institutional abuse and it has to be done state by state. Please take a look at the facts and documentary evidence and help me hold them accountable. This needs to be exposed, acknowledged and addressed. Doctors are dying from this system of institutional abuse. It is a public health emergency no one is talking about. Yet those behind the PHP programs are claiming this system of coercion, abuse and control is the “gold standard” of addiction treatment and, using another loophole, they want to expand this system to mainstream healthcare.
Sincerely,
Michael L. Langan, M.D.



I can think of nothing more institutionally unjust than an unregulated zero-tolerance monitoring program with no oversight using unregulated drug and alcohol testing of unknown validity. But that is what is occurring. Some of us are trying to expose this corrupt system but barriers exist. As with the Laboratory Developed Tests (LDTs), those involved have intentionally taken steps to remove both answerability and accountability. Both the tests and the body of individuals administering these tests are notable for their lack of transparency, oversight and regulation. This renders them a power unto themselves.
Doctors (and others coerced into Professional Health Programs) across the country have reported going to law enforcement and state agencies only to be turned away. The Federation of State Physician Health Programs (FSPHP) has convinced these outside agencies that this is a “parochial” issue best handled by the medical profession.. Those reporting crimes are turned back over to the very people committing the crimes.
Press Release | Forensic Science Misconduct: A Dark and Cautionary Tale | @csidds.
Originally posted on FORENSICS in FOCUS @ CSIDDS | News and Trends:
Don’t expect a “whodunnit” version of CSI victories in this Op-ed blog article about a darker side of the forensic sciences. It is from an author with ample forensic credentials and experience from both within and outside criminal courts of the US. The article has topics ranging from the continued use of outdated or grossly over hyped “CSI” methods, ethical and moral failures in some forensic groups, to the criminal courts inability to understand much of anything about what is “real ” versus self-serving personal opinion called “science.” A measure of proof confirming these systemic problems is the article’s presenting a glimpse into the multi-million dollar costs to taxpayers for damages won by those wrongfully convicted with the help of court-qualified forensic testimony. Some optimism about better scientific scrutiny is presented but the institutional inertia resisting legitimate change in some forensic organizations, government agencies, and criminal justice institutions is still…
View original 56 more words
I will be putting up a survey shortly and want to hear your stories. One of the recurrent themes I keep hearing from those victimized by PHPs is falsified drug and alcohol tests. Attached is an example of what they are capable of.
Remember, this group has essentially removed themselves from accountability in drug and alcohol testing via the use of Laboratory Developed Tests (LDTs), a loophole which avoids FDA approval and oversight. Whereas most drug testing is transparent and held accountable, the PHPs use testing that is opaque, unregulated and accountable to no one. Accountability demands both the provision of information and justification for ones actions. PHPs block both. While most drug-testing requires the immediate provision of information if the test is questioned (as it should be), PHPs have put forth the logical fallacy that doctors have some sort of inherent expertise in toxicology and pharmacology and can “figure out” how to circumvent the testing process if they were to get copies of their lab results. They block this provision of information. And even if this information is ultimately provided, as seen below, no outside organizations exist to hold them to account. They do not have to justify their actions to anyone. No safeguards exist to assure integrity and honesty of the sample. No safeguards exist to assure the integrity and honesty of those ordering the sample either.
The documents below show forensic fraud. This is undeniable and indefensible. It does not take a toxicologist or Medical Review Officer to understand what “chain-of-custody” is and that “updating” one constitutes misconduct, fraud and (as seen here) criminal activity. These documents were obtained 5 months after a falsified test was ordered by Linda Bresnahan, Director of Operations at Physician Health Services, Inc. (PHS, inc.) the Massachusetts PHP via fax no less. The blood test was drawn on July 1, 2011. On July 19th, 2011 Ms Bresnahan requests (through the PHP secretary Mary Howard) that an already positive test for the alcohol biomarker phosphatidylethanol be “updated” with ID # 1310 and a “chain-of-custody. (which is an oxymoron-a “chain-of-custody” by definition cannot be “updated.” Unveleivably the lab does it without hesitation or any apparent compunction. The documents speak for themselves. ID # 1310 just happens to be my ID number. When I complained that no one ever accused me of ever having an alcohol problem she replied:
“You have an Irish last name-good luck finding anyone who will believe you!”
For a more detailed analysis see here, here and here. And where was the Medical Review Officer during all of this? Good question and one he will not answer! And no one else is holding him to account. This needs to change.
A
B
C
1. Supression of Dissent: Basic Information
2. The keys to backfire
• “Reveal: expose the injustice, challenge cover-up
• Redeem: validate the target, challenge devaluation
• Reframe: emphasize the injustice, counter reinterpretation
• Redirect: mobilize support, be wary of official channels• Resist: stand up to intimidation and bribery”
via Helpful resources for those abused and afraid — via www.bmartin.cc .
 Via the Daily Beast: http://www.thedailybeast.com/articles/2015/03/23/american-doctors-are-killing-themselves-and-no-one-is-talking-about-it.html
Via the Daily Beast: http://www.thedailybeast.com/articles/2015/03/23/american-doctors-are-killing-themselves-and-no-one-is-talking-about-it.html
Excerpt:
“Doctors who acknowledge problems with substances or mental health are typically referred to a physicians health program, or PHP. These organizations evaluate, monitor, and treat physicians. Established initially in the 1970s, PHPs, which exist in almost every state, were intended to divert physicians suffering from alcohol or drug problems from censure from their state medical boards. PHPs are incorporated as nonprofits and have autonomy from the boards. But some PHPs breach confidentiality if they fear a doctor is a danger to the public. And some state medical boards also fund their PHPs. Since the boards hold the keys to licensure, many say this is a conflict of interest.
There are growing concerns about whether PHPs have the right approach to the job. They typically send doctors to rehab programs rooted in the faith-and-abstinence principles of Alcoholics Anonymous. While AA’s 12 steps might work for some with alcohol-use disorders, critics say most PHP recommendations are ill suited for patients with mental health problems.
J. Wesley Boyd, a Harvard psychiatrist who left his post as assistant director of the Massachusetts PHP over a disagreement about practices there, says PHPs routinely intimidate their clients. In an article he co-wrote for the Journal of Addictions Medicine in 2012, Boyd noted that many doctors who seek or are referred by colleagues for treatment are mandated to attend pre-selected rehabilitation facilities for 60 to 90 days. Afterward, they must agree to monitoring and drug testing, typically at their own cost. When doctors resist PHP recommendations, they risk losing their livelihood and their licenses.”
For full article see: http://www.thedailybeast.com/articles/2015/03/23/american-doctors-are-killing-themselves-and-no-one-is-talking-about-it.html
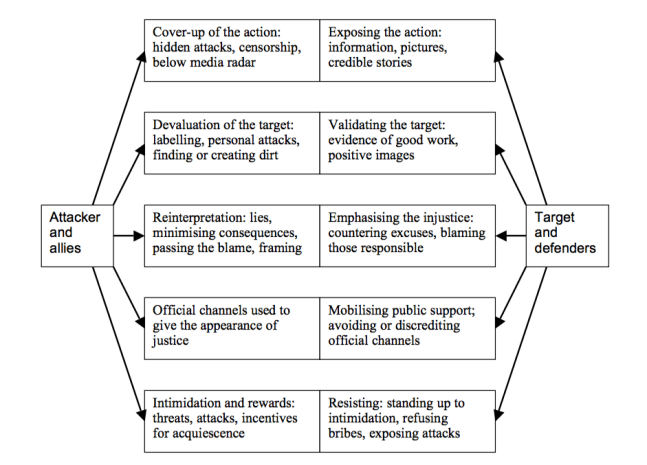 1. Supression of Dissent: Basic Information
1. Supression of Dissent: Basic Information
2. The keys to backfire
• “Reveal: expose the injustice, challenge cover-up
• Redeem: validate the target, challenge devaluation
• Reframe: emphasize the injustice, counter reinterpretation
• Redirect: mobilize support, be wary of official channels• Resist: stand up to intimidation and bribery”
via Helpful resources for those abused and afraid — via www.bmartin.cc .


