They can be a terror to your mind and show you how to hold your tongue
They got mystery written all over their forehead
They kill babies in the crib and say only the good die young
They don’t believe in mercy
Judgement on them is something that you’ll never see
They can exalt you up or bring you down main route
Turn you into anything that they want you to be–Bob Dylan, Foot of Pride

Although no reliable statistics yet exist, anecdotal reports suggest a marked rise in physician suicide in recent years. From the reports I am receiving it is a lot more than the oft cited “medical school class” of 400 per year.
This necessitates an evaluation of predisposing risk factors such as substance abuse and depression, but also requires a critical examination of what external forces may be involved in the descent from suicidal ideation to suicidal planning to completed suicide. What are the cumulative situational and psychosocial factors in physicians that make suicide a potential option and what acute events precipitate the final act?
Depression and Substance Abuse no Different from General Population
The prevalence of depression in physicians is close to that of the general population 1,2 and, if one looks critically at the evidence based literature, substance abuse in medical professionals approximates that of the general population. Controlled studies using DSM diagnostic criteria indicate that physicians have the same rates (8-14%) of substance abuse and dependence as the general population,3 and slightly lower rates compared to other occupations.4,5 Epidemiological surveys reveal the same. Hughes, et al.6 reported a lifetime prevalence of drug or alcohol abuse or dependence in physicians of 7.9%, markedly less than the 14.6% prevalence reported in the general population by Kessler.7
Job Stress and Untreated Mental Illness Risk Factors
Job stress coupled with inadequate treatment for mental illness may be factors contributing to physician suicide according to one recent study. Using data from the National Violent Death Reporting System, Gold, Sen, & Schwenk, 2013 8 compared 203 physicians who had committed suicide to more than 31,000 non-physicians and found that having a known mental health disorder or a job problem that contributed to the suicide significantly predicted being a physician. Physicians were 3.12 times more likely to have a job problem as a contributing factor. In addition, toxicology testing showed low rates of medication treatment. The authors concluded that inadequate treatment and increased problems related to job stress are potentially modifiable risk factors to reduce suicidal death among physicians. They also warned that the database used likely underestimated physician suicides because of “underreporting and even deliberate miscoding because of the stigma attached.”8
Few studies have evaluated the psychosocial stressors surrounding physician suicide but there is no reason to believe they are any different from the rest of the population. Although the triggering life events and specific stressors may vary outside, the inner psyche and undercurrent of thoughts and feelings should remains the same. Perhaps the same drivers of suicide identified in other populations are contributing to physician suicide.
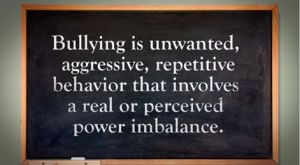
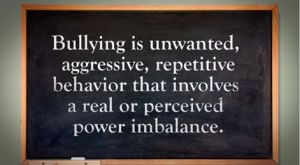
Perceived Helplessness, Hopelessness, Bullying and Defeat
Perceived helplessness is significantly associated with suicide as is9 Hopelessness10,11 Bullying is known to be a predominant trigger for adolescent suicide12-14 One study found that adolescents in custody who were bullied were 9.22 times more likely to attempt suicide than those were not bullied.15
Heightened perceptions of defeat and entrapment are known to be powerful contributors to suicide.16,17 The “Cry of Pain” model 18,19 specifies that people are particularly prone to suicide when life experiences are interpreted as signaling defeat which is defined as a sense of “failed struggle” or loss of social position and resources.. The person is unable to identify an escape from or resolution to a defeating situation, a sense of entrapment proliferates with the perception of no way out, and this provides the central impetus for ending ones life. There is a helplessness and hopelessness that precipitates the descent from ideation, to planning, and then to finality.
Organizational Justice Important Protective Factor
In a study on Italian and Swedish female physicians, degrading experiences and harassment at work were found to be the most powerful independent variables contributing to suicidal thoughts.20 Degrading work experiences harassment, and lack of control over working conditions were found to be associated with suicidal thoughts among Italian and Swedish male university physicians.21
Evidence exists for the role of rescue factors (i.e. social support) as buffers against suicide in the face of varying degrees of life stress.22,23 The study of female physicians revealed meetings to discuss stressful work experiences as a potential protective factor, 20 and support at work when difficulties arose appeared to be a protective factor for the male physicians.21 In line with this, studies of Finnish physicians found that control over one’s work and organizational justice were the most important determinants of work-related wellbeing.24,25 Organizational justice has been identified as a psychosocial predictor of health and wellbeing26 27 Low organizational justice has been identified as a notable risk factor for psychological distress and depression.28,29

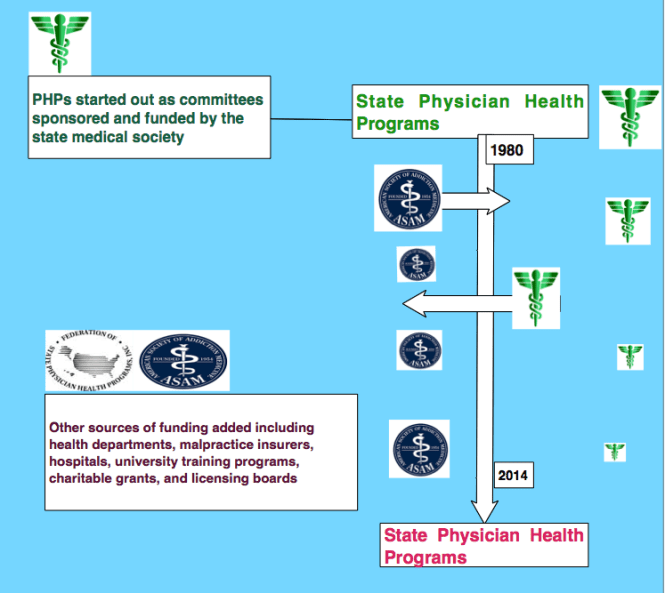
Historical Precedent-the Suicides at Ridgeview
Could these factors be playing a role in physician suicide? They evidently did at the Ridgeview Institute, a drug and alcohol treatment program for impaired physicians in Metropolitan Atlanta created by G. Douglas Talbott. Talbott helped organize and served as past president of the American Society of Addiction Medicine (ASAM) and was a formative figure in the American Medical Association’s (AMA’s) Impaired Physician Program. He has owned and directed a number of treatment facilities for impaired professionals, most recently the Talbott Recovery Campus in Atlanta, one of the preferred referrals for physicians ordered into evaluation and treatment by licensing boards.
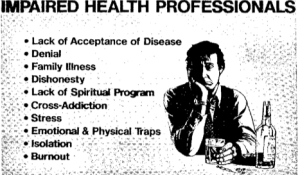
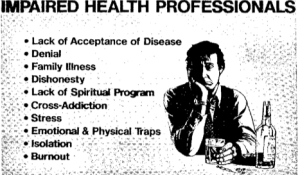
After creating the DeKalb County Impaired Physicians Committee for the Medical Association of Georgia, Talbott founded the Georgia Disabled Doctors Program in 1975 in part because “traditional one-month treatment programs are inadequate for disabled doctors.” According to Talbott, rehabilitation programs that evaluate and treat the rest of the population for substance abuse issues are incapable of doing so in doctors as they are unlike others. He bases this uniqueness on “incredibly high denial”, and what he calls the “four MDs,” “M-Deity”, “Massive Denial” “Militant Defensiveness”, and “More Drugs.”30
Contingency Management = Extortion Using Medical License
According to Talbott, “impaired doctors must first acknowledge their addiction and overcome their ‘terminal uniqueness’ before they can deal with a drug or alcohol problem.” “Terminal uniqueness “ is a phrase Talbott uses to describe doctors’ tendency to think they can heal themselves. “M-Deity” refers to doctors “being trained to think they’re God,”31 an unfounded generalization considering the vast diversity of individuals that make up our profession. This attitude, according to some critics, stems from the personal histories of the treatment staff, including Talbott, who are recovering alcoholics and addicts themselves. One such critic was Assistant Surgeon General under C. Everett Koop John C. Duffy who said that Ridgeview suffered from a “boot-camp mentality” toward physicians under their care and “assume every physician suffering from substance abuse is the same lying, stealing, cheating, manipulating individual they were when they had the illness. Certainly some physicians are manipulative, but it’s naïve to label all physicians with these problems.”32
American Society of Addiction Medicine (ASAM) President (1981-1983) LeClair Bissell was also highly critical of Talbott’s approach. Bissell, co-author of the first textbook of ethics for addiction professionals33 when asked if there was any justification to the claim that doctors are sicker than other people and more vulnerable to addiction replied:
“Well, based on my treatment experience, I think they are less sick and much easier to treat than many other groups. I think one reason for that is that in order to become a physician…one has to have jumped over a great many hurdles. One must pass the exams, survive the screening tests and the interviews, be able to organize oneself well enough to do examinations and so on, and be observed by a good many colleagues along the way. Therefore I think the more grossly psychotic, or sicker, are frequently screened out along the way. The ones we get in treatment are usually people who are less brain-damaged, are still quite capable of learning, are reasonably bright. Not only that, but they are quite well motivated in most cases to hang on to their licenses, the threat of the loss of which is frequently what puts them in treatment in the first place. So are they hard to treat? No! Are they easy patients? Yes! Are they more likely to be addicted than other groups? We don’t know.”34
“I’m not much for the bullying that goes along with some of these programs,” Bissell commented to the Atlanta Journal and Constitution in 1987.31 The constitution did a series of reports after five inpatients committed suicide during a four-year period at Ridgeview.35 In addition there were at least 20 more who had killed themselves over the preceding 12 years after leaving the treatment center.32
Bissell, the recipient of the 1997 Elizabeth Blackwell Award for outstanding contributions to the cause of women and medicine remarked: “When you’ve got them by the license, that’s pretty strong leverage. You shouldn’t have to pound on them so much. You could be asking for trouble.”31 According to Bissell: “There’s a lot of debate in the field over whether treatment imposed by threats is worthwhile…To a large degree a person has to seek the treatment on his own accord before it will work for him.”31
A jury awarded $1.3 million to the widow of one of the deceased physicians against Ridgeview,36 and other lawsuits initiated on behalf of suicides were settled out of court.35
The Constitution reported that doctors entered the program under threats of loss of licensure “even when they would prefer treatment that is cheaper and closer to home.” 37 The paper also noted that Ridgeview “enjoys unparalleled connections with many local and state medical societies that work with troubled doctors,” “licensing boards often seek recommendations from such groups in devising an approved treatment plan,” and those in charge are often “physicians who themselves have successfully completed Ridgeview’s program.”37
The cost of a 28-day program for nonprofessionals at Ridgeview in 1987 was $10,000 while the cost was “higher for those going through impaired-health professionals program,” which lasted months rather than 28 days.32
In 1997 William L. White interviewed Bissell whom he called “one of the pioneers in the treatment of impaired professionals.” The interview was not published until after hear death in 2008 per her request. Noting her book Alcoholism in the Professions38 “remains one of the classics in the field”, White asked her when those in the field began to see physicians and other professionals as a special treatment population. She replied:
“When they started making money in alcoholism. As soon as insurance started covering treatment, suddenly you heard that residential treatment was necessary for almost everybody. And since alcoholic docs had tons of money compared to the rest of the public, they not only needed residential treatment, they needed residential treatment in a special treatment facility for many months as opposed to the shorter periods of time that other people needed.”39
Talbott claimed a “92.3 percent recovery rate, according to information compiled from a five-year follow-up survey based on complete abstinence and other treatment.”40
“There is nothing special about a doctor’s alcoholism,” said Bissel
“these special facilities will tell you that they come up with really wonderful recovery rates. They do. And the reason they do is that any time you can grab a professional person by the license and compel him or her into treatment and force them to cooperate with that treatment and then monitor them for years, you’ll get good outcomes—in the high 80s or low 90s in recovery rates—no matter what else you do.”39
“The ones I think are really the best ones were not specialized. There were other well-known specialty clinics that claimed all the docs they treated got well, which is sheer rot. They harmed a great many people, keeping them for long, unnecessary treatments and seeing to it that they hit their financial bottom for sure: kids being yanked out of college, being forced to sell homes to pay for treatment, and otherwise being blackmailed on the grounds that your husband has a fatal disease. It’s ugly.”39
Stanton Peele’s “In the Belly of the American Society of Addiction Medicine Beast” describes the coercion, bullying, threats and indoctrination that are standard operating procedure in Talbott’s facilities.41 Uncooperative patients, “and this covers a range of sins of commission or omission including offering one’s opinion about one’s treatment,” are “threatened with expulsion and with not being certified-or advocated for with their Boards.”41 The cornerstone of treatment is 12-step spiritual recovery. All new patients are indoctrinated into A.A. and coerced to confess they are addicts or alcoholics. Failure to participate in A.A. and 12-step spirituality means expulsion from the program with the anticipated result being loss of one’s medical license.
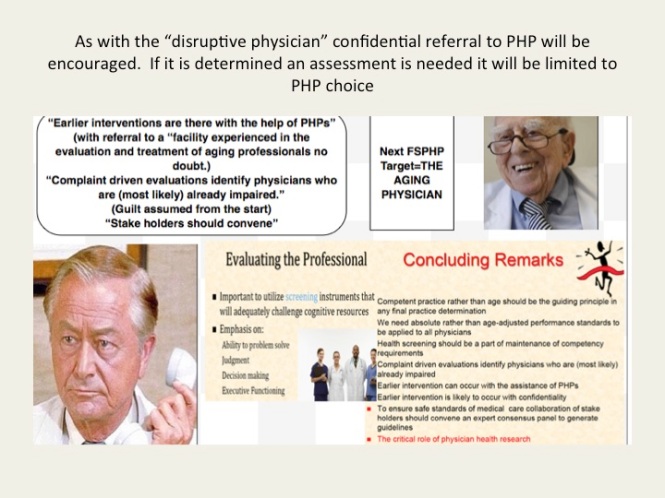
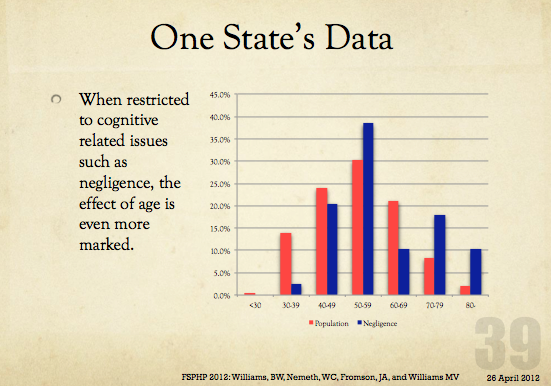
From a talk given by FSPHP
Fraud, Malpractice, False Diagnoses and False imprisonment
In May 1999 Talbott stepped down as president of the American Society of Addiction Medicine (ASAM) as a jury awarded Dr. Leonard Masters a judgment of $1.3 million in actual damages and an undisclosed sum in punitive damages for fraud, malpractice, and the novel claim of false imprisonment.42 The fraud finding required a finding that errors in the diagnosis were intentional. After being accused of excessive prescribing of narcotics to his chronic pain patients, Masters was told by the director of the Florida PHP that he could either surrender his medical license until the allegations were disproved or submit to a four-day evaluation. Masters agreed to the latter, thinking he would have an objective and fair evaluation, but was instead diagnosed as “alcohol dependent” and coerced into the Talbott recovery program. He was forced to stay in the program under threat of his medical license as staff would routinely threaten to report any doctor who questioned any aspect of their diagnosis or treatment to their state medical boards “as being an impaired physician, leaving necessary treatment against medical advice”42 which would mean the loss of his licensure. However, Masters was not an alcoholic. According to his attorney, Eric. S. Block, “No one ever accused him of having a problem with alcohol. Not his friends, not his wife, not his seven children, not his fellow doctors, not his employees, not his employers, No one.” 43 He was released 4 months later and forced to sign a five-year “continuing care” contract with the PHP, also under continued threat of his medical license. Talbott faced no professional repercussions and no changes in the treatment protocols were made. Talbott continued to present himself and ASAM as the most qualified advocate for the assessment and treatment of medical professionals for substance abuse and addiction up until his death last year.44
Same System Imposed on Doctors Today—Institutional Injustice Worse due to Laboratory Developed Tests. Fortified Scaffold and Tightened the Noose.
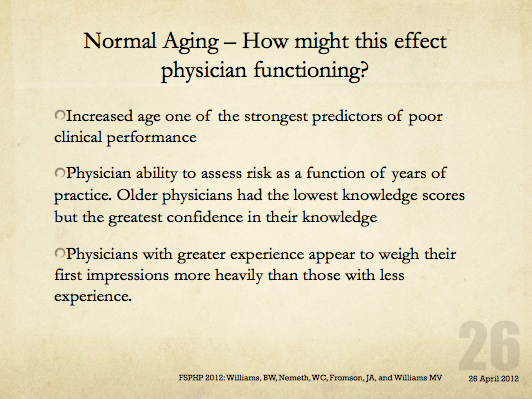
In almost all states today any physician referred for an assessment for substance abuse will be mandated to do so in a facility just like Ridgeview. There is no choice. There is one difference however. When the Ridgeview suicides occurred the plethora of laboratory developed tests were not yet introduced. A decade ago Dr. Gregory Skipper introduced the first laboratory developed test for forensic testing and used it on doctors in physician health programs. These non-FDA approved tests of unknown validity presented a new unpredictable variable into the mix with a positive test necessitating another assessment at an out of state treatment facility—a “PHP-approved” assessment facility. The addition of this laboratory Russian Roulette renders the current system much worse than it was at the time of the Ridgeview suicides.
And if a positive test occurs there are no safeguards protecting the donor. LDTs are unregulated by the FDA. There is no oversight and no one to file a complaint with.
In addition the PHPs have no oversight by the medical boards, departments of health or medical societies. They police themselves. The PHPs have convinced law enforcement that when it comes to doctors it is a “parochial issue” best handled by the medical community. I have been hearing from doctors all over the country who have tried to report crimes to the local police, the state Attorney General and other law enforcement agencies only to be turned back over to the very perpetrators of the crimes. “He’s a sick doctor, we’ll take care of him.” The “swift and certain consequences” of this are an effective means of keeping the rest of the inmates silent. Likewise doctors have been going to the media only to have the door slammed in their faces because the media has generally bought in to the “impaired” and “disruptive” physician construct these same people developed through propaganda, misinformation and moral panics and crusades.

Urgent Need to Admit to the Problem
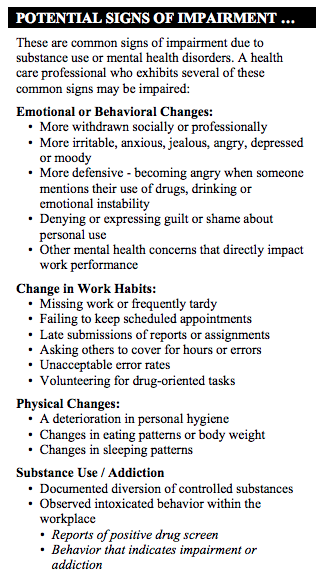
There has been an increase in physician suicide in the past decade. By my estimate the numbers are going to be far higher than the oft-cited 400 per year. The speculation as to cause has been unenlightening and in fact frustrating. Knowledge of anatomy, access to dangerous drugs, increased workload and even student loans have been proposed as contributing factors. Although there has been some tangential mention of physician health programs it has been indirect. Direct and defined discussion is necessary and state PHPs need to be named as a possible contributor to suicide. Admitting the possibility there is a problem is the first crucial step in defining and addressing the problem. The 1980s historical precedent is correlated with physician suicide. The current system is not only based on Ridgeview but has been fortified in scope and power. The physician health movement has effectively removed due process from doctors while removing answerability and accountability from themselves. And they have not only fortified the scaffold but widened it from substance abusing doctors to all doctors. “Potential impairment” and “relapse without use” were introduced without any meaningful resistance and they are now using a panoply of non-FDA approved laboratory developed tests of unknown validity to test for substances of abuse in a zero-tolerance abstinence based monitoring program. With no regulatory oversight the stage is set not only for error but misuse as witch-pricking devices for punishment and control. Doctors across the country are complaining of the very same abuses Leonard Masters did–false diagnoses, misdiagnosis, unneeded treatment and fraud.
In summary, any doctor who is referred to their state PHP today is required to have any assessment and treatment at a “PHP-approved” facility based on Ridgeview. It is mandated. There is no choice. Coercion, control and abuse at Ridgeview was associated with multiple suicides in doctors in the 1980s. The use of non-FDA approved tests of unknown validity worsens the abuse and fits the “cry of pain” model of hopelessness, helplessness and despair. Locus of control is lost. Organizational justice is absent.
The temporal relationship is clear.
Why is this still the elephant in the room?
This needs to be named, defined and openly discussed and debated. How many more must die before we speak up?
Please help me get the conversation going.

- Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Archives of internal medicine. Jul 13 1998;158(13):1422-1426.
- Frank E, Dingle AD. Self-reported depression and suicide attempts among U.S. women physicians. The American journal of psychiatry. Dec 1999;156(12):1887-1894.
- Brewster JM. Prevalence of alcohol and other drug problems among physicians. JAMA : the journal of the American Medical Association. Apr 11 1986;255(14):1913-1920.
- Anthony J, Eaton W, Mandell W, al. e. Psychoactive Drug Dependence and abuse: More Common in Some Occupations than in Others? Journal of Employee Assistance Res. 1992;1:148-186.
- Stinson F, DeBakely S, Steffens R. Prevalence of DSM-III-R Alcohol abuse and/or dependence among selected occupations. Alchohol Health Research World. 1992;16:165-172.
- Hughes PH, Brandenburg N, Baldwin DC, Jr., et al. Prevalence of substance use among US physicians. JAMA : the journal of the American Medical Association. May 6 1992;267(17):2333-2339.
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. Jun 2005;62(6):593-602.
- Gold KJ, Sen A, Schwenk TL. Details on suicide among US physicians: data from the National Violent Death Reporting System. General hospital psychiatry. Jan-Feb 2013;35(1):45-49.
- Rivers I, Noret N. Potential suicide ideation and its association with observing bullying at school. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. Jul 2013;53(1 Suppl):S32-36.
- Lester D, Walker RL. Hopelessness, helplessness, and haplessness as predictors of suicidal ideation. Omega. 2007;55(4):321-324.
- Beck AT. Hopelessness as a predictor of eventual suicide. Annals of the New York Academy of Sciences. 1986;487:90-96.
- Hinduja S, Patchin JW. Bullying, cyberbullying, and suicide. Archives of suicide research : official journal of the International Academy for Suicide Research. 2010;14(3):206-221.
- Hertz MF, Donato I, Wright J. Bullying and suicide: a public health approach. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. Jul 2013;53(1 Suppl):S1-3.
- Kim YS, Leventhal B. Bullying and suicide. A review. International journal of adolescent medicine and health. Apr-Jun 2008;20(2):133-154.
- Kiriakidis SP. Bullying and suicide attempts among adolescents kept in custody. Crisis. 2008;29(4):216-218.
- Taylor PJ, Gooding P, Wood AM, Tarrier N. The role of defeat and entrapment in depression, anxiety, and suicide. Psychological bulletin. May 2011;137(3):391-420.
- Lester D. Defeat and entrapment as predictors of depression and suicidal ideation versus hopelessness and helplessness. Psychological reports. Oct 2012;111(2):498-501.
- Williams JMG. Cry of Pain. Harmondsworth: Penguin; 1997.
- Williams JMG, Crane C, Barnhofer T, Duggan DS. Psychology and suicidal behavior: elaborating the entrapment model. In: Hawton K, ed. Prevention and treatment of suicidal behavior: from science to practice. Oxford: Oxford University Press; 2005:71-89.
- Fridner A, Belkic K, Marini M, Minucci D, Pavan L, Schenck-Gustafsson K. Survey on recent suicidal ideation among female university hospital physicians in Sweden and Italy (the HOUPE study): cross-sectional associations with work stressors. Gender medicine. Apr 2009;6(1):314-328.
- Fridner A, Belkic K, Minucci D, et al. Work environment and recent suicidal thoughts among male university hospital physicians in Sweden and Italy: the health and organization among university hospital physicians in Europe (HOUPE) study. Gender medicine. Aug 2011;8(4):269-279.
- Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: Risks and protectors. Pediatrics. 2001;107(485).
- Clum GA, Febbraro GAR. Stress, social support and problem-solving appraisal/skill: Prediction of suicide severity within a college sample. Journal of Psychopathology and Behavioral Assessment. 1994;16:37-46.
- Lindfors PM, Meretoja OA, Toyry SM, Luukkonen RA, Elovainio MJ, Leino TJ. Job satisfaction, work ability and life satisfaction among Finnish anaesthesiologists. Acta anaesthesiologica Scandinavica. Aug 2007;51(7):815-822.
- Heponiemi T, Kuusio H, Sinervo T, Elovainio M. Job attitudes and well-being among public vs. private physicians: organizational justice and job control as mediators. European journal of public health. Aug 2011;21(4):520-525.
- Elovainio M, Kivimaki M, Vahtera J. Organizational justice: evidence of a new psychosocial predictor of health. Am J Public Health. Jan 2002;92(1):105-108.
- Lawson KJ, Noblet AJ, Rodwell JJ. Promoting employee wellbeing: the relevance of work characteristics and organizational justice. Health promotion international. Sep 2009;24(3):223-233.
- Hayashi T, Odagiri Y, Ohya Y, Tanaka K, Shimomitsu T. Organizational justice, willingness to work, and psychological distress: results from a private Japanese company. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. Feb 2011;53(2):174-181.
- Lang J, Bliese PD, Lang JW, Adler AB. Work gets unfair for the depressed: cross-lagged relations between organizational justice perceptions and depressive symptoms. The Journal of applied psychology. May 2011;96(3):602-618.
- Gonzales L. When Doctors are Addicts: For physicians getting Molly Kellogg is easy. Getting help is not. Chicago Reader. July 28, 1988, 1988.
- King M, Durcanin C. The suicides at Ridgeview Institute: A Doctor’s treatment program may be too tough, some say. Atlanta Journal and Constitution. December 18, 1987a, 1987: A12.
- Durcanin C, King M. The suicides at Ridgeview Institute: Suicides mar success at Ridgeview with troubled professionals. Atlanta Journal and Constitution. December 18, 1987, 1987: A13.
- Bissell L, Royce JE. Ethics for Addiction Professionals. Center City, Minnesota: Hazelden; 1987.
- Addiction Scientists from the USA: LeClair Bissell. In: Edwards G, ed. Addiction: Evolution of a Specialist Field. 1 ed: Wiley, John & Sons, Incorporated; 2002:408.
- Durcanin C. The suicides at Ridgeview Institute: Staff members didn’t believe Michigan doctor was suicidal. Atlanta Journal and Constitution. December 18, 1987, 1987: A8.
- Ricks WS. Ridgeview Institute loses $1.3 million in suit over suicide. Atlanta Journal and Constitution. October 11, 1987, 1987: A1.
- King M, Durcanin C. The suicides at Ridgeview Institute: Many drug-using doctors driven to Ridgeview by fear of losing licenses. Atlanta Journal and Constitution. December 18, 1987b, 1987: A1.
- Bissell L, Haberman PW. Alcoholism in the Professions. Oxford University Press; 1984.
- White W. Reflections of an addiction treatment pioneer. An Interview with LeClair Bissell, MD (1928-2008), conducted January 22, 1997. Posted at http://www.williamwhitepapers.com. 2011.
- Williams c. Health care field chemical dependency threat cited. The Tuscaloosa News. January 16, 1988, 1988: 16.
- Peele S. In the Belly of the American Society of Addiction Medicine Beast. The Stanton Peele Addiction Website (accessed March 28, 2014) http://web.archive.org/web/20080514153437/http://www.peele.net/debate/talbott.html.
- Ursery S. $1.3M verdict coaxes a deal for doctor’s coerced rehab. Fulton County Daily Report. May 12, 1999b 1999.
- Ursery S. I was wrongly held in alcohol center, doctor charges. Fulton Count y Daily Report. April 27, 1999a 1999.
- Parker J. George Talbott’s Abuse of Dr. Leon Masters MD ( http://medicalwhistleblowernetwork.jigsy.com/george-talbott-s-abuse-of-leon-masters ). Medical Whistelblower Advocacy Network.









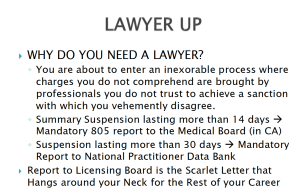










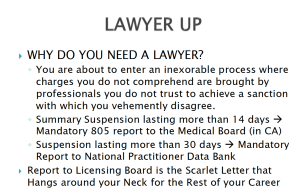
 A Federal class action lawsuit has been filed in the Eastern District of Michigan against the state PHP program alleging constitutional violations related to the forced medical treatment of health care professionals involved in the State’s “Professionals Health Program” (PHP) and the “callous and reckless termination of professional licenses without due process.” According to the complaint:
A Federal class action lawsuit has been filed in the Eastern District of Michigan against the state PHP program alleging constitutional violations related to the forced medical treatment of health care professionals involved in the State’s “Professionals Health Program” (PHP) and the “callous and reckless termination of professional licenses without due process.” According to the complaint: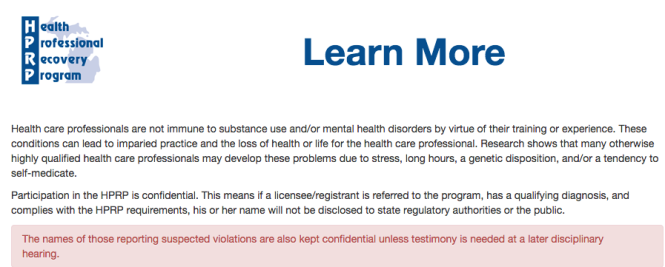
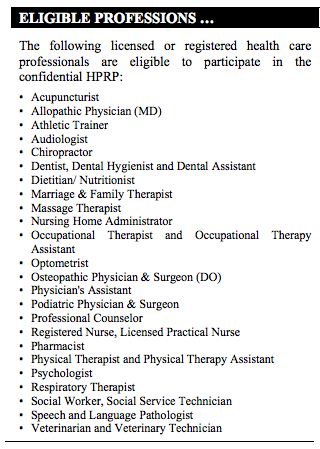 After initial intake with HPRP, the licensee is referred to a “qualified evaluator” and “If the evaluation indicates a substance use and/or mental health disorder that represent a possible impairment” the HPRP makes referrals for treatment services to an “approved provider.
After initial intake with HPRP, the licensee is referred to a “qualified evaluator” and “If the evaluation indicates a substance use and/or mental health disorder that represent a possible impairment” the HPRP makes referrals for treatment services to an “approved provider.