Physician Suicide and the Elephant in the Room
Michael Langan, M.D.
Although no reliable statistics exist, anecdotal reports suggest an alarming upsurge in physician suicide. This necessitates a reappraisal of known predisposing risk factors such as substance abuse and depression but also requires a critical examination of what external forces or vulnerabilities might be unique to doctors and how they might be involved in the descent from suicidal ideation to suicidal planning to completed suicide.
Depression and Substance Abuse Comparable to General Population
Depression and substance abuse are the two biggest risk factors for suicide. The prevalence of depression in physicians is close to that of the general population 1,2 and, if one looks critically at the evidence based literature, substance abuse in medical professionals approximates that of the general population. Controlled studies using DSM diagnostic criteria suggest that physicians have the same rates (8-14%) of substance abuse and dependence as the rest of the population 3 and slightly lower rates compared to other occupations.4,5 Epidemiological surveys reveal the same. Hughes, et al.6 found a lifetime prevalence of drug or alcohol abuse or dependence in physicians of 7.9%, markedly less than the 14.6% prevalence reported in the general population by Kessler.7
State Physician Health Programs
Perhaps it is how physicians are treated differently when they develop a substance abuse or mental health problem.
Physician Health Programs (PHP) can be considered an equivalent to Employee Assistance Programs (EAPs) for other occupations. PHPs meet with, assess and monitor doctors who have been referred to them for substance use or other mental or behavioral health problems. Originally developed as “impaired physician” programs, the PHPs were created to help doctors who developed problems with substance abuse or addiction an alternative to disciplinary action by State Medical Boards. These programs existed in almost every state by 1980. Often staffed by volunteer physicians and funded State Medical Societies, these programs served the dual purpose of helping sick colleagues and protecting the public. Preferring rehabilitation to probation or license revocation so long as the public was protected from imminent danger, most medical boards accepted the concept with support and referrals. Most EAPs were developed with the collaboration of workers unions or some other group supporting the rights and interests of the workers. As there is no such organization representing doctors, PHPs developed in the absence of regulation or oversight. As a consequence there is no meaningful accountability.
In Ethical and Managerial Considerations Regarding State Physician Health Programs published in the Journal of Addiction Medicine in 2012, John Knight, M.D. and J. Wesley Boyd, M.D., PhD who collectively have more than 20 years experience with the Massachusetts PHP state that:
“Because PHP practices are unknown to most physicians before becoming a client of the PHP, many PHPs operate out- side the scrutiny of the medical community at large. Physicians referred to PHPs are often compromised to some degree, have very little power, and are, therefore, not in a position to voice what might be legitimate objections to a PHP’s practices.”8
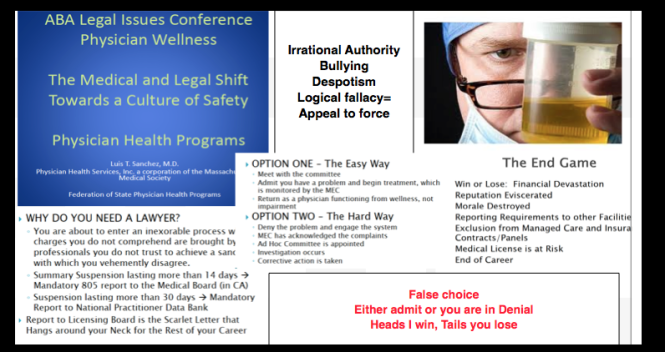
Noting that “for most physicians, participation in a PHP evaluation is coercive, and once a PHP recommends monitoring, physicians have little choice but to cooperate with any and all recommendations if they wish to continue practicing medicine,” Knight and Boyd raise serious ethical and managerial questions about current PHP policies and practice including conflicts of interest in referrals for evaluation and treatment, lack of adherence to standards of care for forensic testing of substances of abuse, violations of ethical guidelines in PHP research, and conflicts of interest with state licensing boards.
Knight and Boyd recommend “that the broader medical community begin to reassess PHP’s as a whole” and that “consideration be given toward the implementation of independent ethical oversight and establish and appeals process for PHP clients who feel they are being treated unfairly.” 8 They also recommend the relationship of PHP’s between the evaluation and treatment centers and licensing boards be transparent and that national organizations review PHP practices and recommend national standards “that can be debated by all physicians, not just those who work within PHPs.”8 Unfortunately this has not happened. Most physicians have no idea that the state physician health programs have been taken over by the “impaired physicians movement.”
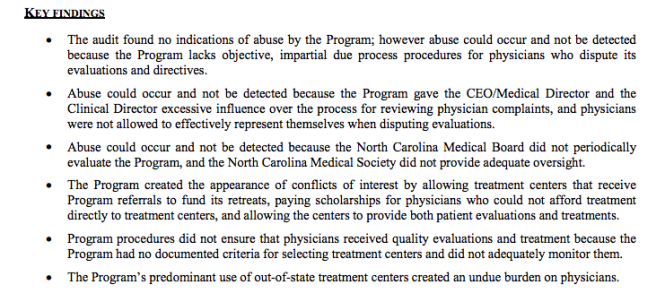
In his Psychology Today blog, Boyd again recommends oversight and regulation of PHPs. He cites the North Carolina Physicians Health Program Audit released in April of 2014 that reported the below key findings:
As with Knight and Boyd’s paper outlining the ethical and managerial problems in PHPs, the NC PHP audit finding that abuse could occur and not be detected generated little interest from either the medical community or the media.
Although state PHPs present themselves as confidential caring programs of benevolence they are essentially monitoring programs for physicians who can be referred to them for issues such as being behind on chart notes. If the PHP feels a doctor is in need of PHP “services” they must then abide by any and all demands of the PHP or be reported to their medical board under threat of loss of licensure.
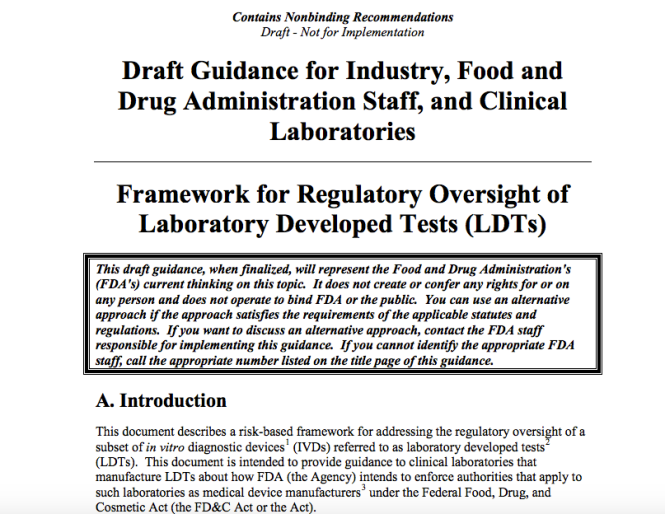
State PHP programs require strict adherence to 12-step doctrine9 yet many of the physicians monitored by them are neither addicts nor alcoholics. Some do not even have substance abuse issues and there are reports of “disruptive” physicians being diagnosed with “character defects” at the “PHP-approved” facilities that do these assessments. PHPs require abstinence from drugs and alcohol yet use non-FDA approved Laboratory Developed Tests in their monitoring programs. Many of these tests were introduced to commercial labs and promoted by ASAM/FSPHP physicians.10-12
LDTs bypass the FDA approval process and have no meaningful regulatory oversight. The LDT pathway was not designed for “forensic” tests but clinical tests with low risk. Some are arguing for regulation and oversight of LDTs due to questionable validity and risk of patient harm.13
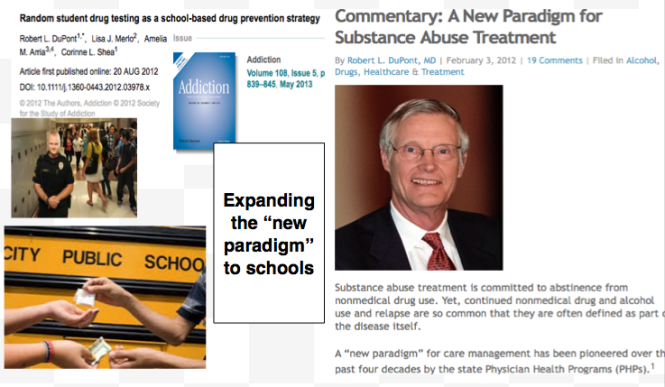
These same physicians are claiming a high success rate for PH programs9 and suggesting that they be used for random testing of all physicians.14
As with LDTs, the state PHPs are unregulated, and without oversight. State medical societies and departments of health have no control over state PHPs.
Their opacity is bolstered by peer-review immunity, HIPPA, HCQIA, and confidentiality agreements. The monitored physician is forced to abide by any and all demands of the PHP no matter how unreasonable-all under the coloration of medical utility and without any evidentiary standard or right to appeal.
The ASAM has a certification process for physicians and claim to be “addiction” specialists. This “board certification” is not recognized by the American Board of Medical Specialties and is not a recognized medical specialty. The goal of the ASAM is to be recognized as the experts in addiction medicine with the consensus expert opinion based on the 12-step prohibitionist brain disease model. The ASAM has aligned itself with a number of inpatient drug treatment centers (Hazelden, Talbott, Marworth, Bradford,etc) and are heavily funded by the drug testing industry. It is in fact a “rigged game.”
State PHPs are non-profit non-governmental organizations and have been granted quasi-governmental immunity by most State legislatures from legal liability.
By infiltrating “impaired physician” programs they have established themselves in almost every state by joining, gaining power, and removing dissenters. Groupthink and 12-step indoctrination are the goals. By advertising as advocates for doctors who are “caring,” “confidential resources,” “giving help,” and advocating for “colleagues in need” the outward appearance is one of benevolence.
The biggest obstacle is that this system allows them to throw the normal rules of conduct under the imperative of a higher goal assumed to trump all other consideration. Those outside of programs either defend or ignore the reports of ethical and criminal violations, complacent in their trust of these “experts” claiming they are just helping sick doctors and protecting the public.
With no oversight or regulatory body involved this is all done with impunity, immunity, and undercover. They use the accusation of substance abuse as an indication to disregard the claims of the accused. The physician is left without rights, depersonalized, and dehumanized. The imposition of confinement, stigmatization, lack of oversight of the organizations, peer-review protected confidentiality, and lack of procedural protection is a one-way train to hopelessness and despair.
By establishing a system that of coercion, control, secrecy, and misinformation, the FSPHP is claiming an “80% success rate” 15and deeming the “PHP-blueprint” as “the new paradigm in addiction medicine treatment.
The ASAM/FSPHP had a major influence on the DSM-V where drug abuse and dependence are no longer separate entities. They are also working behind the scenes to get legislation to randomly drug test all physicians.
They are now after the “disruptive physician” and the evidentiary criteria are fairly low and red flags include “deviating from workplace norm in dress or conduct” and being tardy for meetings.
They have identified “the aging physician” as a potential problem because “as the population of physicians ages,””cognitive functioning” becomes “a more common threat to the quality of medical care.”
The majority of physicians are unaware that the Federation of State Medical Boards House of Delegates adopted an updated Policy on Physician Impairment in 2011 that uses addiction as an example of a “potentially impairing illness.” According to the Federation of State Physician Health Programs …”physician illness and impairment exist on a continuum with illness typically predating impairment, often by many years. This is a critically important distinction. Illness is the existence of a disease. Impairment is a functional classification and implies the inability of the person affected by disease to perform specific activities.”
“Process addiction” was added as a potentially impairing illness including compulsive gambling, compulsive spending, compulsive video gaming, and “workaholism.” According to the FSPHP “the presence of a process addiction can be problematic or even impairing in itself, and it can contribute to relapse of a physician in recovery. As such, process addictions should be identified and treated.” They define three levels of relapse including the novel “relapse without use.”
Bullying, Helplessness, Hopelessness and Despair
Perceived helplessness is significantly associated with suicide.16 So too is hopelessness, and the feeling that no matter what you do there is simply no way out17,18 Bullying is known to be a predominant trigger for adolescent suicide19-21 One study found that adolescents in custody who were bullied were 9.22 times more likely to attempt suicide than those were not bullied.22
Heightened perceptions of defeat and entrapment are known to be powerful contributors to suicide.23,24 The “Cry of Pain” model 25,26 specifies that people are particularly prone to suicide when life experiences are interpreted as signaling defeat which is defined as a sense of “failed struggle” or loss of social position and resources.. The person is unable to identify an escape from or resolution to a defeating situation, a sense of entrapment proliferates with the perception of no way out, and this provides the central impetus for ending ones life.
There is also evidence that rescue factors such as social supports may play a role in preventing suicide. These rescue factors act buffers to protect against suicide in the face of varying degrees of life stress.27,28 The study of female physicians revealed meetings to discuss stressful work experiences as a potential protective factor, 29 and support at work when difficulties arose appeared to be a protective factor for the male physicians.30 Research involving Finnish physicians found that control over one’s work and organizational justice were the most important determinants of work-related wellbeing.31,32 Organizational justice is related to fairness and refers to an individuals perception of an organizations behaviors, decisions, and actions and how these influence one’s own attitudes and behaviors and has been identified as a psychosocial predictor of health and wellbeing33 34 Low organizational justice has been identified as a notable risk factor for psychological distress and depression.35,36
A recent report indicates that job stress, coupled with inadequate treatment for mental illness may play a role in physician suicide..
Using data from the National Violent Death Reporting System the investigators compared 203 physicians who had committed suicide to more than 31,000 non-physicians and found that having a known mental health disorder or a job problem that contributed to the suicide significantly predicted being a physician.1
Physicians were 3.12 times more likely to have a job problem as a contributing factor. In addition, toxicology testing showed low rates of medication treatment. The authors concluded that inadequate treatment and increased problems related to job stress are potentially modifiable risk factors to reduce suicidal death among physicians.
They also warned that the database used likely underestimated physician suicides because of “underreporting and even deliberate miscoding because of the stigma attached.”
I can think of nothing more institutionally unjust than an unregulated zero-tolerance monitoring program with no oversight using unregulated drug and alcohol testing of unknown validity.
We have heard of numerous suicides due to these institutionally unjust programs. Three doctors died by suicide in Oklahoma in a one month period alone (August 2014). All three were being monitored by the Oklahoma PHP. I went to an all boys high-school of less than 350 students yet a classmate a couple years ahead of me died by suicide a few months ago. He was being monitored by the Washington PHP. His crime? A DUI in 2009–a one-off situational mistake that in all likelihood would never have recurred. But as is often the case with those ensnared by state PHPs he was forced to have a “re-assessment” as his five-year monitoring contract was coming to an end. These re-assessments are often precipitated by a positive Laboratory Developed Test (LDT) and state medical boards mandate these assessments can only be done at an out-of-state “PHP-approved” facility. Told he could no longer operate and was unsafe to practice medicine by the PHP and assessment center he then hanged himself. And at the conclusion of Dr. Pamela Wible’s haunting video below are listed just the known suicides of doctors; many were being monitored by their state PHPs–including the first name on the list– Dr. Gregory Miday.
None of these deaths were investigated. None were covered in the mainstream media. These are red flags that need to be acknowledged and addressed! This anecdotal evidence suggests the oft-used estimate of 400 suicides per year (an entire medical school class) is a vast underestimation of reality—extrapolating just the five deaths above to the entire population of US doctors suggests we are losing at least an entire medical school per year.
As physicians we need to demand transparency, oversight, regulation and auditing by outside groups. This is a public health emergency.
To wit:
They first came after the substance abusers and I did not speak out because I was not a substance abuser.
They then came for those with psychiatric diagnoses and I did not speak out because I was not diagnosed with a psychiatric disorder.
They then came after the “disruptive physician” and I did not speak out because I was not disruptive.
They then came after the aging physician and I did not speak out because I was young.
They then came after me and there was no one else to speak out for me.
- Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Archives of internal medicine. Jul 13 1998;158(13):1422-1426.
- Frank E, Dingle AD. Self-reported depression and suicide attempts among U.S. women physicians. The American journal of psychiatry. Dec 1999;156(12):1887-1894.
- Brewster JM. Prevalence of alcohol and other drug problems among physicians. JAMA : the journal of the American Medical Association. Apr 11 1986;255(14):1913-1920.
- Anthony J, Eaton W, Mandell W, al. e. Psychoactive Drug Dependence and abuse: More Common in Some Occupations than in Others? Journal of Employee Assistance Res. 1992;1:148-186.
- Stinson F, DeBakely S, Steffens R. Prevalence of DSM-III-R Alcohol abuse and/or dependence among selected occupations. Alchohol Health Research World. 1992;16:165-172.
- Hughes PH, Brandenburg N, Baldwin DC, Jr., et al. Prevalence of substance use among US physicians. JAMA : the journal of the American Medical Association. May 6 1992;267(17):2333-2339.
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. Jun 2005;62(6):593-602.
- Boyd JW, Knight JR. Ethical and managerial considerations regarding state physician health programs. Journal of addiction medicine. Dec 2012;6(4):243-246.
- DuPont RL, McLellan AT, White WL, Merlo LJ, Gold MS. Setting the standard for recovery: Physicians’ Health Programs. Journal of Medical Regulation. Mar 2010;95(4):10-25.
- Skipper GE, Weinmann W, Thierauf A, et al. Ethyl glucuronide: a biomarker to identify alcohol use by health professionals recovering from substance use disorders. Alcohol and alcoholism. Sep-Oct 2004;39(5):445-449.
- Skipper GE, Thon N, Dupont RL, Baxter L, Wurst FM. Phosphatidylethanol: the potential role in further evaluating low positive urinary ethyl glucuronide and ethyl sulfate results. Alcoholism, clinical and experimental research. Sep 2013;37(9):1582-1586.
- Skipper GE, Thon N, DuPont RL, Campbell MD, Weinmann W, Wurst FM. Cellular photo digital breathalyzer for monitoring alcohol use: a pilot study. European addiction research. 2014;20(3):137-142.
- Sharfstein J. FDA Regulation of Laboratory-Developed Diagnostic Tests: Protect the Public, Advance the Science. JAMA : the journal of the American Medical Association. Jan 5 2015.
- Pham JC, Pronovost PJ, Skipper GE. Identification of physician impairment. JAMA : the journal of the American Medical Association. May 22 2013;309(20):2101-2102.
- McLellan AT, Skipper GS, Campbell M, DuPont RL. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. Bmj. 2008;337:a2038.
- Rivers I, Noret N. Potential suicide ideation and its association with observing bullying at school. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. Jul 2013;53(1 Suppl):S32-36.
- Lester D, Walker RL. Hopelessness, helplessness, and haplessness as predictors of suicidal ideation. Omega. 2007;55(4):321-324.
- Beck AT. Hopelessness as a predictor of eventual suicide. Annals of the New York Academy of Sciences. 1986;487:90-96.
- Hinduja S, Patchin JW. Bullying, cyberbullying, and suicide. Archives of suicide research : official journal of the International Academy for Suicide Research. 2010;14(3):206-221.
- Hertz MF, Donato I, Wright J. Bullying and suicide: a public health approach. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. Jul 2013;53(1 Suppl):S1-3.
- Kim YS, Leventhal B. Bullying and suicide. A review. International journal of adolescent medicine and health. Apr-Jun 2008;20(2):133-154.
- Kiriakidis SP. Bullying and suicide attempts among adolescents kept in custody. Crisis. 2008;29(4):216-218.
- Taylor PJ, Gooding P, Wood AM, Tarrier N. The role of defeat and entrapment in depression, anxiety, and suicide. Psychological bulletin. May 2011;137(3):391-420.
- Lester D. Defeat and entrapment as predictors of depression and suicidal ideation versus hopelessness and helplessness. Psychological reports. Oct 2012;111(2):498-501.
- Williams JMG. Cry of Pain. Harmondsworth: Penguin; 1997.
- Williams JMG, Crane C, Barnhofer T, Duggan DS. Psychology and suicidal behavior: elaborating the entrapment model. In: Hawton K, ed. Prevention and treatment of suicidal behavior: from science to practice. Oxford: Oxford University Press; 2005:71-89.
- Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: Risks and protectors. Pediatrics. 2001;107(485).
- Clum GA, Febbraro GAR. Stress, social support and problem-solving appraisal/skill: Prediction of suicide severity within a college sample. Journal of Psychopathology and Behavioral Assessment. 1994;16:37-46.
- Fridner A, Belkic K, Marini M, Minucci D, Pavan L, Schenck-Gustafsson K. Survey on recent suicidal ideation among female university hospital physicians in Sweden and Italy (the HOUPE study): cross-sectional associations with work stressors. Gender medicine. Apr 2009;6(1):314-328.
- Fridner A, Belkic K, Minucci D, et al. Work environment and recent suicidal thoughts among male university hospital physicians in Sweden and Italy: the health and organization among university hospital physicians in Europe (HOUPE) study. Gender medicine. Aug 2011;8(4):269-279.
- Lindfors PM, Meretoja OA, Toyry SM, Luukkonen RA, Elovainio MJ, Leino TJ. Job satisfaction, work ability and life satisfaction among Finnish anaesthesiologists. Acta anaesthesiologica Scandinavica. Aug 2007;51(7):815-822.
- Heponiemi T, Kuusio H, Sinervo T, Elovainio M. Job attitudes and well-being among public vs. private physicians: organizational justice and job control as mediators. European journal of public health. Aug 2011;21(4):520-525.
- Elovainio M, Kivimaki M, Vahtera J. Organizational justice: evidence of a new psychosocial predictor of health. Am J Public Health. Jan 2002;92(1):105-108.
- Lawson KJ, Noblet AJ, Rodwell JJ. Promoting employee wellbeing: the relevance of work characteristics and organizational justice. Health promotion international. Sep 2009;24(3):223-233.
- Hayashi T, Odagiri Y, Ohya Y, Tanaka K, Shimomitsu T. Organizational justice, willingness to work, and psychological distress: results from a private Japanese company. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. Feb 2011;53(2):174-181.
- Lang J, Bliese PD, Lang JW, Adler AB. Work gets unfair for the depressed: cross-lagged relations between organizational justice perceptions and depressive symptoms. The Journal of applied psychology. May 2011;96(3):602-618.





 The Plan to… Require Doctors to Drug-Test all Patients
The Plan to… Require Doctors to Drug-Test all Patients





 Wanted!–a Few Statisticians, Biostatisticians and Epidemiologists who want to make a difference in Medicine, Society and our Future
Wanted!–a Few Statisticians, Biostatisticians and Epidemiologists who want to make a difference in Medicine, Society and our Future
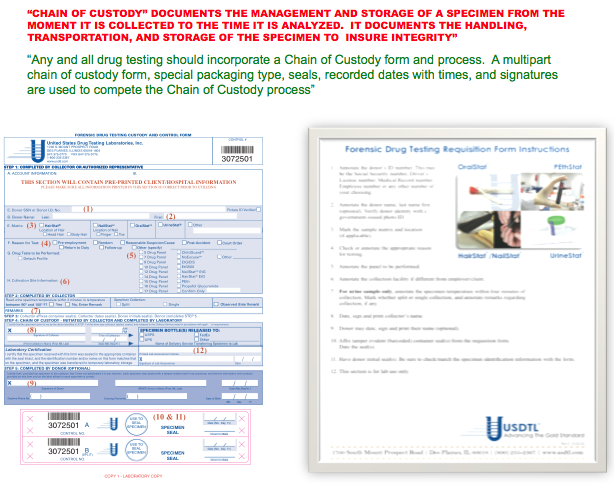
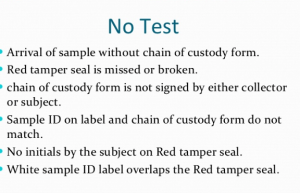
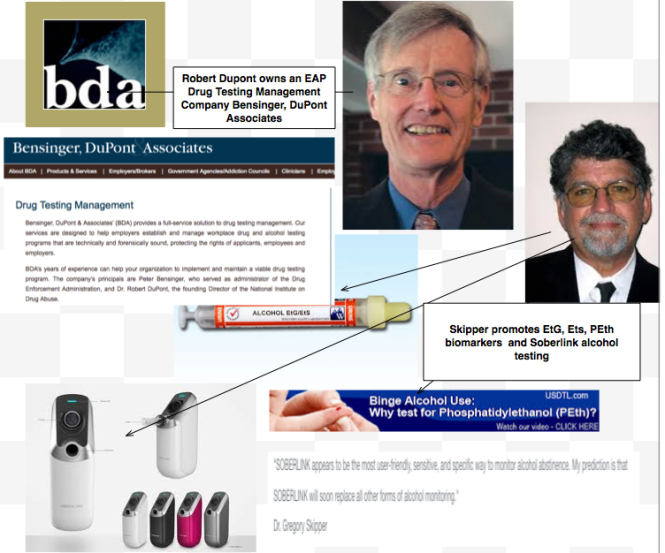

 Using an arbitrary cutoff level of 100 ug/L the EtG was marketed as a valid and reliable test and blindly tested on those being monitored by programs not beholden to the strict protocol and procedure dictated by the Mandatory Guidelines for Federal Workplace Drug Testing that most Employee Assistance Programs (EAPs) adopted. In other words, the test was used on those who possessed little power or had their power removed.
Using an arbitrary cutoff level of 100 ug/L the EtG was marketed as a valid and reliable test and blindly tested on those being monitored by programs not beholden to the strict protocol and procedure dictated by the Mandatory Guidelines for Federal Workplace Drug Testing that most Employee Assistance Programs (EAPs) adopted. In other words, the test was used on those who possessed little power or had their power removed.