 “With one arm around the shoulder of religion and the other around the shoulder of medicine, we might change the world.”—Twelve Steps and Twelve Traditions, AA World Services, Inc (1953).
“With one arm around the shoulder of religion and the other around the shoulder of medicine, we might change the world.”—Twelve Steps and Twelve Traditions, AA World Services, Inc (1953).
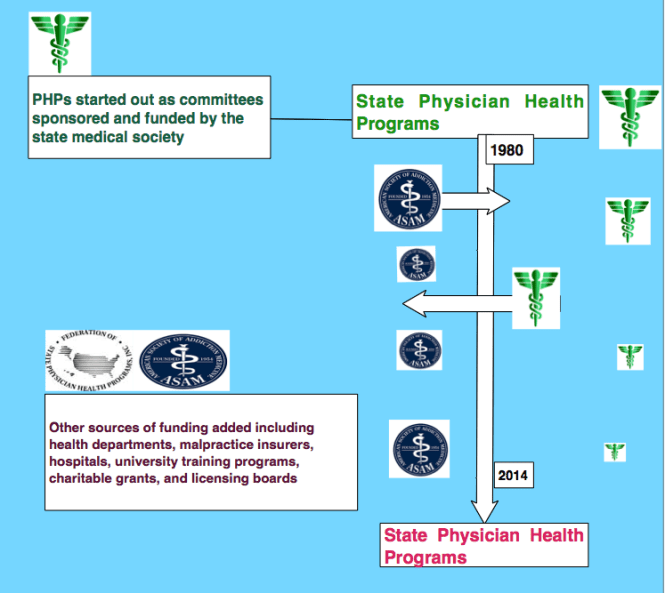
In order to comprehend the current plight of the medical profession and the dark clouds that lie ahead it is necessary to understand the history of the “impaired physician movement” and the American Society of Addiction Medicine (ASAM).
In 1985 the British sociologist G. V. Stimson wrote:
“The impaired physician movement is characterized by a number of evangelical recovered alcoholic and addict physicians, whose recovery has been accompanied by an involvement in medical society and treatment programs. Their ability to make authoritative pronouncements on physician impairment is based on their own claim to insider’s knowledge.”1
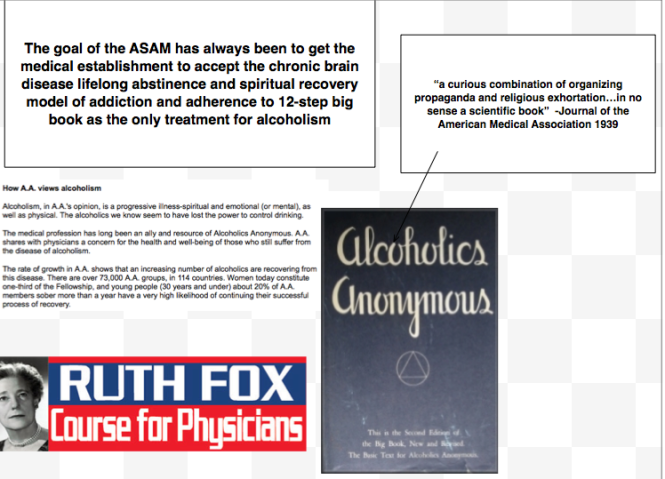
The impaired physician movement emphasizes disease and therapy rather than discipline and punishment and believes that addiction is a chronic relapsing brain disease requiring lifelong abstinence and 12-step spiritual recovery. The drug or alcohol abuser or addict is a person lacking adequate internal controls over his or her behavior; for his own protection as well as the protection of society external restraints are required including involuntary treatment.
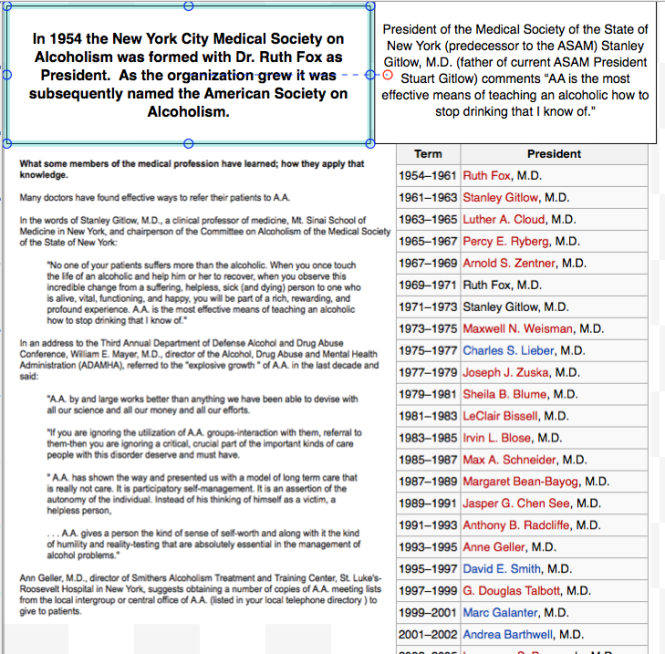
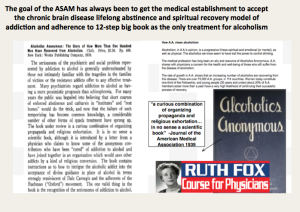
The American Society of Addiction Medicine (ASAM) can trace its roots to the 1954 founding of the New York City Medical Society on Alcoholism (NYCMSA) by Ruth Fox, M.D whose husband died from alcoholism.
Finding that alcoholics in her psychoanalytic practice did not recover when she used conventional analytic approaches, she taught her patients about alcoholism as a disease and introduced “them to AA meetings held in her living room.”2
A number of physicians in the New York Medical Society were themselves recovering alcoholics who turned to Alcoholics Anonymous for care.3
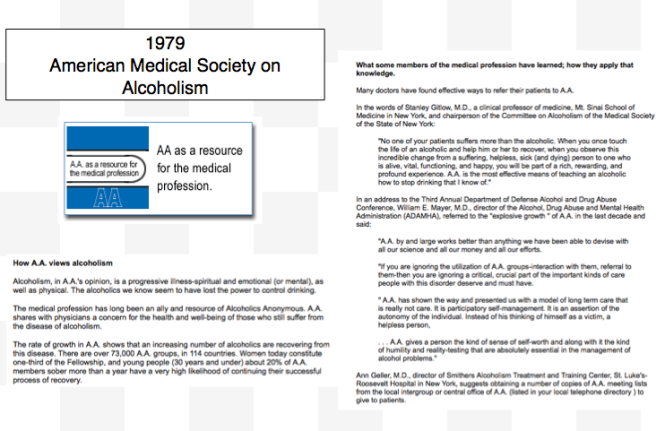
The society, numbering about 100 members, established itself as a national organization in 1967, the American Medical Society on Alcoholism (AMSA).3
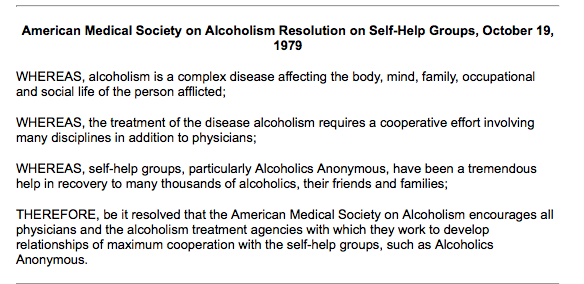
The group promoted the concept of alcoholism as a chronic relapsing disease requiring lifelong spiritual recovery through the 12-steps of AA.
By 1970 membership was nearly 500.2
In 1973 AMSA became a component of the National Council on Alcoholism (NCA), now the National Council on Alcoholism and Drug Dependence (NCADD) in a medical advisory capacity until 1983.
“Abstinence from alcohol is necessary for recovery from the disease of alcoholism” became the first AMSA Position Statement in 1974.2
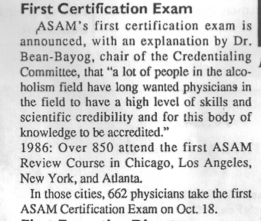
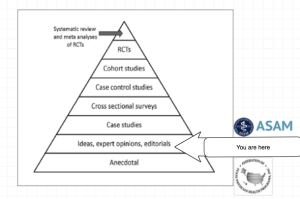
In 1985 ASAM’s first certification exam was announced. According to Dr. Bean-Bayog, chair of the Credentialing Committee:
“A lot of people in the alcoholism field have long wanted physicians in the field to have a high level of skills and scientific credibility and for this body of knowledge to be accredited.”2And in 1986 662 physicians took the first ASAM Certification Exam.
By 1988 membership was over 2,800 with 1,275 of these physicians “certified” as:
“having demonstrated knowledge and expertise in alcoholism and other drug dependencies commensurate with the standards set forth by the society.”4 “While certification does not certify clinical skill or competence,” the Board explained, “it does identify physicians who have demonstrated knowledge in diagnosis and treatment of alcoholism and other drug dependencies.”5Achieving “recognized board status for chemical dependence” and fellowships in “chemical dependency” are among the five-year objectives identified by the group. These are to come to fruition by “careful discussion, deliberation, and consultation” to “determine its form and structure and how best to bring it about.”5
The formation of ASAM State Chapters begins with California, Florida, Georgia, and Maryland submitting requests.6
In 1988 the AMA House of Delegates votes to admit ASAM to the House. According to ASAM News this “legitimizes the society within the halls of organized medicine.”2
In 1989 the organization changes its name to the American Society of Addiction Medicine (ASAM).2
Since 1990, physicians have been able to list addiction medicine as a self-designated area of practice using the specialty code “ADM.”
By 1993 ASAM has a membership of 3,500 with a total of 2,619 certifications in Addiction Medicine.
The Membership Campaign Task Force sets a goal to double its membership of 3,500 to 7,000 by the year 2000 to assure “the future of treatment for patients with chemicals. It represents a blueprint for establishing addiction medicine as a viable entity.”7
Ninety physicians become Fellows of the American Society of Addiction Medicine (FASAM) in 1996 “to recognize substantial and lasting contributions to the Society and the field of addiction medicine.”8
Among the honorees are Robert DuPont, G. Douglas Talbott, Paul Earley, and Mel Pohl. In addition to at least five consecutive years of membership and certification by the Society, Fellows must have “taken a leadership role in ASAM through committee service, or have been an officer of a state chapter, and they must have made and continue to make significant contributions to the addictions field.”8
The American Board of Addiction Medicine (ABAM) is formed in 2007 as a non-profit 501(C)(6) organization “following conferences of committees appointed by the American Society of Addiction Medicine” to “examine and certify Diplomats.”9
In 2009 National Institute on Drug Abuse (NIDA) Director Nora Volkow, M.D., gives the keynote address at the first ABAM  board certification diploma ceremony.10
board certification diploma ceremony.10
According to an article in Addiction Professional “Board certification is the highest level of practice recognition given to physicians.”
“A Physician membership society such as ASAM, however, cannot confer ‘Board Certification,’ ” but a“ “Medical Board such as ABAM has a separate and distinct purpose and mission: to promote and improve the quality of medical care through establishing and maintaining standards and procedures for credentialing and re-credentialing medical specialties.”
The majority of ASAM physicians meet these requirements by “working in a chemical dependency treatment facility, taking continuing medical education courses in addiction, or participating in research.”11
“In the United States accredited residency programs in addiction exist only for psychiatrists specializing in addiction psychiatry; nonpsychiatrists seeking training in addiction medicine can train in nonaccredited ‘fellowships,’ or can receive training in some ADP programs, only to not be granted a certificate of completion of accredited training.”11
Specialty recognition by the American Board of Medical Specialties, fifty Addiction Medicine Fellowship training programs and a National Center for Physician Training in Addiction Medicine are listed as future initiatives of the ABAM Foundation in 2014.
The American Society of Addiction Medicine’s mission is to “establish addiction medicine as a specialty recognized by professional organizations, governments, physicians, purchasers, and consumers of health care products, and the general public’12
In this they have succeeded.
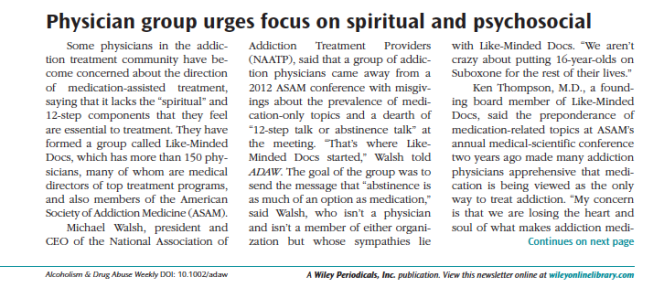
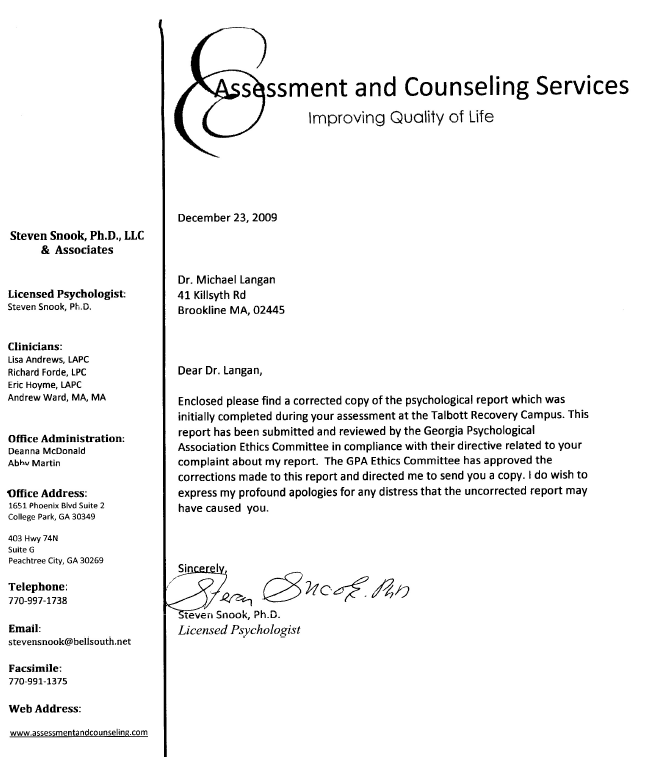
And in the year 2014 G.V. Stimson’s characterization of the “impaired physician movement” remains as accurate and apt as it was in 1985. But the “number of evangelical recovered alcoholic and addict physicians” has increased dramatically (outnumbering Addiction Psychiatry by 4:1) and their involvement in “ medical society and treatment programs” has been realized and enforced through the state Physician Health Programs and their “PHP-approved’ assessment and treatment centers.
Their “ability to make authoritative pronouncements on physician impairment…based on their own claim to insider’s knowledge” has become public policy and sanctified by Regulatory Medicine -essentially the Word of the Lord.
And the 1953 Alcoholics Anonymous prophecy that “With one arm around the shoulder of religion and the other around the shoulder of medicine, we might change the world” is also coming to pass.
But the world is not changing for the better as that arm around the shoulder of religion has its fingers deep in the pockets of the multi-billion dollar drug and alcohol testing and assessment and treatment industries. And the arm around the shoulder of medicine has its fingers clamped tightly around its throat; a stranglehold in full throttle suffocating the Profession of Medicine with no meaningful opposition I can see.
- Stimson GV. Recent developments in professional control: the impaired physician movement in the USA. Sociology of health & illness. Jul 1985;7(2):141-166.
- Four Decades of ASAM. ASAM News. March-April 1994, 1994.
- Freed CR. Addiction medicine and addiction psychiatry in America: Commonalities in the medical treatment of addiction. Contemporary Drug Problems. 2010;37(1):139-163.
- . American Medical Society on Alcoholism & Other Drug Dependencies Newsletter. Vol III. New York, NY: AMSAODD; 1988:12.
- Ursery S. $1.3M verdict coaxes a deal for doctor’s coerced rehab. Fulton County Daily Report. May 12, 1999b 1999.
- . AMSAODD News. Vol III. New York, NY: American Medical Society on Alcoholism & Other Drug Dependencies; 1988.
- Membership Campaign Update. ASAM News. Vol VIII: American Society of Addiction Medicine; 1993:11.
- . ASAM News. Vol 12. Chevy Chase, MD: American Society of Addiction Medicine; 1997:20.
- http://www.abam.net/about/history/.
- Kunz KB, Gentiello LM. Landmark Recognition for Addiction Medicine: Physician certification by the American Board of Addiction Medicine will Benefit all Addiction Professionals. Addiction Professional. 2009. http://www.addictionpro.com/article/landmark-recognition-addiction-medicine.
- Tontchev GV, Housel TR, Callahan JF, Kunz KB, Miller MM, Blondell RD. Specialized training on addictions for physicians in the United States. Substance abuse : official publication of the Association for Medical Education and Research in Substance Abuse. Apr 2011;32(2):84-92.
- http://www.asam.org/about-us/mission-and-goals.