There’s something in his soul
O’er which his melancholy sits on brood,
And I do doubt the hatch and the disclose
Will be some danger—which for to prevent,
I have in quick determination……..
It shall be so. Madness in great ones must not unwatched go.
—Hamlet Act III, Scene 1
There’s something in his soul
O’er which his melancholy sits on brood,
And I do doubt the hatch and the disclose
Will be some danger—which for to prevent,
I have in quick determination……..
It shall be so. Madness in great ones must not unwatched go.
—Hamlet Act III, Scene 1
According to
Radar Online Robin Williams is looking “grim and focused.” Grim? Yes. Focused? No. His visage is one of entrapment, despair, and dread.
In F. Scott Fitzgerald’s The Great Gatsby, Nick Carraway observes that “the loneliest moment in someone’s life is when they are watching their whole world fall apart, and all they can do is stare blankly” This is not focus but melancholia–hopelessness, helplessness, and defeat.
In 1896
Émile Durkheim described “melancholy suicide” as being “connected with a general state of extreme depression and exaggerated sadness, causing the patient no longer to realize sanely the bonds which connect him with people and things about him. Pleasures no longer attract.” Williams’ face is weighted with melancholy. Not focus.
Heightened perceptions of defeat and entrapment are known to be powerful predictors of suicide. According to the “Cry of Pain” model people are particularly prone to suicide when life experiences are interpreted as signaling defeat, defined as a sense of a “failed struggle.” Unable to find some sort of resolution to a defeating situation, a sense of entrapment proliferates and the perception of no way out provides the central impetus for ending one’s life.
As in all suicidal tragedies, the role of addiction and mental illness has been posited as the cause. Although depression and substance abuse are the two biggest risk factors for suicide, neither explains completion of the act–the descent from ideation and planning to finality and oblivion. Saying suicide is caused by depression and drugs is like claiming marijuana is a “gateway drug” to heroin. It may be a a common related pre-conditional occurrence but it is not the cause. It is a non sequitur. And just as most marijuana users never develop an inclination to stick an opiate filled needle into their veins, the majority of depressed individuals and substance abusers do not kill themselves. One does not lead to the other.
And as we have seen in the reports of bullied teenagers who have died by suicide, it is all too often the bullies themselves who are quickest to pronounce this conclusion. Attributing suicide to mental illness and substance abuse deflects culpability. It negates the need for further inquiry. It creates an absence of the need to change. The rationalization diffuses both individual and collective blame. It scatters responsibility and guilt. It is both an individual and community defense mechanism. Incessantly and chronically shaming, humiliating, and degrading another person because of race, body type, sexual preference or whatever perceived eccentricity or non-conformity threatened the community herd was irrelevant. It played no role. It was drink, drugs, or depression–the unspoken understanding is they would have done it anyway. And no one stops to ponder that said depression or desire to alter ones mental state just might in actual fact be a symptom of the humiliation and shame they themselves created. And it works. The bullies are never held accountable. But it is nevertheless they who figuratively loaded the gun, placed it in the victims mouth, and pulled the trigger.
The link between bullying and suicide is well known, especially when combined with entrapment and the feeling there is no way out. “They would have done it anyway.” No, they would not have and a modicum of perceived support, concern, kindness and understanding from others may have prevented it.
Dr. Drew Pinsky seemed omnipresent in discussing Williams suicide; delivering authoritative pronouncements with seeming omniscience and certainty. “The death of Robin Williams has led me to this plea — let’s loudly and seriously address something that’s still hidden, stigmatized and even ignored in this country: Mental illness,” Pinsky writes on his blog. I don’t see the logic here. How is exposing mental illness a product of Williams suicide. He was open, unashamed, and forthright about his prior addictions and depression. He was not hiding it. Neither is the 21st century for that matter.
The more important issue that I see needs pleading, is that mental illness be properly, accurately, and thoughtfully diagnosed and treated.
Depression, as with any mental illness, needs to be diagnosed, monitored, and treated by educated, trained, and experienced experts in depression. Not self-proclaimed experts. Pinsky’s specialty is “addiction medicine” and he is “board certified” by the American Board of Addiction Medicine (ABAM).
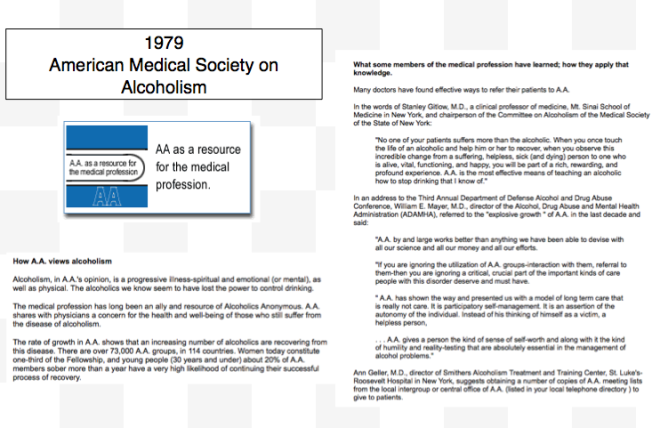
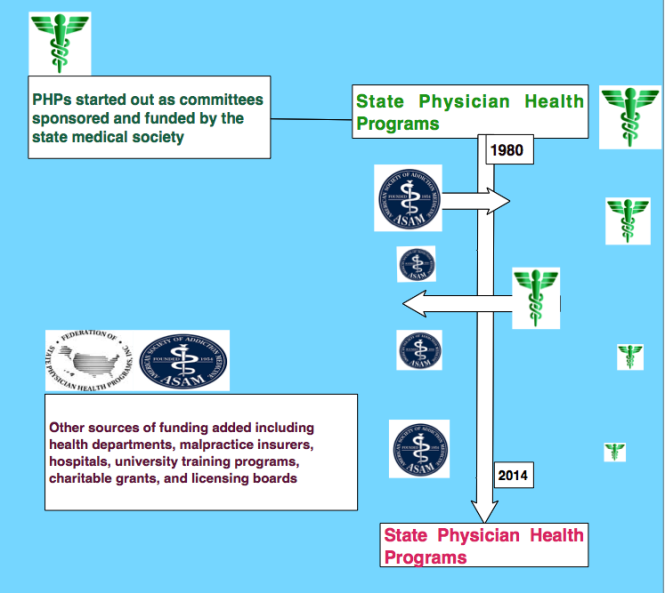
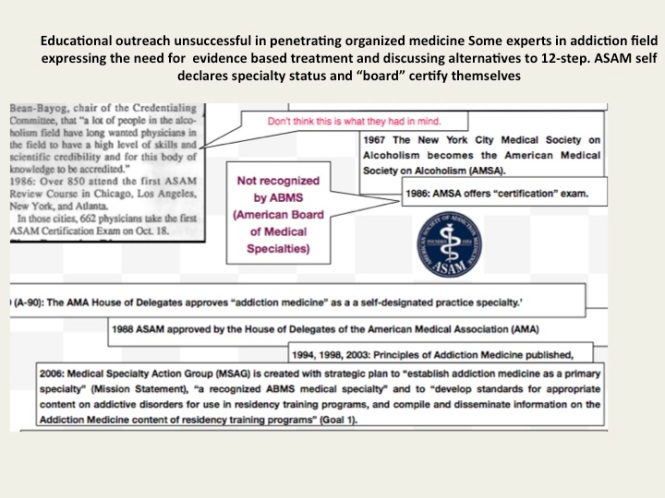
The American Society of Addiction Medicine can trace its roots to the 1954 founding of the New York City Medical Society on Alcoholism (NYCMSA) by Ruth Fox, M.D., whose husband died from alcoholism. This group promoted the concept of alcoholism as a chronic relapsing brain disease requiring lifelong spiritual recovery through the 12-steps of AA. And the primary goal of the ASAM is and always has been the acceptance of 12-step doctrine, lifelong abstinence, and spiritual recovery as the one and only treatment for addiction. It always will be.
This philosophy and guiding doctrine stems from the “impaired physician movement”, a group that, according to British sociologist G.V. Stimson: ” is characterized by a number of evangelical recovered alcoholic and addict physicians, whose recovery has been accompanied by an involvement in medical society and treatment programs. Their ability to make authoritative pronouncements on physician impairment is based on their own claim to insider’s knowledge.” This group grew in numbers, organized, and eventually became the ASAM.
The American Board of Medical Specialties (ABMS) recognizes 24 medical specialties and subspecialties. Addiction Medicine is not one of them. The only ABMS recognized subspecialty is Addiction Psychiatry and it requires a four-year psychiatric-residency program followed by a 1-year Fellowship focusing on addiction in an accredited training program.
In contrast, ABAM certification requires only a medical degree, a valid license to practice medicine, and completion of residency training in ANY specialty.
Hazelden, the facility where Williams was admitted in July is an ASAM facility. And the Medical Director, Marvin Seppala is a Like-Minded Doc. Unlike most ASAM physicians, however, Seppala is a psychiatrist. But he is a psychiatrist brought up in the folds of ASAM ideology. He was, in fact, the first adolescent graduate of Hazelden in the 1970s when he completed the program at the age of 19.
Pinsky, predictably goes on to state that “Williams had a brain disease, ” He posits it against demons or devils as if it is either/or. This concrete splitting of complex subjects into two separate entities to claim only one correct is just one of many simplistic and misleading “false dichotomies” used by the ASAM. Of course addiction is a brain disease. But in reality the definition is unhelpful unless we are living in the Victorian era. It’s like saying Gonorrhea is a genital disease not venereal (from Latin venereus “of sexual love”). In reality it involves a number of factors including both psychosocial and medical. Cornering a definition does nothing to advance knowledge and care.
Addiction is multifactorial and diverse. Simplifying it into binary options does little to advance understanding. And it too involves a variety of issues including the situational, the psychosocial, the genetic and the biochemical. Like every other medical issue there are a number of factors to be taken into consideration. And imposing the 12-steps to salvation on all-comers is not only illogical, but anti-science, and downright improper. It can also be deadly. Especially when the the person it is imposed on is not a full-blown addict but a substance abuser. an experimenter, a dabbler, or someone who has simply had a “lapse.”
The ASAM emphasizes that addiction is a “brain disease” and not a “moral failing” in a mutually exclusive construct that allows either one or the other but not both. It is presented as a dichotomy in which the promotion of one both precludes and dismisses the other. It is either black or white. Period.
But substance use, abuse, and addiction comes in every color, saturation, hue and shade. Psychosocial, behavioral, and social factors play a role in the actions and deeds of everyone including those addicted to alcohol and drugs. The disease concept neglects this multifactorial confluence of factors that ultimately produce a given behavior by viewing all behavior a product of the “disease.” Any and all behavior is simply a product of a “brain disease” in the addicted individual who cannot be trusted to make decisions on his own but has to be told what to do as part of the treatment. A danger to himself and others the addict cannot be trusted to make his own decisions, so we must make them for him.
The chronic brain disease model is an oversimplification of the complex and a false dichotomy–so too is bifurcating “recovery” and “relapse,” treatment” and “discipline,” and “confession”and “denial.” Anything less than total abstinence constitutes an illness.
One true dichotomy that exists among the proponents of the chronic brain disease model of addiction with lifelong abstinence and spiritual recovery is a person is either “with them” or “against them.”
Dr. Drew Pinsky notes “there were a number of factors” that contributed to William’s condition. He states “alcoholism is certainly one. He may have had a genetic potential for depression. Addiction and depression can be an easily fatal combination.” Non-sequitur.
Depression needs to be treated by thoughtful, educated, competent and trained experts in depression not self-declared experts. ASAM doctors are not “real” experts. They are pretend experts trumpeting one frozen paradigm while dismissing or ignoring others. It is expert opinion where the goal is not new knowledge and and new discovery. The die is cast. And most of the “research” put out by this group consists of methodologically unsound studies published in their journals in which an attempt is made to make the data fit an already determined hypothesis.
Point being that depression needs to be evaluated and treated by trained professionals who understand depression. Psychiatrists, psychopharmacologists, neuropsychologists, and psychologists schooled in a broad spectrum of treatment modalities. Numerous depression treatments are available. If one treatment fails or is ineffective then others must be tried. Most depression is treatable, especially subacute or acute depression. SSRIs, SNRIs SNDRIs, tricyclics, MAOs, and atypical antidepressants are available. Different types of psychotherapy are available–cognitive behavioral therapy, interpersonal therapy, dialectic behavioral therapy, mindfulness therapy, and Jungian psychoanalysis can be beneficial for people suffering from depression. And ECT and TMS can also play a role in depression refractory to medications and psychotherapy.
Depression is extremely common in Parkinson’s disease but due to the dopamine loss it requires special consideration of what drugs to use and not use. SSRI’s can sometimes worsen the condition. Consultation with a knowledgable and experienced neurologist is critical.
I do not know what assessments or treatments were being tried in Robin Williams. But the treatment modalities offered by ASAM physicians are usually few to one.
The majority of “addiction medicine” specialists are not psychiatrists. For all you know you may find yourself being treated by an addiction “specialist” who was a practicing proctologist just a few years prior; and perhaps not even a good one at that.
Moreover, many of the ASAM physicians are “anti-medication” and may take people off medications that have been helping them and that they need. And the devastating results are often seen after the patient has been discharged home.
Taken off drugs while in rehab and sent home without them, the beneficial effects may wear off gradually. And as they do mental conditions may deteriorate. Manic episodes, paranoid psychoses, extreme anxiety, and profound depression can all occur well after someone has been discharged home. So can suicide.
And when this happens the ASAM doctors blame it on their fatal “disease” when, just as is seen with the suicides of bullied teens, it was actually they who put the gun to their heads and pulled the trigger.
Depression needs to be treated by experts in depression. Putting someone in a one-size fits all shackled and frozen mold can be fatal. And calling them helpless addicts with a chronic disease who have no control due to character defects adds kindling to the fire. Depressed people need empowerment not powerlessness; self-esteem not shame. Shame is devastating. It goes right to the core of the person’s identity making them feel exposed, inferior, and degraded. Dehumanized, delegitimized, and vulnerable. The link between bullying and suicide is clear. And this is especially true when combined with entrapment. The feeling there is no way out.
When society gives power of diagnosis and treatment to individuals within a group schooled in just one uncompromising model of addiction with the majority attributing their very own sobriety to that model, they will exercise that power to diagnose and treat anyone and everyone according to that model. And it can be fatal.
Under a dictatorship everything else becomes subordinated to the guiding philosophy of the dictatorship. Corresponding doctrine replaces ethics as well as professional guidelines, standards of care, and evidence based medicine. Ideology usurps critical thinking. Having only a hammer, everyone is seen as a nail A symphony with just one note.
And faith in institutions demands mass adherence to faith in that authority. Direct challenge to the status quo undermines the publics blind faith. The biggest obstacle is th at this system allows them to throw the normal rules of conduct under the imperative of a higher goal assumed to trump all other consideration.
at this system allows them to throw the normal rules of conduct under the imperative of a higher goal assumed to trump all other consideration.
All of medicine needs to be predicated on competence, thoughtfulness, good-faith, civility, honesty, and integrity. This is universally applicable. All specialties of medicine are required by that specialty to practice evidence based medicine and avoid conflicts of interest except one–addiction medicine. Due to a confluence of factors they have been given a pass.
But the validity and reliability of opinions lie in their underlying methodology. Reliance on the personal authority of any expert or group of experts is a logical fallacy.
And in order to save American Medicine this problem needs to be clearly recognized. The ASAM has a monopoly on addiction medicine. Treatment of substance abuse in this country is, in fact, defined by the impaired physicians movement paradigm.
A paradigm that is in actuality rife with methodologically flawed studies, cherry picking, bias, and cognitive distortion. A paradigm that places expert opinion, ideology, and doctrine above critical thinking and evidence base. Coercion and control are placed above patient autonomy and individual choice because the patient has a “disease” and can’t think for himself. So we’ll think for him. The conflicts of interest are many and complex. They would be unimaginable in other fields of medicine.
But I agree with Pinsky on one point. His comment that addiction and depression can be a deadly combination is true. And this is especially so when treatment of the addiction is the primary focus and consists of imposed 12-step indoctrination and the depression remains untreated or ineffectively treated. That is a deadly combination indeed–and one that can easily lead a person down the road of hopelessness, helplessness, and despair. And it is time the medical field as a whole shined some light on this, and hold addiction medicine to the same standards of conduct and care as the rest of the profession.
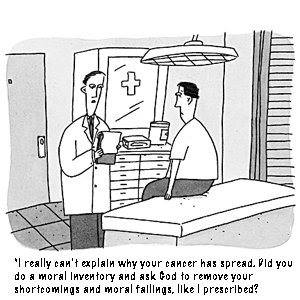
 Over the years, the American Society of Addiction Medicine has continued to promote the AA position that alcoholism (and by inference any other addiction) is an illness which only a “spiritual experience will conquer.” All addictions are believed by ASAM to be caused by a lifelong chronic relapsing brain disorder that can only be treated by complete abstinence from all mood-altering substances (with the apparent exceptions of tobacco and caffeine interestingly) and the vast majority of ASAM doctors believe that the only effective treatment for addiction must include surrendering one’s “will and life over to the care of God.”
Over the years, the American Society of Addiction Medicine has continued to promote the AA position that alcoholism (and by inference any other addiction) is an illness which only a “spiritual experience will conquer.” All addictions are believed by ASAM to be caused by a lifelong chronic relapsing brain disorder that can only be treated by complete abstinence from all mood-altering substances (with the apparent exceptions of tobacco and caffeine interestingly) and the vast majority of ASAM doctors believe that the only effective treatment for addiction must include surrendering one’s “will and life over to the care of God.”

















 There’s something in his soul
O’er which his melancholy sits on brood,
And I do doubt the hatch and the disclose
Will be some danger—which for to prevent,
I have in quick determination……..
It shall be so. Madness in great ones must not unwatched go.
—Hamlet Act III, Scene 1
There’s something in his soul
O’er which his melancholy sits on brood,
And I do doubt the hatch and the disclose
Will be some danger—which for to prevent,
I have in quick determination……..
It shall be so. Madness in great ones must not unwatched go.
—Hamlet Act III, Scene 1



 This dicto simpliciter argument can, in fact, be refuted simply by pointing it out! Sadly, no one ever did so the ASAM front-group hasbeen able to establish this caricature of the arrogant paternalistic know it all needing 3 months or more of treatment as standard of care for our profession. They did this by getting medical boards and the FSMB to accept fantasy as fact by relying on board members tendency to accept expert evidence at face value–which they always do and that is a personality characteristic that I would argue is not dicto simpliciter.
This dicto simpliciter argument can, in fact, be refuted simply by pointing it out! Sadly, no one ever did so the ASAM front-group hasbeen able to establish this caricature of the arrogant paternalistic know it all needing 3 months or more of treatment as standard of care for our profession. They did this by getting medical boards and the FSMB to accept fantasy as fact by relying on board members tendency to accept expert evidence at face value–which they always do and that is a personality characteristic that I would argue is not dicto simpliciter.