By the way if you have a problem with that, I mean, we could just step outside and we could figure it out.
drug testing
I support Bernie Sanders, and I’m not stupid or unrealistic

Today I read for maybe the 10,000th time an assertion that supporters of Bernie Sanders are unrealistic, that Bernie Sanders supporters will all be disappointed if they elect him because he won’t be able tobring the change he’s promising, that Bernie Sanders’ policies will be “just another example of Democrats making promises they can’t keep,” and so on and so forth. And I’d like to briefly dispel a misconception about people who support Bernie Sanders as the next president of the United States:
We’re not stupid.
View original post 587 more words
“For What it’s Worth”— The ASAM/ABAM Diploma Mill
“For What it’s Worth”— The ASAM/ABAM Diploma Mill
“In a time of universal deceit, telling the truth is a revolutionary act.”
— George Orwell
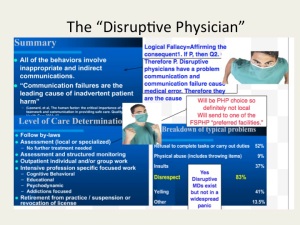
I can think of no other specialty or subspecialty in the profession of medicine where non-existent expertise can be incontestably announced and implemented. If I claimed to be an ace neurosurgeon or an expert otolaryngologist and started practicing my claimed skills in the hospital I would be called on it pretty quick by both colleagues and patients–deemed a delusional fraud and run out on a rail within a week. Both law enforcement, attorneys and psychiatry would be called in short order.
Yet doctors who have not met the usual and customary standards for professional and educational quality that have been identified for medical specialties and subspecialties are able to claim expertise in “addiction medicine” and everybody just lets them.
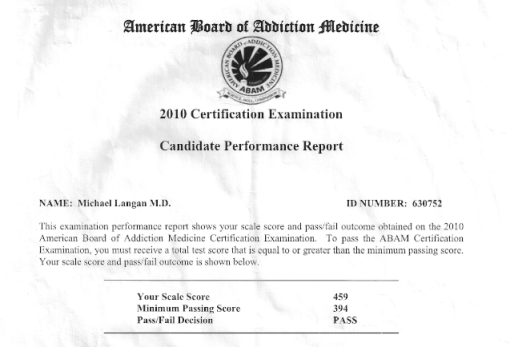
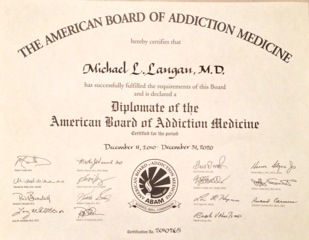
To make this point I sat for the 2010 American Board of Addiction Medicine Certification Examination. I did this to make a point–kind of like seeing how easy it is to buy a gun at a Walmart.
I simply went to the ABAM Website, completed the application and paid the fee.
The requirements to sit for the exam included so many “practice experience hours” over the past five years and 50 CME credits related to addiction.
With a year of psychopharmacology research, a half-day per week moonlighting at the MBTA medical clinic giving drug tests to bus drivers and another overnight moonlighting job giving medical clearance to patients at a local psychiatric hospital detox unit I satisfied the first requirement. For the latter I looked through the last five years of morning reports, noontime lectures and grand rounds I went to and added them up and, falling a little short supplemented the CME credits with some online modules.
And with that I was given a date at Pearson to take the test.
I have absolutely no training or education in the field of addiction medicine. I didn’t pick up a book or study anything. I did not prepare at all. I did not even get a good night’s sleep the night before and stayed up until 2:30 a.m. Nevertheless I went to the testing facility the next morning and finished the test within an hour and a half. My score is below. Aced it. Passing score was 394 and I got a 459.
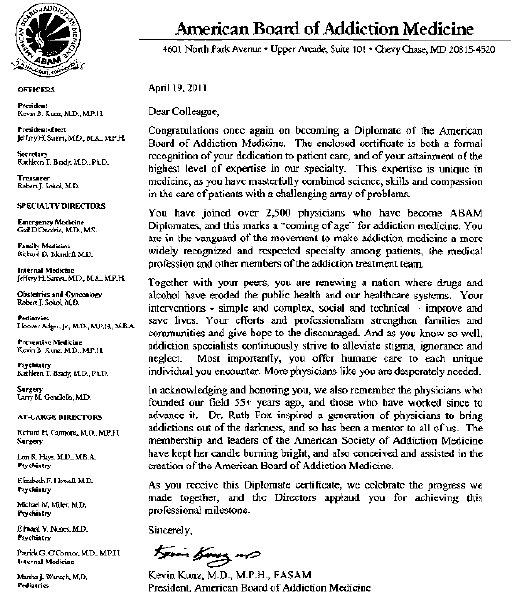
And the point I am trying to make is I am no expert in Addiction Medicine. Neither is 4000 of me. Yet the letter below says I am. Majority apparently rules.
Giving false expertise to the unqualified and granting them power over others is just as dangerous as the gun from Walmart. They can both kill.
An interest in something does not an expert make. If we allow this then the ASAM 12-step chronic brain disease model not only swallows addiction medicine but tarnishes all of medicine. An imposition by force and the deep pockets of the billion dollar drug and alcohol testing, assessment and treatment industry.
ASAM is not a true medical specialty. It is a special interest group. ABAM is not recognized by the American Board of Medical Specialties (ABMS).
The arguments seem to be:
1) Addiction is a prevalent “disease” that needs to be “treated;”
2) There are not enough Addiction Psychiatrists to diagnose and treat them.
3) Being an M.D. addict or alcoholic gives enough knowledge and apprenticeship skills to diagnose and treat others with the same affliction.
4) Let’s utilize them to fill the void.
This is logical fallacy and it is dangerous.
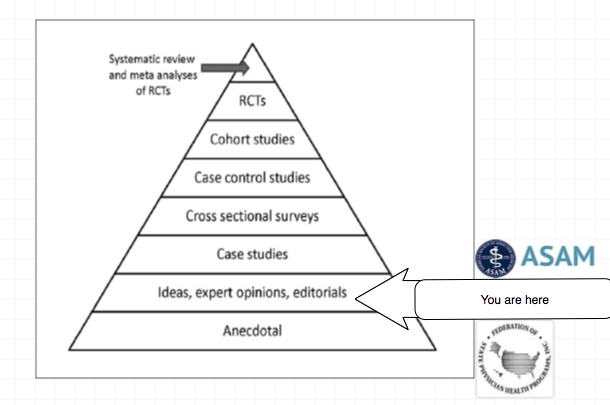
The validity and reliability of opinions lie in their underlying methodology and evidence base. Reliance on the personal authority of any expert or group of experts is the fallacy of appeal to authority.
An interest in something does not an expert make. I had an interest in science as a child but my certification as a member of Sir Isaac Newton’s Scientific Club did not make me a scientist.
I have asthma but that does not make me a Pulmonologist. That addiction “specialist” diagnosing and treating you may have 5 years prior been a proctologist; and maybe not even a very good one at that.
Somewhere there may be doctor with no post-graduate training in surgery wielding a scalpel and calling himself an expert surgeon, but it is difficult to imagine that he is a very good one.
I received my ABMS certification without meeting a single person. It was all done by mail. This fits the very definition of “Diploma Mill.” This is not to besmirch those with a sincere interest in helping others with addiction. Many if not most of those involved are sincere. But this is not expertise. This is not authority. And, as we have seen, this low bar opens the door for some very bad apples.
“This election is not about issues,” Rick Davis, John McCain’s campaign manager said this week. “This election is about a composite view of what people take away from these candidates.” That’s a scary thought. For the takeaway is so often base, a reflection more of people’s fears and insecurities than of our hopes and dreams.
— Judith Warner, New York Times, September 4, 2008
Why are we tolerating the use of junk science against those in the medical profession? A direct question that begs for a direct answer.
I am looking for a few honest and credible statisticians, biostatisticians or epidemiologists who want to make a difference in the spirit of service and helping others. I can’t pay you but you would be combating injustice, corruption and dishonesty. You would be doing your part in helping the Medical Profession, honest and decent doctors, our country and perhaps our future.
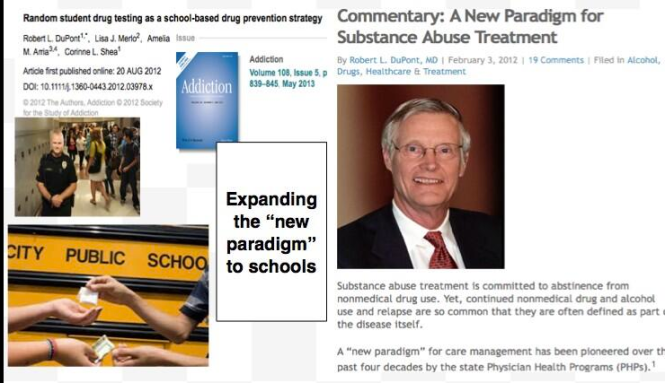
It is only a few public policy steps and minor changes in state regulatory statutes before what is described in the ASAM White Paper on Drug Testing comes to fruition. Before we know it the Drug and Alcohol Testing Industries “New Paradigm” as described here by Robert Dupont will be ushered in as it did with doctors; not with a bang but a whimper. From the ASAM white Paper:
“THIS WHITE PAPER ENCOURAGES WIDER AND “SMARTER” USE OF DRUG TESTING WITHIN THE PRACTICE OF MEDICINE AND, BEYOND THAT,BROADLY WITHIN AMERICAN SOCIETY. SMARTER DRUG TESTING MEANS INCREASED USE OF RANDOM TESTING* RATHER THAN THE MORE COMMON SCHEDULED TESTING,* AND IT MEANS TESTING NOT ONLY URINE BUT ALSO OTHER MATRICES SUCH AS BLOOD, ORAL FLUID (SALIVA), HAIR, NAILS, SWEAT AND BREATH WHEN THOSE MATRICES MATCH THE INTENDED ASSESSMENT PROCESS. IN ADDITION, SMARTER TESTING MEANS TESTING BASED UPON CLINICAL INDICATION FOR A BROAD AND ROTATING PANEL OF DRUGS RATHER THAN ONLY TESTING FOR THE TRADITIONAL FIVE-DRUG PANEL.”To prevent this future drug testing dystopia, that includes testing schoolchildren, we need to take a step back and analyze the reliability and credibility of the “evidence-base” behind these multiple non-FDA approved forensic drug and alcohol tests and testing devices the ASAM proposes be used on the population at large utilizing the Medical Profession as a urine collection agency and bypassing forensic drug testing protocol by calling this “evaluation” and treatment rather than “monitoring” and punishment. New definitions, loopholes, secrecy and subterfuge are the bread and butter of these prohibitionist profiteers.
Amazingly, there has been no Academic review of these tests, let alone a Cochrane type critical analysis. It is essentially untapped territory. In addition there has been no Institute of Medicine type Conflict of Interest Analysis. And that is why I am asking for help from statisticians, biostatisticians and epidemiologists. The task would entail a review of the literature prior to the introduction of these tests for evidence base of forensic applicability (there essentially is none) and a review of the literature peri-and post marketing of these devices to assess the reliability and credibility of the underlying methodology and ascertain the evidence-base. The goal would be publication in both academic journals and presentation to the general public through media publication with the assistance of investigative journalists and other writers. The goal is to get the truth out about these tests and allow both the medial profession and public at large to awaken to the menace this presents to medicine, our society and our future.Lack of Evidence-Base, Bias and Conflicts of Interest: Making the Data Fit the Hypothesis
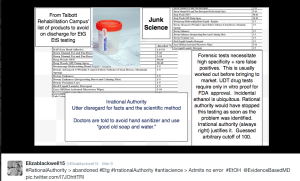
I am no epidemiologist or statistician but as with pornography I know junk-science when I see it. Almost all of these tests were introduced with little or no evidence-base and, as with most of their endeavors, they did it below board via loopholes and cutting corners.
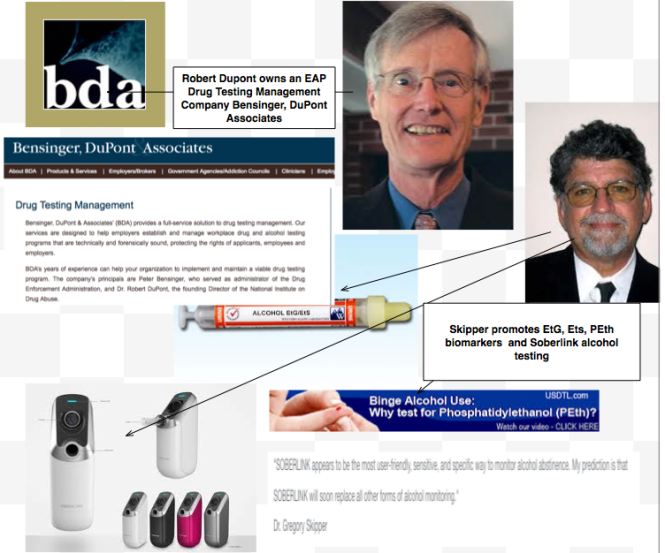
The overwhelming majority of papers are small, methodologically flawed, non-randomized, non-blinded retrospective studies in that appear to make the data fit the hypothesis. The authors can invariably be linked to those profiting from the tests of the testing process ( the patent holder, doctors associated with the drug testing labs, ASAM or FSPHP, Robert Dupont, Greg Skipper, etc.)
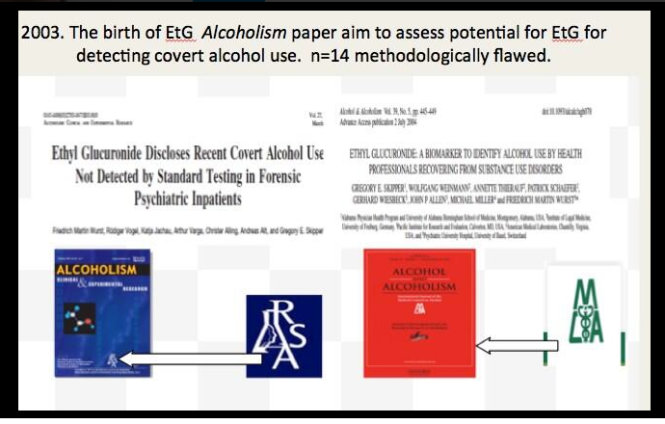
Ethyl Glucuronide (EtG) was introduced in 1999 as a biomarker for alcohol consumption,1 and was subsequently suggested as a tool to monitor health professionals by Dr. Gregory Skipper because of its high sensitivity to ethanol ingestion.2
Described as the “innovator of EtG as an alcohol biomarker,” Skipper and Friedrich Wurst, “convinced” NMS labs in Pennsylvania “to start performing EtG testing in 2002.
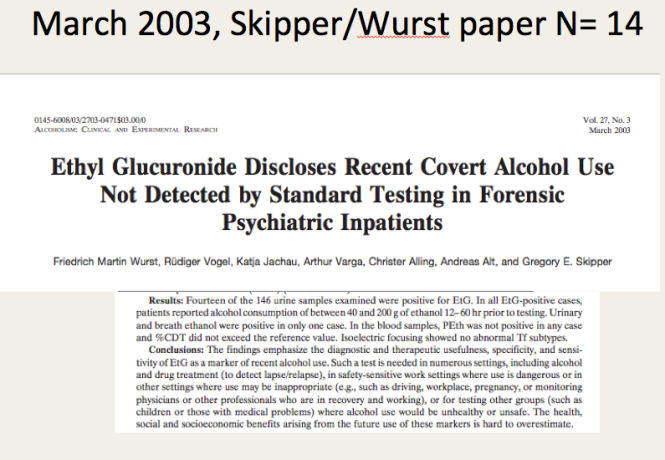
The study most often cited as 100% proof that there is 100% accuracy in EtG testing proving alcohol consumption involved a mere 35 forensic psychiatric inpatients in Germany that was published in 2003.3
Shortly thereafter the Physician Health Programs began using it in monitoring doctors and other professional monitoring programs soon followed.
 Laboratory Developed Tests -A Loophole to Avoid FDA Approval and Accountability
Laboratory Developed Tests -A Loophole to Avoid FDA Approval and Accountability
Up until the birth of the EtG tests used for forensic drug and alcohol monitoring had to go through the arduous, expensive and necessary FDA approval process. The LDT pathway was designed to develop simple tests with little risk that have low market potential (i;e. the cost of the normal FDA approval process would prohibit them from coming to market). The LDT pathway was designed to improve patient care and help improve diagnosis and treatment. It was not designed for forensic tests. LDT approval does not require in vivo testing. It is essentially an honor system and to develop an LDT it is not even necessary to prove that the test is actually testing what it is purportedly testing for (validity).
So with little to no evidence base they introduced the EtG, had it developed and marketed as a LDT in collusion with unscrupulous labs, and then began using it on physicians being monitored by State PHPs. This then spread to other monitoring organizations in which there was a large power-differential between those ordering the tests and those being tested (criminal-justice, other professional monitoring programs). These biomarkers have never been used in Federal Drug Testing, SAMHSA approved, DOT, and other organizations where unions or other organizations are present and looking out for the best interests of those being tested.
Another example of how this group removes accountability. There has been essentially no oversight or regulation of LDTs. Although there was a recent push for regulation of these tests the Drug and Alcohol Testing Industry Association lobby made sure that forensic tests would be exempt.They then began publishing “research” on the EtG using the physicians being monitored as subjects. Many of the studies promoting the EtG and other biomarkers can be found in Journals that are linked to organizations that are linked to AA and were organized to educate the medical community.
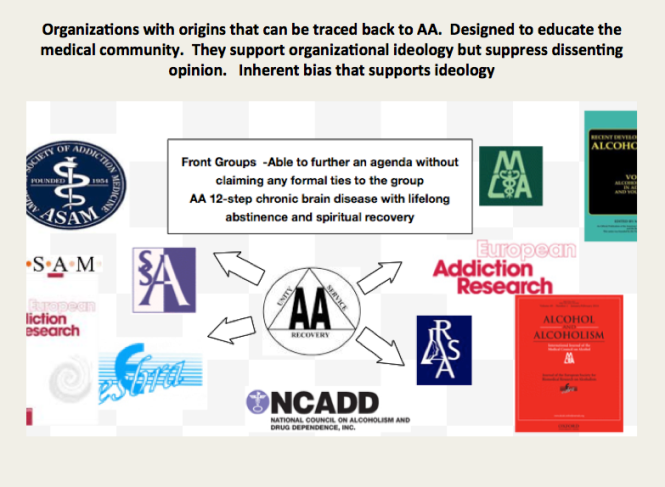
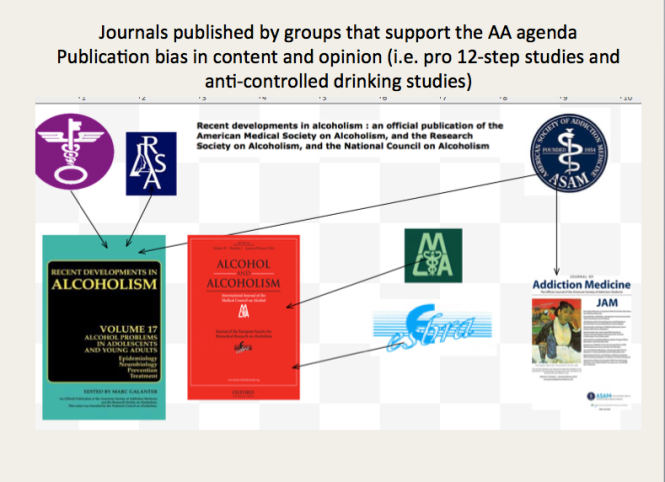 These small, methodologically flawed studies amount to little more than opinion pieces but This “evidence-base” is predominantly in biased journals published by biased medical “societies.
The EtG was subsequently found to be so sensitive that it could measure incidental exposure to alcohol in foods, over the counter cold medications, mouthwash4,5, hand sanitizer gel6, nonalcoholic beer7, and nonalcoholic wine.8 Sauerkraut and bananas have even been shown to cause positive EtG levels.9
The United States Substance Abuse and Mental Health Services Administration warned against using a positive EtG as primary or sole evidence of drinking for disciplinary or legal action.10 The Wall Street Journal in 2006 reported the problems with the EtG to the general public.11
These small, methodologically flawed studies amount to little more than opinion pieces but This “evidence-base” is predominantly in biased journals published by biased medical “societies.
The EtG was subsequently found to be so sensitive that it could measure incidental exposure to alcohol in foods, over the counter cold medications, mouthwash4,5, hand sanitizer gel6, nonalcoholic beer7, and nonalcoholic wine.8 Sauerkraut and bananas have even been shown to cause positive EtG levels.9
The United States Substance Abuse and Mental Health Services Administration warned against using a positive EtG as primary or sole evidence of drinking for disciplinary or legal action.10 The Wall Street Journal in 2006 reported the problems with the EtG to the general public.11
 As any rational authority would do, the majority of monitoring agencies abandoned the EtG after these flaws were revealed. The PHPs did not. They continued to use the EtG on doctors uninterruptedly by telling them to avoid any products that could potentially contain alcohol; a ubiquitous substance in the environment. Since that time they have justified and rationalized (EtG)2,12 13 use by sequentially raising cutoff levels from 100 to 250 to 500 to 1000 to 2000 to now unknown and adding other LDTs as “confirmation tests such as Ethyl Sulfate (EtS)14,15 Phosphatidyl-Ethanol ( Peth)16 17 and other devices such as the Subcutaneous Remote Alcohol Monitoring Bracelet (SCRAM) and, their newest device the Cellular Photo Digital Breathalyzer (CPDB) that has recently been launched, just like the EtG
As any rational authority would do, the majority of monitoring agencies abandoned the EtG after these flaws were revealed. The PHPs did not. They continued to use the EtG on doctors uninterruptedly by telling them to avoid any products that could potentially contain alcohol; a ubiquitous substance in the environment. Since that time they have justified and rationalized (EtG)2,12 13 use by sequentially raising cutoff levels from 100 to 250 to 500 to 1000 to 2000 to now unknown and adding other LDTs as “confirmation tests such as Ethyl Sulfate (EtS)14,15 Phosphatidyl-Ethanol ( Peth)16 17 and other devices such as the Subcutaneous Remote Alcohol Monitoring Bracelet (SCRAM) and, their newest device the Cellular Photo Digital Breathalyzer (CPDB) that has recently been launched, just like the EtG  with little to no evidence base other than a pilot study done by Greg Skipper and Robert Dupont.18
A 2013 article published in an ASAM incubated journal Alcoholism: Clinical and Experimental Research promotes the Phosphatidyl-ethanol (PEth ) test to confirm drinking.16 The study was done on physicians being monitored by the Alabama Physician Health Program who tested positive for EtG/EtS alcohol biomarkers. It is co-authored by Robert Dupont, Greg Skipper, and Friedrich Wurst and involved 18 subjects who tested positive for EtG/EtS of whom 7 claimed they did not drink. After finding that 5 of the 7 tested negative for PEth they concluded that “positive PEth testing following positive EtG/EtS results confirms recent drinking. Hard to wrap your head around the science in that one.
with little to no evidence base other than a pilot study done by Greg Skipper and Robert Dupont.18
A 2013 article published in an ASAM incubated journal Alcoholism: Clinical and Experimental Research promotes the Phosphatidyl-ethanol (PEth ) test to confirm drinking.16 The study was done on physicians being monitored by the Alabama Physician Health Program who tested positive for EtG/EtS alcohol biomarkers. It is co-authored by Robert Dupont, Greg Skipper, and Friedrich Wurst and involved 18 subjects who tested positive for EtG/EtS of whom 7 claimed they did not drink. After finding that 5 of the 7 tested negative for PEth they concluded that “positive PEth testing following positive EtG/EtS results confirms recent drinking. Hard to wrap your head around the science in that one. Skipper is also using both Scram ankle bracelets and the CPDB monitoring in pilots in the Human Interventional Motivational Study (HIMS) Program that was developed in 2009 to “identify, treat and, eventually, re-certify airline pilots with substance abuse problems.
Skipper is also using both Scram ankle bracelets and the CPDB monitoring in pilots in the Human Interventional Motivational Study (HIMS) Program that was developed in 2009 to “identify, treat and, eventually, re-certify airline pilots with substance abuse problems.

The Cochrane Collaboration does systematic reviews of the literature using conscientious, explicit, and judicious criteria to in order to produce and disseminate only high quality and evidenced based health care, exclude bias, and enhance transparency. The Cochrane database is a current and evolving database that includes the accuracy of diagnostic tests and is internationally recognized as the standard in evidence based health care. This benchmark for evidence based health care and systematic reviews, records just 5 controlled trials under the topic ethyl glucuronide.8,19-21 These 5 studies represent the only high-quality evidence regarding EtG applying to EtG. Information provided by the five studies suggests the following, and only the following:
- EtG and EtS measurements increase with alcohol ingestion.
- The window of detection is shorter than what is commonly proposed (80 hours).
- Individual values are variable both within and between subjects.
- Non alcoholic wine can cause positive levels.
Notably, there are no studies that fit Cochrane Criteria, other than non-alcoholic wine, that look at the pharmacokinetics of EtG or EtS in terms of dose-response curves, cut-off levels, specificity drug and food interactions, or modes of ingestion.
SAMHSA notes that there is little research on PEth and that EtG, EtS, and PEth “do not have a strong research base,” and that “it is not known at this time how the test results might be affected by the presence of physical diseases, ethnicity, gender, time, or the use of other drugs. Until considerable more research has occurred, use of these markers should be considered experimental.”
Phosphatidylethanol (PEth), SCRAM, and the yields no data as a test in the Cochrane library.
SAMHSA notes that there is little research on PEth and that EtG, EtS, and PEth “do not have a strong research base,” and that “it is not known at this time how the test results might be affected by the presence of physical diseases, ethnicity, gender, time, or the use of other drugs. Until considerable more research has occurred, use of these markers should be considered experimental.”
Evidence based medicine (EBM) can be defined as the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients.22
Medical progress and scientific advancement is occurring so fast that the volume of medical literature is expanding at a rate of greater than 7% per year.23
Evidence based medicine is not restricted to randomized trials and meta-analyses. It involves tracking down the best external evidence with which to answer our clinical questions.22
Expert opinion is the lowest level of evidence available in the EBM paradigm.24,25
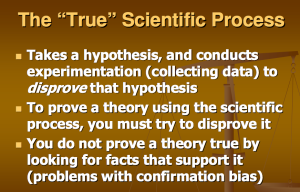
Fortunately, the scientific method is a tool to help people progress toward the truth despite their susceptibilities to confirmation bias and other errors.26
Unfortunately, due to a confluence of factors (including political) this has not been done. But, unless we want a future as envisioned by Robert Dupont and explained in the the ASAM White Paper on Drug Testing we need to act now. This is not a “New Paradigm” but a “New Inquisition.”
- Wurst FM, Kempter C, Seidl S, Alt A. Ethyl glucuronide–a marker of alcohol consumption and a relapse marker with clinical and forensic implications. Alcohol Alcohol. Jan-Feb 1999;34(1):71-77.
- Skipper GE, Weinmann W, Thierauf A, et al. Ethyl glucuronide: a biomarker to identify alcohol use by health professionals recovering from substance use disorders. Alcohol Alcohol. Sep-Oct 2004;39(5):445-449.
- Wurst FM, Vogel R, Jachau K, et al. Ethyl glucuronide discloses recent covert alcohol use not detected by standard testing in forensic psychiatric inpatients. Alcohol Clin Exp Res. Mar 2003;27(3):471-476.
- Costantino A, Digregorio EJ, Korn W, Spayd S, Rieders F. The effect of the use of mouthwash on ethylglucuronide concentrations in urine. J Anal Toxicol. Nov-Dec 2006;30(9):659-662.
- Reisfield GM, Goldberger BA, Pesce AJ, et al. Ethyl glucuronide, ethyl sulfate, and ethanol in urine after intensive exposure to high ethanol content mouthwash. J Anal Toxicol. Jun 2011;35(5):264-268.
- Rosano TG, Lin J. Ethyl glucuronide excretion in humans following oral administration of and dermal exposure to ethanol. J Anal Toxicol. Oct 2008;32(8):594-600.
- Thierauf A, Gnann H, Wohlfarth A, et al. Urine tested positive for ethyl glucuronide and ethyl sulphate after the consumption of “non-alcoholic” beer. Forensic Sci Int. Oct 10 2010;202(1-3):82-85.
- Hoiseth G, Yttredal B, Karinen R, Gjerde H, Christophersen A. Levels of ethyl glucuronide and ethyl sulfate in oral fluid, blood, and urine after use of mouthwash and ingestion of nonalcoholic wine. J Anal Toxicol. Mar 2010;34(2):84-88.
- Musshoff F, Albermann E, Madea B. Ethyl glucuronide and ethyl sulfate in urine after consumption of various beverages and foods–misleading results? Int J Legal Med. Nov 2010;124(6):623-630.
- Administration SAaMHS. The role of biomarkers in the treatment of alcohol use disorders. In: Advisory SAT, ed2006:1-7.
- Helliker K. A test for alcohol–and its flaws. The Wall Street Journal2006.
- Wurst FM, Skipper GE, Weinmann W. Ethyl glucuronide–the direct ethanol metabolite on the threshold from science to routine use. Addiction. Dec 2003;98 Suppl 2:51-61.
- Wurst FM, Alling C, Aradottir S, et al. Emerging biomarkers: new directions and clinical applications. Alcoholism, clinical and experimental research. Mar 2005;29(3):465-473.
- Anton RF. Commentary on: ethyl glucuronide and ethyl sulfate assays in clinical trials, interpretation, and limitations: results of a dose ranging alcohol challenge study and 2 clinical trials. Alcoholism, clinical and experimental research. Jul 2014;38(7):1826-1828.
- Hernandez Redondo A, Schroeck A, Kneubuehl B, Weinmann W. Determination of ethyl glucuronide and ethyl sulfate from dried blood spots. International journal of legal medicine. Jul 2013;127(4):769-775.
- Skipper GE, Thon N, Dupont RL, Baxter L, Wurst FM. Phosphatidylethanol: the potential role in further evaluating low positive urinary ethyl glucuronide and ethyl sulfate results. Alcoholism, clinical and experimental research. Sep 2013;37(9):1582-1586.
- Hahn JA, Dobkin LM, Mayanja B, et al. Phosphatidylethanol (PEth) as a biomarker of alcohol consumption in HIV-positive patients in sub-Saharan Africa. Alcoholism, clinical and experimental research. May 2012;36(5):854-862.
- Skipper GE, Thon N, DuPont RL, Campbell MD, Weinmann W, Wurst FM. Cellular photo digital breathalyzer for monitoring alcohol use: a pilot study. European addiction research. 2014;20(3):137-142.
- Hoiseth G, Bernard JP, Stephanson N, et al. Comparison between the urinary alcohol markers EtG, EtS, and GTOL/5-HIAA in a controlled drinking experiment. Alcohol Alcohol. Mar-Apr 2008;43(2):187-191.
- Wojcik MH, Hawthorne JS. Sensitivity of commercial ethyl glucuronide (ETG) testing in screening for alcohol abstinence. Alcohol Alcohol. Jul-Aug 2007;42(4):317-320.
- Sarkola T, Dahl H, Eriksson CJ, Helander A. Urinary ethyl glucuronide and 5-hydroxytryptophol levels during repeated ethanol ingestion in healthy human subjects. Alcohol Alcohol. Jul-Aug 2003;38(4):347-351.
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. Jan 13 1996;312(7023):71-72.
- Norwitz ER, Greenberg JA. Promoting evidence-based medicine. Rev Obstet Gynecol. Summer 2008;1(3):93-94.
- Shaneyfelt TM, Centor RM. Reassessment of clinical practice guidelines: go gently into that good night. JAMA. Feb 25 2009;301(8):868-869.
- Straus SE, Green ML, Bell DS, et al. Evaluating the teaching of evidence based medicine: conceptual framework. BMJ. Oct 30 2004;329(7473):1029-1032.


“There comes a time when silence is betrayal.” ― Martin Luther King Jr.




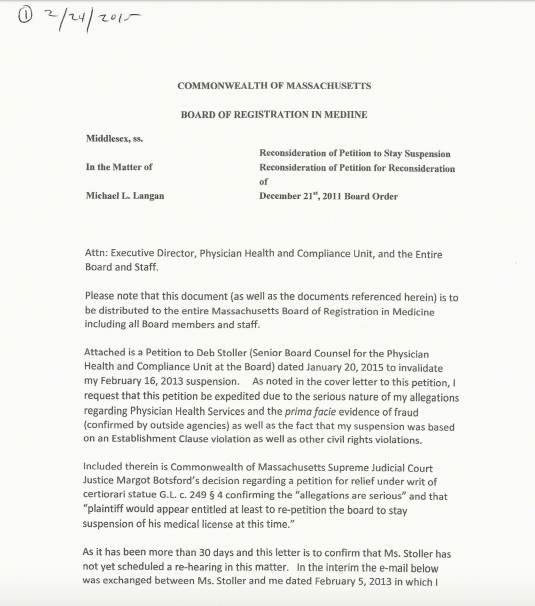
Massachusetts Board Attorney Deb Stoller’s “Fraud on the Court”–Accountability and Consequences Imperative
The plan to expand Physician Health Programs (PHPs) to all professionals

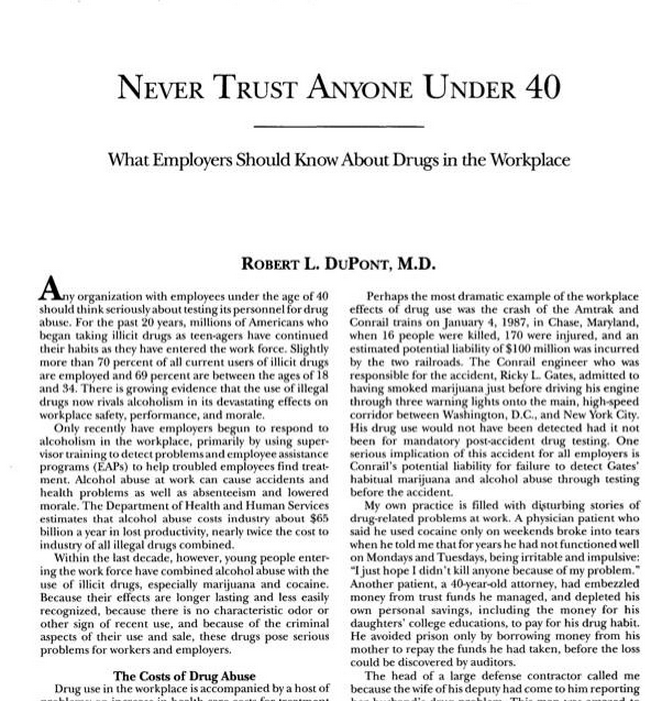
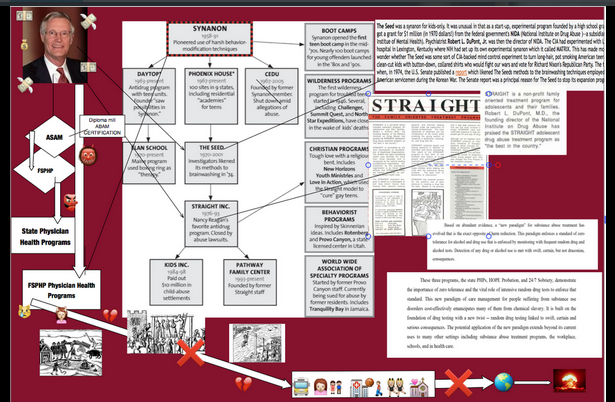
In 2012 former Nixon Drug Czar Robert Dupont, MD delivered the keynote speech at the Drug and Alcohol Testing Industry Association (DATIA) annual conference and described a “new paradigm” for addiction and substance abuse treatment. He advocated zero tolerance for alcohol and drug use enforced by monitoring with frequent random drug and alcohol tests. Detection of any substances is met with “swift and certain consequences.”
And then he proposed expansion of this paradigm to other populations including workplace, healthcare, and schools.
Robert Dupont was a key figure in launching the “war on drugs” — now widely viewed as the failed policy that has turned the US into the largest jailer in the world.
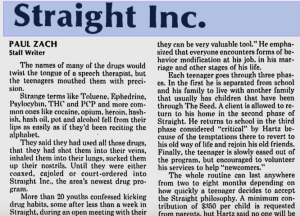
 In the 1970s, Dupont administered the experimental drug rehab program called “The Seed” – that was later deemed by congress to use methods similar to those used on American POW’s in North Korea. He would later go on to consult for “Straight, Inc”, a rehab program that treated troubled teens as “addicts”, often for minor infractions or normal teenage behavior.
In the 1970s, Dupont administered the experimental drug rehab program called “The Seed” – that was later deemed by congress to use methods similar to those used on American POW’s in North Korea. He would later go on to consult for “Straight, Inc”, a rehab program that treated troubled teens as “addicts”, often for minor infractions or normal teenage behavior.
Deemed the “family oriented treatment program,” Dupont encouraged organization and expansion. Targeting the children of wealthy white families parents fears were used to refer their kids to the programs. Signs of hidden drug use such as use of Visine, altered sleep patterns, and changes in clothing style were used as indications for referral. Any child who arrived would be considered an addict in need of their services. Coercion, confrontation, command and control were the guiding principles. Submit or face the consequences. We know what’s right. The idea was to strip the child of all self-esteem and then build him back up again in the straight image. Abused, dehumanized, delegitimized and stigmatized-the imposition of guilt, shame, and helplessness was used for ego deflation to facilitate canned and condensed 12-step as a preparatory step on the path of lifelong spiritual recovery.
Children were coaxed or terrorized into signing confessions, berated, and told they were in “denial.” Inaccurate and false diagnoses were given to wield greater control. Reports and witness accounts now indicate that many of the kids did not even have drug problems but by creating a “moral panic” about teenage drug use they exploited parents fears for profit. Straight, Inc. became the biggest juvenile rehabilitation center in the world for rehabilitation and treatment of addiction.
12 year old girl admitted to inpatient addiction rehabilitation for sniffing a “magic marker”–Once!
A Deficiency Correction Order was issued by the Executive Office of Human Services, Office of Children, Commonwealth of Massachusetts Services to Straight, Boston in 1990 that read in part:
| “Although Straight’s statement of services states that Straight serves chemically dependent adolescents, a review of records and interviews with staff demonstrate that Straight admits children who are not chemically dependent. For example, one twelve-year-old girl was admitted to the program although the only information in the file regarding use of chemicals was her admission that she had sniffed a magic marker.” |
Straight was always making outlandish claims of success but there was no scientific evidence based data to support it. In September 1986 USA TODAY ran an article headlined: DRUGS: Teen abusers start by age 12 which opened with: “Almost half of the USA’s teen drug abusers got involved before age 12…”
The article was based on a study conducted by Straight, Inc.
Many former patients of Straight were so devastated by the abuse that they took their own lives. Since then, Dupont has been a key figure in the proliferation of workplace drug testing programs, and once advocated for drug testing anyone in the workplace under the age of 40.1,2
The Physician Health Program (PHP) blueprint is essentially Straight, Inc. for Doctors in both Mechanics and Mentality
The “new paradigm” Dupont speaks of before the Drug and Alcohol Testing Industry Association is modeled after state physician health programs (PHPs) and as was done with Straight, “remarkable” claims of success are being made.3-6 Promoted as “Setting the standard for recovery” PHPs are now being pitched to other populations7
 Dupont and Dr. Greg Skipper proclaim the “need to reach more of the 1.5 million Americans who annually enter substance abuse treatment, which now is all too often a revolving door.”8 They conclude:
Dupont and Dr. Greg Skipper proclaim the “need to reach more of the 1.5 million Americans who annually enter substance abuse treatment, which now is all too often a revolving door.”8 They conclude:
This model of care management for substance use disorders has been pioneered by a small and innovative group of the nation’s physicians in their determination to help other physicians save their careers and families while also protecting their patients from the harmful consequences of continued substance abuse. In fulfilling the professional admonition “physician: first heal thyself,” these physicians have created a model with wide applicability and great promise.8
In “Six lessons from state physician health programs to promote long-term recovery” Dupont and Skipper attribute this success rate to the following factors:8
(1) Zero tolerance for any use of alcohol and other drugs;
(2) Thorough evaluation and patient-focused care;
(3) Prolonged, frequent random testing for both alcohol and other drugs;
(4) Effective use of leverage;
(5) Defining and managing relapses; and
(6) The goal of lifelong recovery rooted in the 12-Step fellowships.8
 As with Straight, the majority of those admitted to PHPs are not even addicts. The Federation of State Physician Health Programs (FSPHP) was able to convince Federation of State Medical Boards, to adopt the notion of “potentially impairing” illness and “relapse without use” to promote early intervention using the same false logic as Straight, Inc. and the 12-year old with the magic marker. ( i.e. teen drug abuse starts by age 12 and that any sign or symptom inexorably progresses to impairment justifying “treatment”).
As with Straight, the majority of those admitted to PHPs are not even addicts. The Federation of State Physician Health Programs (FSPHP) was able to convince Federation of State Medical Boards, to adopt the notion of “potentially impairing” illness and “relapse without use” to promote early intervention using the same false logic as Straight, Inc. and the 12-year old with the magic marker. ( i.e. teen drug abuse starts by age 12 and that any sign or symptom inexorably progresses to impairment justifying “treatment”).
Signals for “impairment” can be as benign as not having “complete, accurate, and up-to-date patient medical records.” according to Physician Health services, the Massachusetts Physician Health Program and subsidiary of the Massachusetts Medical Society.
Despite the overwhelming amount of paperwork physicians now have, incomplete or illegible records could be construed as a red flag, since, as Associate Director of PHS Judith Eaton notes“when something so necessary is not getting done, it is prudent to explore what else might be going on.”
It is a false premise “feel-good fallacy” with faulty conclusions. And because it is being perpetrated on doctors (and those in the criminal-justice system) no one seems to care. But this is merely a wedge for a grander plan.
Dupont has been heavily involved in studies using non-FDA approved laboratory developed tests and other devices of unknown validity on doctors in PHPS and promoting the use of these tests for forensic monitoring.9,10
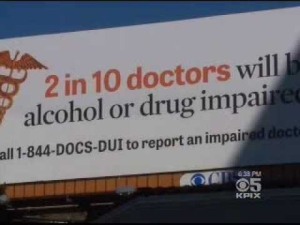
And they want to bring these tests to you.Propaganda and misinformation has been designed to sway public opinion.
A Medscape article from “Drug abuse among Doctors: Easy, Tempting, and Not Uncommon” is a prototypical example of the propaganda and misinformation being used to sway public policy and opinion. Focusing on a small study ( n =55) done by Lisa Merlo (Director of Research for the Florida PHP). Dr.Marvin Seppala states in the article that impaired doctors are:
“….often described as the best workers in the hospital,” he says. “They’ll overwork to compensate for other ways in which they may be falling short, and to protect their supply. They’ll sign up for extra call and show up for rounds they don’t have to do.” Physicians are intelligent and skilled at hiding their addictions, he says. Few, no matter how desperate, seek help of their own accord.”
There is no evidence base for a hidden cadre of drug-impaired doctors causing medical error. A critical review of the literature reveals no evidence base exists. Moreover, this blather does not even comport with reality. It defies reason and even basic common sense.
 But through misinformation and deceptive propaganda similar to that used by Straight these groups have created “moral panics” aimed at physicians designed to separate them from everyone else.
But through misinformation and deceptive propaganda similar to that used by Straight these groups have created “moral panics” aimed at physicians designed to separate them from everyone else.
To be sure, doctors who are practicing impaired due to substance abuse need to be removed from practice both to get the help they need and to protect the public. But that is not what is happening. Instead, what is occurring is that doctors can get caught up in this system for any number of reason. Indeed, some of these physicians have no history of drug-addiction—they are the equivalents of the 12-year-old girl caught sniffing a magic marker.
And this is how the scam works.
When doctors monitored by their PHP test positive they are forced to have an evaluation at a “PHP-approved” treatment center. In 2011 the American Society of Addiction Medicine (ASAM) issued a Public Policy Statement recommending physicians in need of assessment and treatment be referred only to “PHP approved” facilities. The medical directors of the “PHP-approved” facilities can be found on this list of “Like-Minded Docs”.
In 2011, The organization that oversees the licensing for all medical doctors, the Federation of State Medical Boards, adopted a new policy and approved the concept of “potentially impairing illness.” and the Orwellian notion of drug “relapse without use.”
This implies that they will be able to ruin any doctor who does not comply or who is found guilty, even if fraudulently.
The question might be, “Why?” As with anything, we have to think about who profits.
Indeed, Dupont has remained a vocal and influential spokesman for drug and alcohol testing. But he along with former DEA head Peter Bensinger run a corporate drug-testing business. Their employee-assistance company, Bensinger-Dupont is the sixth largest in the nation.
Now, they also want to extend these tests to drivers.11,12 and Federal Workplace Drug Testing Programs.
They would like to replace the current system used in pilots, bus drivers, and Federal Employees with “comprehensive drug and alcohol testing.”13 AND THEY ARE promoting hair testing, 14Their goal is 24/7 sobriety with complete abstinence 15, and zero tolerance.16
Their claims of success are based on a single retrospective cohort study looking at the outcomes of 904 physicians monitored by 16 different State PHPs.17
An 80% success rate is claimed but 102 of the 904 participants were “lost to follow up” and of the remaining 802, 155 failed to complete the contract.
So what happened to the 24 of who “left care with no apparent referral,” the 85 who “voluntarily stopped or retired,” and the 48 who “involuntarily stopped” or had their “license revoked.” Whether you leave a PHP voluntarily, involuntarily, or with no apparent referral it is the end.. The plug is pulled. Game over. Comparing this to other populations where the consequences are not as terminal is like comparing apples to oranges.
But the bigger question is what happened to the 157 physicians who left or stopped? How many of those killed themselves. The study reports 6 suicides, 22 deaths, and another 157 who are no longer doctors. How many of the 22 deaths were suicides and what happened to the 157 who stopped for no apparent reason? Using the last recorded clerical status as an endpoint obfuscates the true endpoints. Where are they now? Alive or dead?
Propaganda and misinformation is designed to sway public opinion and it is all hidden from public view and scrutiny. Absolutely no oversight or regulation from outside agencies exists for PHPs and very little exists for the “PHP-approved” up-front cash only assessment and rehabilitation facilities. The commercial drug-testing labs using non-FDA approved LDTs have no accountability either. No agencies exist to hold them accountable for errors or even intentional misconduct. The College of American Pathologists (CAP) is the only avenue for complaint and CAP is an accreditation agency that can only “educate” not “discipline.” It is a system that fosters and fuels misconduct as no consequences exist for wrongdoing and they built it that way.
The American Society of Addiction Medicine erected this scaffold state-by-state. And that is how it must be removed. It is a system of coercion, control, and fear. Crimes like the ones being committed here in Massachusetts must be investigated as crimes. The perpetrators must be held accountable.
It is a system of institutional injustice that is killing physicians by driving them to hopelessness, helplessness, and despair. The general medical community needs to awaken to the reality of the danger to expose and dismantle it at the State level. And many of the doctors caught in this maw do not even have an addiction or substance abuse issue –equivalent to the 12-year old girl in referred to Straight for sniffing a magic marker. On the other hand many of those in charge of the administration of these programs have engaged in egregious even horrific misconduct and have a history of manipulating the system.
Secondly, all of the so-called “research” must be subject to evidence base review. It is not there.
And thirdly, the numerous, intertwined and myriad conflicts of interest must be addressed because it’s money that is the big driver of this “benevolent” interest in whether or not you are sober.
With over 20 years experience as Associate Directors of the Massachusetts PHP, Physician Health Services, Inc. (PHS,inc.), Dr.’s J Wesley Boyd, MD, PhD and John R. Knight of Harvard Medical School published an Ethical and Managerial Considerations Regarding State Physician Health Programs pointing out serious conflicts of interest and ethical issues involving PHP programs and the need “to review PHP practices and recommend national standards that can be debated by all physicians, not just those who work within PHPs.”
They recommend ethical oversight of PHPs, a formal appeals process for physicians, periodic auditing, a national system for licensing, and recommend “the broader medical community begin to reassess PHPs as a whole in an objective and thoughtful manner.” Unfortunately, this has not occurred. It urgently needs to because the Physician Health Program “Blueprint” is essentially Straight inc. in both mechanics and mentality. Doctors are being forced into treatment when they do not need treatment just like the magic-marker sniffing 12-year old. Those who do not meet the diagnostic criteria for a disease are being intentionally misdiagnosed with a disease in order to charge for the unnecessary testing and treatment of that disease. It is a system of abuse, coercion, control and institutional injustice and as was seen with Straight, Inc., many are taking their own lives. ASAM public policy is recommending the PHP paradigm be expanded to all professionals and they don;t need your permission to do so. The only entities needed to bring this to fruition are those involved in the regulation of your profession.
- Engs RC. Mandatory random testing needs to be undertaken at the worksite. Controversies in the Addiction Field. Vol 1. Dubuque, IA: Kendall/Hunt; 1990:105-111.
- Dupont RL. Never trust anyone under 40: What employers should know about Molly Kellogg in the workplace. Policy Review. Spring 1989:52-57.
- DuPont RL, McLellan AT, Carr G, Gendel M, Skipper GE. How are addicted physicians treated? A national survey of Physician Health Programs. Journal of substance abuse treatment. Jul 2009;37(1):1-7.
- White WL, Dupont RL, Skipper GE. Physicians health programs: What counselors can learn from these remarkable programs. Counselor. 2007;8(2):42-47.
- Skipper GE, Campbell MD, Dupont RL. Anesthesiologists with substance use disorders: a 5-year outcome study from 16 state physician health programs. Anesthesia and analgesia. Sep 2009;109(3):891-896.
- Yellowlees PM, Campbell MD, Rose JS, et al. Psychiatrists With Substance Use Disorders: Positive Treatment Outcomes From Physician Health Programs. Psychiatric services. Oct 1 2014.
- DuPont RL, McLellan AT, White WL, Merlo LJ, Gold MS. Setting the standard for recovery: Physicians’ Health Programs. Journal of Medical Regulation. Mar 2010;95(4):10-25.
- Dupont RL, Skipper GE. Six lessons from state physician health programs to promote long-term recovery. Journal of psychoactive drugs. Jan-Mar 2012;44(1):72-78.
- Skipper GE, Thon N, Dupont RL, Baxter L, Wurst FM. Phosphatidylethanol: the potential role in further evaluating low positive urinary ethyl glucuronide and ethyl sulfate results. Alcoholism, clinical and experimental research. Sep 2013;37(9):1582-1586.
- Skipper GE, Thon N, DuPont RL, Campbell MD, Weinmann W, Wurst FM. Cellular photo digital breathalyzer for monitoring alcohol use: a pilot study. European addiction research.2014;20(3):137-142.
- Voas RB, DuPont RL, Talpins SK, Shea CL. Towards a national model for managing impaired driving offenders. Addiction. Jul 2011;106(7):1221-1227.
- DuPont RL, Voas RB, Walsh JM, Shea C, Talpins SK, Neil MM. The need for drugged driving per se laws: a commentary. Traffic injury prevention. 2012;13(1):31-42.
- Reisfield GM, Shults T, Demery J, Dupont R. A protocol to evaluate drug-related workplace impairment. Journal of pain & palliative care pharmacotherapy. Mar 2013;27(1):43-48.
- DuPont RL, Baumgartner WA. Drug testing by urine and hair analysis: complementary features and scientific issues. Forensic science international. Jan 5 1995;70(1-3):63-76.
- Caulkins JP, Dupont RL. Is 24/7 sobriety a good goal for repeat driving under the influence (DUI) offenders? Addiction. Apr 2010;105(4):575-577.
- DuPont RL, Griffin DW, Siskin BR, Shiraki S, Katze E. Random drug tests at work: the probability of identifying frequent and infrequent users of illicit drugs. Journal of addictive diseases. 1995;14(3):1-17.
- McLellan AT, Skipper GS, Campbell M, DuPont RL. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. Bmj. 2008;337:a2038.
And the stars look very different today- Goodnight Thin White Duke

Life on Mars
It’s a God-awful small affair
To the girl with the mousy hair
But her mummy is yelling no
And her daddy has told her to go
But her friend is nowhere to be seen
Now she walks through her sunken dream
To the seat with the clearest view
And she’s hooked to the silver screen
But the film is a saddening bore
For she’s lived it ten times or more
She could spit in the eyes of fools
As they ask her to focus on
Sailors fighting in the dance hall
Oh man look at those cavemen go
It’s the freakiest show
Take a look at the lawman
Beating up the wrong guy
Oh man wonder if he’ll ever know
He’s in the best selling show
Is there life on Mars?
It’s on America’s tortured brow
That Mickey Mouse has grown up a cow
Now the workers have struck for fame
‘Cause Lennon’s on sale again
See the mice in their million hordes
From Ibiza to the Norfolk Broads
Rule Britannia is out of bounds
To my mother, my dog, and clowns
But the film is a saddening bore
‘Cause I wrote it ten times or more
It’s about to be writ again
As I ask you to focus on
Sailors fighting in the dance hall
Oh man look at those cavemen go
It’s the freakiest show
Take a look at the lawman
Beating up the wrong guy
Oh man wonder if he’ll ever know
He’s in the best selling show
Is there life on Mars?
Guest Post: Dr. Daniel Vande Lune, MD discusses how HCQIA provided immunity is misused by hospitals for sham peer-review
The Ability for Hospitals to Hide behind the Immunity of HCQIA and the Abuse and Coercion by the PHP: my story and caveats.
I have been asked to write a guest blog and whole heartedly agreed. I am not afraid to tell my story and indeed, I feel that physicians need to know my story, so they don’t become yet another victim. This story really isn’t any different that a lot of other physician’s experiences. I want to be certain it is understood that my story is two-fold; violation of due process, breach of contract, and a sham peer review on the hospital’s part and a myriad of violations including roughshod disregard for civil liberties, committed by the North Carolina Physicians’ Health Program. Unfortunately, most physicians have no idea about many of the legal aspects that surround our careers, nor do they have any idea the power a hospital or PHP can wield.
In 1986, HCQIA (Health Care Quality Improvement Act) passed into law. On the outside, this act looked like a good thing because it tried to reign in escalating medical malpractice cases, and to protect people from those physicians. Quite generally, it allows physicians to be reviewed by their peers without the threat of civil litigation by the physician being reviewed. There are many points that have to be met in order for a peer review organization to stand behind HCQIA and earn its immunity. Again, unfortunately, because of this immunity, doctors can become the victim of a Sham Peer Review.
Lawyer, Gregory Piché, who has experience representing not only physicians but also hospitals in these matters, has written an excellent book, Sham Peer Review: The Power of Immunity and Abuse of Trust. While the book duly notes that it is very hard for physicians to fight back against a perceived sham peer review, it is not impossible. There are a multitude of reasons why a doctor might be targeted, for example, professional jealousy or competition. In the second chapter of his book he outlines 12 signs that you may be a victim of a sham peer review. I won’t enumerate those here but, they are eye opening. In my story, I was able to check off 10 of the 12 warning signs.
So enough background for now, let’s get on with my personal example. In November 2013, I was accused of misbehavior at the outpatient surgery center associated with Johnston Medical Center (Smithfield, North Carolina). Four staff members, who were kept anonymous from me, accused me of throwing an instrument and later that same day, striking a patient. Heinous behavior. I didn’t recall anything special from the day in question, I still stand by my side of the events. The instrument I was accused of throwing was a retractor. We were doing an arthroscopic case and thus no retractors were being used. All I can guess is that when we converted to an open procedure, I may have gently tossed the arthroscopic cannula onto the back table. The second accusation, again most heinous, was in a large man who was having hand surgery under a Bier block with sedation. He repeatedly moved and fidgeted, at one point sitting bolt upright on the operating table. I forcibly grabbed his wrist, still attached to a lead hand, and placed it firmly on the operating table, making a thudding sound. I certainly did not strike this patient, that violates my personal rules of honor and integrity. Skipping way ahead for a moment, I eventually had a Fair Hearing through the hospital’s administrative remedies, at which time only one of the accusers showed up. She was not a credible witness and in the end stated that the others hadn’t witnessed anything visually.
Mind you, these events supposedly took place in November of 2013. I was not made aware of it until December and didn’t go before the MEC until January. This is where it is very important to know the bylaws or to review them should you find yourself in a similar position. Under the bylaws I was to have been notified in writing and provided with details concerning the accusastion. Yet, I received only a phone call and then was not told any details of the accusations. Additionally, as a first time report, this should have gone to the head of the surgery department, not directly to the MEC. It should have been handled internally. This was the first violation of their bylaws. In North Carolina, failure to follow your bylaws is considered a breach of contract. From this point on they were violating my rights of due process. Because of the violations of their bylaws, due process, and their breach of contract, they have no right to stand behind the immunity of HCQIA. I wish I knew then what I know now. I should have looked at my bylaws and hired counsel before attending a meeting with the MEC. However, I figured that my explanation would ring true with my “peers.” Another mistake. I did ask about having a lawyer present but I was told that would not be allowed, which is probably true under the bylaws, but certainly is another personal violation of representation.
I presented myself to the MEC and gave my side of the story but I was rebuffed. They investigated and told me they believed my accusers, the same accusers that DID NOT show up to my fair hearing eight months later. I was told that I would be “voluntarily required,” an oxymoron, to go the North Carolina Physicians’ Health Program to be evaluated. The oxymoron was explained as such: if they made it required, they would have to immediately report me to the NPDB. However, it was not voluntary in that my privileges were threatened if I didn’t attend. As I was planning to move out of North Carolina within six months, I agreed simply to keep the peace and move on without issue. I was given assurances by the Vice President of Medical Affairs that the evaluation would be kept confidential and that if anything came of the visit, it would be recommendations only. I, like many others, had never heard of the PHP before.
Due to scheduling issues, I was unable to be evaluated until late February, meanwhile still practicing and working out of this hospital; I was covering their ER, performing consults, and bringing them surgical cases (revenue). I presented for my evaluation, confirmatory email in hand, only to be told that I didn’t have an appointment that day and would need to reschedule. Fine, although I was convinced that was a test of my patience something that has been confirmed by others. Again, due to scheduling issues, (travel for interviews, death of a friend, and on call requirements), I didn’t get seen until early April. I was eventually accused, by the hospital, that I was purposefully delaying my evaluation. Much to my amazement, upon presenting, I was told that I would have to have a urine drug screen and that I would have to pay for it! This was not mentioned ahead of time, although the receptionist who had erred with my initial appointment, commented that I had been told. I was also told, by the psychiatrist, that there was no doctor-patient relationship and he could report me to any authorities he saw fit. Despite me signing a release, I feel that without a doctor-patient relationship, he never had the authority to see my subsequent test results. Certainly, an argument can me made about a HIPAA violation on his part. To this point I have had my 5th and 14th Amendment rights violated by the hospital. NCPHP is probably guilty of illegal search and seizure as well as invasion of privacy.
We haven’t even started the evaluation. We began our talk. Not more than 15 minutes into the evaluation, he was trying to strong-arm me in to a contract with the PHP which would follow me to any future state where I might work. I refused, as I had been guaranteed that I was there for recommendations only. I answered all questions voluntarily, wanting to present myself as open and willing, not an “angry person.” I never refused a question, answering some of the most intimate questions possible. During this evaluation, I was never asked the 20 Questions of Johns Hopkins nor the CAGE questions. I was simply asked about consumption of alcohol which I didn’t deny. I have never been accused of coming to work impaired nor have I had any legal issues related to the social use of alcohol.
As the evaluation ended, I was escorted to and joined in the restroom by the psychiatrist, who was present as I provided a sample. Humiliating and violating. I then asked what drugs it tested for; I was told 12 drugs and alcohol. I balked as I had told him that I used alcohol socially. The urine was in his possession and I was told “not to worry about it.” Of course, the test came back positive for ethanol metabolites. As my evaluation was on Friday, the test result was communicated to me on Monday. At this point, the NCPHP recommended to the hospital that I undergo an evaluation for anger management as well as substance abuse. Remember, I had never been accused of impairment and this was a single isolated test. The courses were expensive and out-of-state. I refused anything to do with substance abuse evaluation or monitoring – which required the out-of-state evaluation or six months of draconian monitoring. I was especially concerned about travel restrictions under the monitoring contract as my daughter was getting married back in the Midwest. I was told they couldn’t guarantee that I could travel for her wedding. Obviously, that was a deal breaker.
At this point, I appealed to the hospital, offering to attend local anger counseling for which I would pay and I even offered to undergo urine testing at the hospital. The hospital continued to rebuff my concessions and attempts at coming to an amicable middle-of-the-road solution. I finally hired a lawyer who made it plain that signing a contract with the NCPHP was not a good thing. It was roughly at this time that the State Auditor in North Carolina released her report on the NCPHP. With all of the stories I know, it’s hard to believe that they didn’t find more evidence of malfeasance in reviewing 100 charts. They did find conflict of interest issues and recommended that physicians be allowed to seek their own care. Despite this recommendation, I was not afforded that opportunity. I presented this information to the MEC along with position statements from SAMHSA (they are against use of an isolated positive test and don’t believe the EtG test should be used as the sole forensic test especially when dealing the career of a professional), as well as reports condemning the EtG test (it is not approved by the FDA). Again, I was rebuffed.
In early May, after failing to sign the contract, I was summarily suspended from the hospital. Again, the bylaws were violated as I did not meet any of the definitions for a summary suspension. Why after six months was I suspended summarily? If they were so concerned, I should have been suspended the previous November. After 30 days, by federal mandate, I was reported to the NPDB and subsequently investigated by the NCMB. I was released from my contract at Duke University. Although my license was never suspended, revoked, or restricted, I have been unable to get even a locums job. I have been rejected by at least three hospitals in Iowa. I’m working towards a Texas license but I’m finding that to be quite difficult. The hospital and PHP have continued to hide behind the veil of immunity. The violations of due process and breach of contract cannot be questioned which eliminates that immunity. The bigger concern is violation of civil liberties committed by both institutions.
Interestingly, the NCMB investigated and asked that I seek another evaluation, for anger management, with a counselor. They gave me a short list of providers in Iowa City, where I had relocated with my family. I went to one visit and she found no issues, other than an adjustment disorder stemming from the way I had been treated. I thought one visit rang hollow, so I pretty much begged the counselor to give me some recommendation. She said I could possibly benefit from a course in communication. Again, from a list of their choosing (the NCMB), I completed an at home course that dealt with communication and anger management.
Meanwhile, the hospital continued to hide behind the recommendations of the NCPHP. They would not back down from that. I eventually was given a Fair Hearing. After three nights of testimony in August and September of 2014, I was vindicated. The panel said that there was not enough evidence to have sent me for an evaluation in the first place, making everything following that moot. One of them has called it a witch hunt; a sham peer review. This decision was remanded by the MEC back to the panel who stuck to their initial decision. However, the MEC refused to overturn my suspension, which is allowed according to the bylaws. An appellate review also fell on deaf ears.
I think this story has many take home points. It never hurts to get a lawyer involved, the earlier the better. I firmly believe that had I involved a lawyer in January of 2014, I may never have had to go for an evaluation at the PHP. Know or review your hospital bylaws if you are ever in any situation with a hospital. Although I was given assurances that only recommendations would be made, the hospital hid behind their HCQIA immunity and the PHP, both entities holding my license/privileges over my head. Get everything in writing. Avoid any PHP, unless you feel you truly need their help, voluntarily. Even then, consider an evaluation by a trusted community colleague. The NCPHP is very typical of these organizations throughout the country, its modus operandi is addiction medicine. They base all of their recommendations on the spiritual 12-step program of alcoholics anonymous and the disproven belief that physicians need more intense treatment, junk science as most people call it. Like most of these institutions, they do not treat patients. They evaluate and refer you to an expensive out-of-state course, where you will most likely be entrapped in a prolonged, never ending contract with the PHP. It has been well documented that if you attend a substance abuse evaluation, you will most likely be labeled an abuser, ending up with 90 days of inpatient treatment. Lastly, be aware of the warning signs of a sham peer review, especially if you are just starting in a new position. Physicians are proud and territorial and they are not always “their brother’s keeper.”
I continue to fight for my professional career but the road blocks are enormous. Finding a lawyer to file suit, on a contingency basis, has also been impossible. As physicians, we need to stand up to these inequities. We need to support each other and contemplate the future when we may need to band together in a class action lawsuit. Maybe it’s time the ACLU becomes truly involved and excited about this opportunity.
Daniel Vande Lune, M.D.