 In Bending Science: How Special Interests Corrupt Public Health Research 1 Thomas McGarity and Wendy Wagner describe how special interest groups scheme to advance their own economic or ideological goals by using distorted or “bent” science to influence legal, regulatory and public health policy.
In Bending Science: How Special Interests Corrupt Public Health Research 1 Thomas McGarity and Wendy Wagner describe how special interest groups scheme to advance their own economic or ideological goals by using distorted or “bent” science to influence legal, regulatory and public health policy.
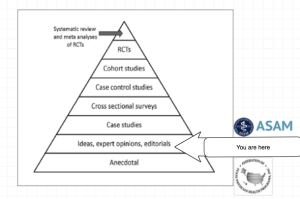
The authors describe a “separatist view” of science and policy that assumes scientific research is sufficiently reliable for public policy deliberations and legal proceedings when it reaches them. This is illustrated as a pipeline in which it is presumed the scientific community has properly vetted the information flow through rigorous peer-review and professional oversight. The final product that exits the pipeline is understood to be unbiased and produced in accordance with the professional norms and procedures of science. The reliability, integrity and validity of the final product is indubitably accepted. The separatist view does not consider the possibility that the scientific work exiting the pipeline could be intentionally shaped and contaminated by biasing influences as it flows through the pipeline. When this occurs the final product exiting the pipeline is distorted or “bent” and bent science can result in bad decision making and bad policy.
The separatist view does not consider the possibility that the scientific work exiting the pipeline could be intentionally shaped and contaminated by biasing influences as it flows through the pipeline. When this occurs the final product exiting the pipeline is distorted or “bent” and bent science can result in bad decision making and bad policy.
Bent science starts with a pre-determined outcome and works backward from a desired result. It is not true science. Those orchestrating the deception (“benders”) use a variety of tactics and strategies to shape, package and spin science to support their own hidden agenda and suppress opposing science.
Benders attempt to hide, dismiss and debunk contrarian research and unsupportive science. Benders will attack and harass the science and scientists that pose a threat to their interests. Using carefully crafted studies designed to confirm a desired outcome, the pre-determined conclusions are subsequently promoted and publicized to the relevant stakeholders who are often unable ( or sometimes unwilling) to discern real science from junk-science.
Misinformation, propaganda, and deception are disseminated in a variety of venues. Public relations firms are used to manipulate public perception and freelance writers are hired brandish favorable consensus statements. Authoritative reviews and critiques are ghostwritten under the names of “outside experts” who profit both monetarily and by adding a high-profile publication to their resume.
Opinion is paraded as fact and with a dearth of professional oversight the charade usually goes unnoticed and unopposed.
Data-dredging, cherry picking, confirmatory bias, confirmatory distortion, fabrication, falsification, exaggeration, and a whole host of deceptive tactics are used to work backward from an already determined result.
Any information that contradicts the answer is manipulated, undermined, suppressed or downplayed; even if it is the result of real science and evidence-based research; even if it is the truth. Professional procedure, protocol and ethics are off the table. It is an underhanded free-for-all. Bare knuckle boxing. Trash your opponents work and label it junk-science. Undermine the integrity of your opponents. Use ad hominem attacks to question the opponents motives. Claim the scientists are hacks on the take. Start rumors about them.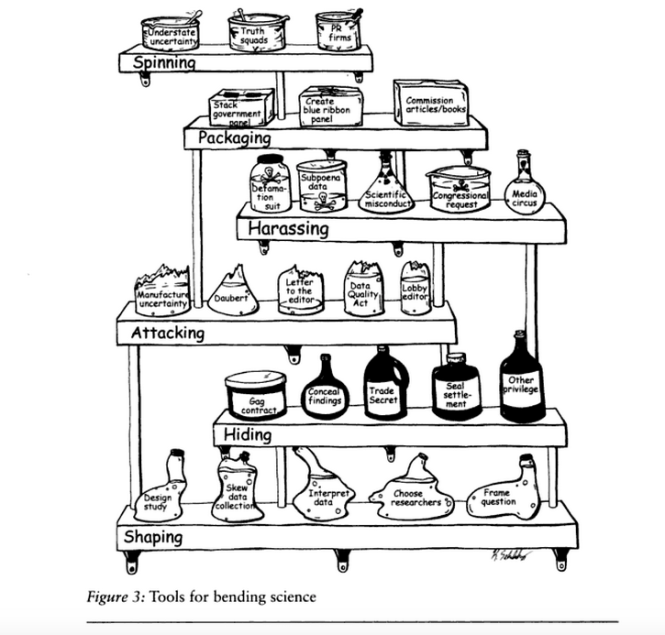 Loudly claim you are the one who is evidence based. Proclaim professionalism and authority. Quibble. Move the goalpost. Nit-pick and split hairs. Proclaim over and over and over again you are the one who is evidence based.
Loudly claim you are the one who is evidence based. Proclaim professionalism and authority. Quibble. Move the goalpost. Nit-pick and split hairs. Proclaim over and over and over again you are the one who is evidence based.
And the problem is it usually works. It is an unfair playing field. When no meaningful barriers are in place to detect cheating and identify cheaters they usually win.
Bending science can have serious and sometimes horrific consequences and multiple examples including the Tobacco and pharmaceutical industry are given in the book.
Calling for immediate action to reduce the role that bent science plays in regulatory and judicial decision making, the authors emphasize the assistance of the scientific community is necessary in designing and implementing reform.
“Shedding even a little light on how advocates bend policy -relevant science could go a long way toward remedying these problems. Indeed, precisely because the advocates have overtaken the law in this area, heightened attention to the social costs of bending science could itself precipitate significant change.”
But there are difficulties in challenging bent science including a general lack of recognition of the problem. With an absence of counter-studies to oppose deliberately manufactured ends-oriented research this would be expected.
Bent science involves the deliberate manufacturing of a pool of information designed to promote a specific agenda. A level playing field would require a pool of opposing research specifically addressing that agenda. In reality this requires both the incentive and the power to do so–an unlikely scenario short of an equally well funded competitor or sufficient public concern about the problem.
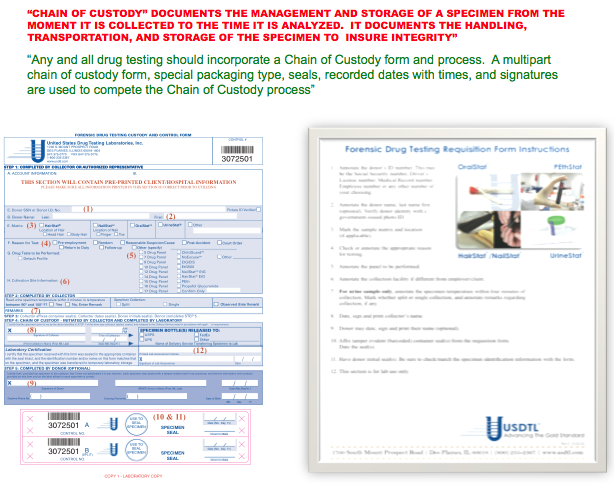
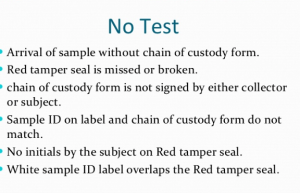
In fact counter-forces are often nonexistent. Investigatory techniques developed and promoted by the FBI crime lab (such as firearms identification and intoxication testing) is one example described in the book. These techniques evolved with little meaningful oversight from the larger scientific community and could be badly bent but there is no meaningful pool of information to disprove them. The authors aptly state that “defendants in most criminal cases lack resources to mount effective challenges, much less undertake their own counter-research.”
And part of the “art” of bending involves swaying public opinion and the mainstream media is typically aligned with the benders so opposing viewpoints seldom make the headlines.
Additionally, there is no meaningful oversight or avenue to pursue accountability. No systems exist to prevent, catch and publicly expose bent-science or those who bend science.
The influence of special interest groups on the practice of medicine is unknown. No one has examined the role of bent science in the rules, regulations, policies and decisions made by those who are in charge of the standards of medical practice and professional behavior of doctors but as a regulated profession governed by the decisions and policies of regulators it is certainly possible.
Regulation of the Medical Profession
Alexis de Toqueville once observed that a key feature of American government was the decentralized character of administration. “Written laws exist in America,” he wrote, “and one sees the daily execution of them; but although everything moves regularly, the mover can nowhere be discovered. The hand which directs the social machine is invisible.”2
Administrative law is the body of law that allows for the creation of public regulatory agencies and contains all of the statutes, judicial decisions and regulations that govern them. Administrative agencies implement their powers in the form of rules, regulations, orders and decisions. State medical boards are the regulatory agencies responsible for the licensure and discipline of physicians. They grant the right to practice medicine in the form of a medical license and each state has Medical Practice Act that governs and defines the practice of medicine. The medical board is empowered to take action against a doctor for substandard care, unprofessional behavior and other violations as defined by the state Medical Practice Act.
Administrative Code governs the licensure and disciplinary process and the State Administrative Procedure Act governs the legal process (due process, discovery, etc.). Regulatory changes are enacted through procedural, interpretive and legislative rules.
Both medical practice acts and administrative procedure acts are subject to change. Changes in medical practice acts can redefine what is acceptable practice and what constitutes professional behavior. This can increase the power and control these agencies have over doctors both professionally and socially.
Changes in Administrative practice acts can decrease what rights a doctor has if this power and control is abused. Changes in the wording of administrative code and administrative practice acts can have profound implications in these rights including due-process, timeliness of being heard, rights to appeal decisions and time-constraints for judicial review.
And when these changes occur they do so silently. The hand that directs the machine is indeed invisible. The consequences, however, are not. These changes not only impact those touched by the hand but can have a systemic impact on the entire profession.
State medical practice acts as well as administrative practice acts and code are susceptible to change and therefore susceptible to the influence of special interest groups benefitting from such change. Regulation of the medical profession is thus susceptible to bent science.
Bent Science and the Medical Profession
The impact of bent science on the regulation of the medical profession has not been studied. As a profession governed by regulatory agencies medicine is certainly not immune to the influence of special interest groups who could in turn influence public policy and regulatory decisions, rules and regulations to benefit their own interests.
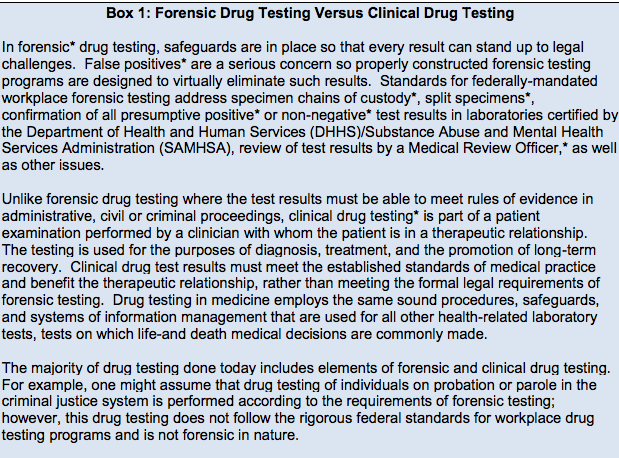
Making sound decisions about regulation calls for an understanding of the problem it is intended to solve. This demands methodologically sound science and evidence-based facts arrived at through rigorous peer review and professional oversight. The science on which policy decisions are made must be reliable and unbiased. Legitimate policy must be based on recognized and legitimate institutions and experts.
If the information regulatory agencies rely on to discipline doctors and protect the public is unreliable then serious consequences can occur.
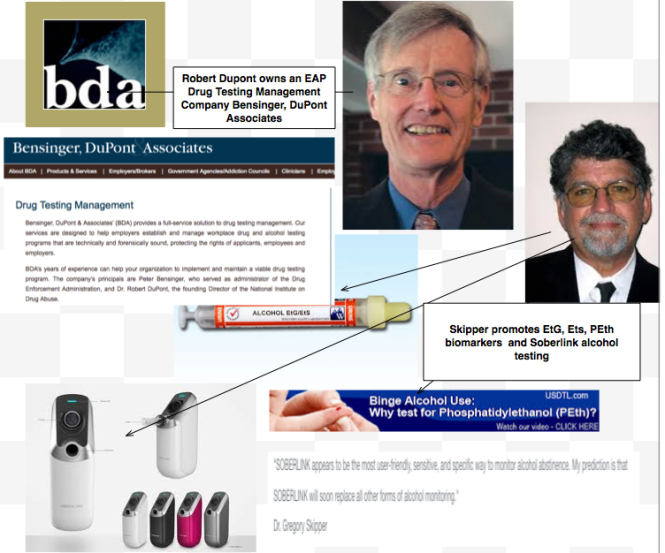
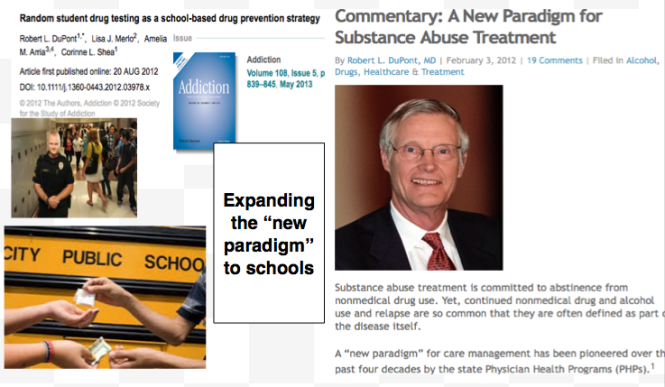
It would be beneficial to look for changes in public policy, guidelines, rules and regulations involving the medical profession and examine the reasons behind them. When did the problem present? Who presented it? Was it based on methodologically sound and accurate data? What organizations do the problem presenters represent? What organizations or individuals aligned or associated with the presenters might benefit? What are the consequences? Who is harmed?
Howard Becker describes the role of “moral entrepreneurs,” who crusade for making and enforcing rules that benefit their own interests by bringing them to the attention of the public and those in positions of power and authority under the guise of righting a society evil.8
The mechanics and mentality is similar to the science benders and, as discussed below, they use some of the same techniques.
Moral entrepreneurs take the lead in labeling a particular behavior deviant and spreading this label throughout society. They associate the behavior of some group with a society evil, affix an easily recognizable label to it and then express the conviction that the evil must be combated. Labeled as being outside the central core values of consensual society, the deviants in the designated group are perceived as posing a threat to both the values of society and society itself.
Activities can rise to the level of ‘social problems” when harm or danger is attributed to those activities and governmental powers are called upon to put an end to those harms. Bent science requires convincing others of a viewpoint and the likelihood of this occurring increases when the activity that is identified as a problem resonates with underlying societal concerns and anxieties. The problem is then endorsed by experts who give legitimacy to such claims.3,4 This legitimacy results attracts media attention which further enforces support from both the public and policy makers.5,6
As a result any bent science directed at regulatory and public policy decision making should be clearly visible.
The sociologist Stanley Cohen used the term ”moral panic” to characterize the amplification of deviance by the media, the public, and agents of social control.7 According to cultural theorist Stuart Hall, the media obtain their information from the primary definers of social reality in authoritative positions and amplify the perceived threat to the existing social order. The authorities then act to eliminate the threat.9 The dominant ideas or ideologies are reproduced by relying on the opinions of the defining authority and then spread through the media.
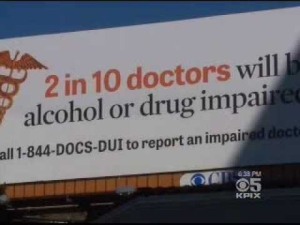
An internet search of what labels have been affixed to doctors in association with a threat to society there are three. A google search of “impaired physician” yields 20, 600 results; “disruptive physician” yields 17, 400 results; and “aging physician” yields 27, 800 results. A large number of these articles, opinion pieces and reviews associate impaired, disruptive and aging physicians with patient death and other adverse events, medical error, and malpractice. The labels affixed to these physicians have been characterized as a major threat to public health and the rhetorical tools used in many of these articles seems aimed at increasing public anxiety.
A PubMed search yields 154 results for the “impaired physician”; 47 results for the “disruptive physician”; and 19 results for the “aging physician.” Many of these are opinion pieces written by the same group of physicians and aimed at hospital administrators, regulators and those involved in the legal or business aspects of medicine.
There is, in fact, no evidence based research that associates the impaired, disruptive or aging physician with any adverse events. The “impaired,” “disruptive” and “aging” physician labels as evinced by a quick google search seem escalated far beyond the level warranted by the existing evidence.
The “impaired” and “disruptive” labels have taken on the status of moral panic and the “aging” label, which is being associated with cognitive impairment, seems to be heading in that direction. The number of articles being published and lectures being given on the dangers of cognitively impaired doctors is increasing. It has not yet reached the level of public awareness the impaired and disruptive have.
To acknowledge that the current level of concern about these labels is exaggerated is not to suggest they do not exist. They do. But the disparity between the evidence-base, or lack thereof, and the level of concern warrants further investigation.
To be clear, doctors who are impaired by drug and alcohol abuse need to be removed from practice to protect the public and receive treatment; doctors who are abusive to others or engage in behavior that threatens patient care need to be held accountable for their actions; and doctors who are cognitively impaired due to dementia need to be removed from practice and evaluated by the proper specialists. If a diagnosis of dementia is confirmed then they need to be removed from practice.
What is the motivation behind the “impaired,” “disruptive” and “aging” physician labels and the multiple articles linking these labels to patient harm and medical error? There is no data driven evidence so where does it come from? Could moral entrepreneurs be behind it? If so then there should be evidence of bent science and to examine this we must look for evidence that these labels have been used to influence regulatory decisions, rules, regulations and policy.
And with the recently archived Journal of Medical Regulation this task can be easily accomplished.
The Journal of Medical Regulation as Timeline and Framework for Policy Evaluation
The Federation of State Medical Boards (FSMB) is a national not-for profit organization that gives guidance to state medical boards through public policy development and recommendations on issues pertinent to medical regulation. Shortly after its founding in 1912, the Federation of State Medical Boards began publishing a quarterly journal addressing issues relating to medical licensing and regulation of doctors. First published in 1913 as the Quarterly of the Federation of State Boards of the United States, the publication has undergone several name changes and publication schedules. From1921 to 1999 it was published monthly as the Federation Bulletin. In 1999 it was changed to the quarterly Journal of Medical Licensure and Discipline and in 2010 was revised to the Journal of Medical Regulation The Journal of Medical Regulation is in the process of archiving all issues dating back to 1913.
Presently every paper dating back to 1967 is available online and the archival organization and availability of full articles published sequentially over the past half-century is historically invaluable. As the official journal of the national organization involved in the medical licensing and regulation of doctors, this archival organization allows for an unskewed and impartial examination in both historical and cultural context. We can identify when particular issues and problems were presented, who presented them and how.
The Journal of Medical Regulation archives provides a structured context to examine these issues in their historical and cultural context. This facilitates a retrospective analysis. As a timeline it allows identification of when the issues were presented. It also allows us to look at the events preceding the problem, who benefited from them, and the consequences. Could these factors be involved in influencing the regulation of medicine and shaping the medical profession? Could bent science have been involved in regulatory and administrative changes that have significantly impacted the rights and well-being of doctors and how the profession of medicine is defined? Could some of the current problems such as the marked increase in physician suicide, sham-peer review, and physician burnout be the result of bent science? If bent science is contributing to bad policy and bad decision making then it need to be exposed and addressed. Bent science is bad medicine and if it exists then we need to urgently shine a light on it.
- McGarity TO, Wagner WE. Bending Science: How Special Interests Corrupt Public Health Research. Cambridge, MA: Harvard University Press; 2008.
- de Toqueville A. Democracy in America. New York: Penguin Books; 1984.
- Blumer H. Social Problems as Collective Behavior. Social Problems. 1971;18:298-306.
- Stone DA. Causal Stories and the formation of policy agendas. Political Science Quarterly. 1989;104:280-300.
- Best J. Threatened Children, Rhetoric and Concern about Child Victims. Chicago University of Chicago Press; 1990.
- Gerbner G, Gross L. The scarey World of TV’s heavy viewer. Psychology Today. 1976;9(89):41-45.
- Cohen S. Folk Devils and Moral Panics: The Creation of the Mods and Rockers (New Edition). Oxford, U.K.: Martin Robertson; 1980.
- Becker H. Outsiders: Studies in the Sociology of Deviance. New York: Free Press; 1963.
- Hall SC, Critcher C, Jefferson T, Clark J, Roberts B. Policing the Crisis: Mugging, the State, and Law and Order. London: Macmillan; 1978.









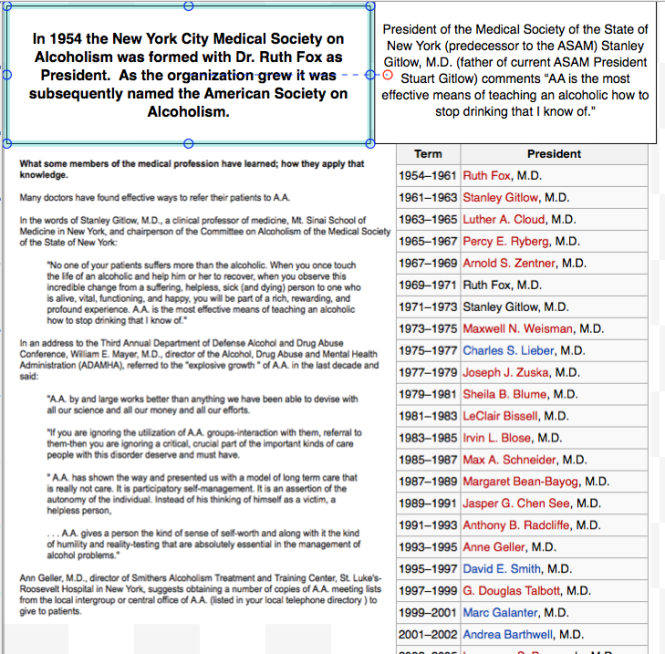

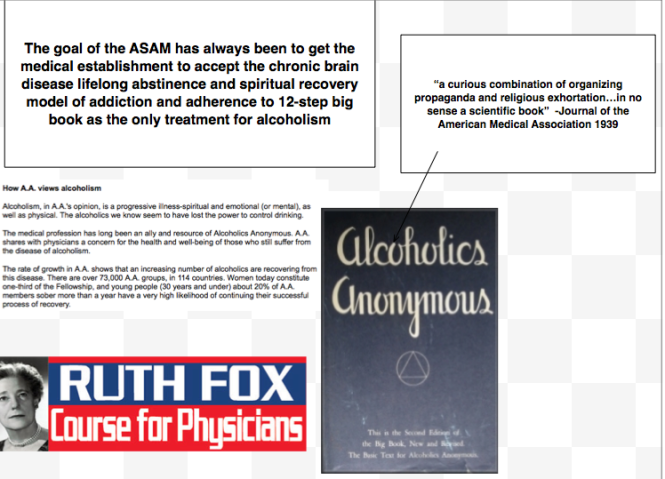













 In order to understand the current incarnation of
In order to understand the current incarnation of 