
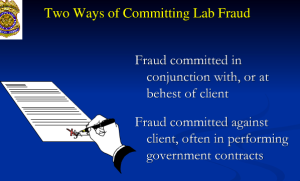
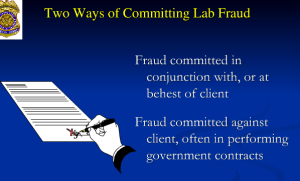
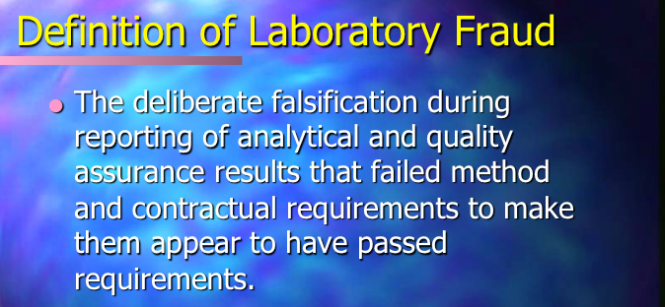
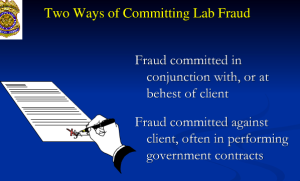
The attached documents show the MA PHP (PHS, inc) and USDTL engaging in flagrant forensic fraud. They are caught red handed. Moreover, the VP of operations at USDTL laboratories Joseph Jones, is involved.
This is not Annie Dookhan lone nut falsification of drug tests but misconduct indicative of top-down systemic corruption. It appears to be standard operating procedure.

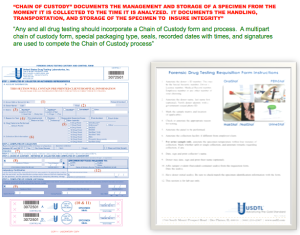
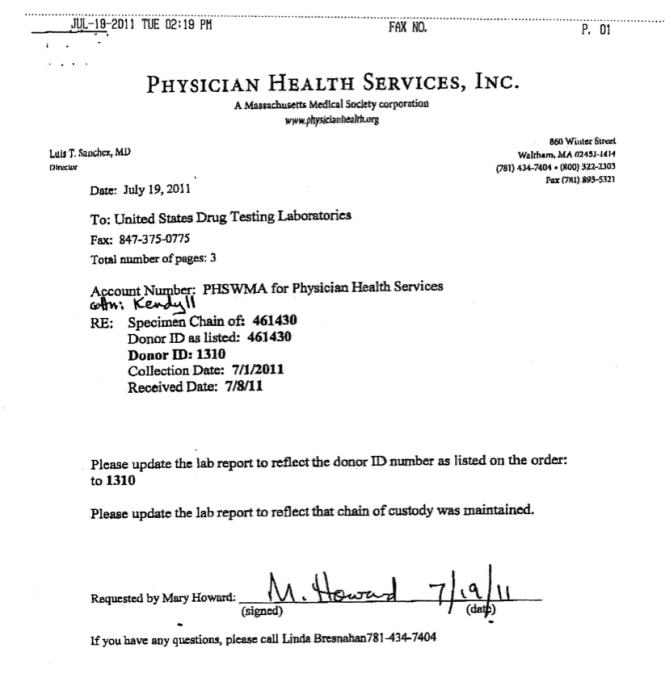
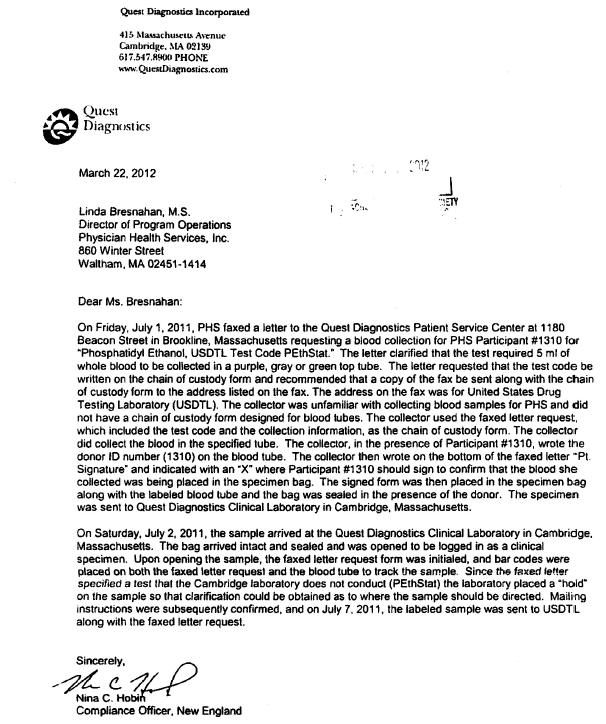
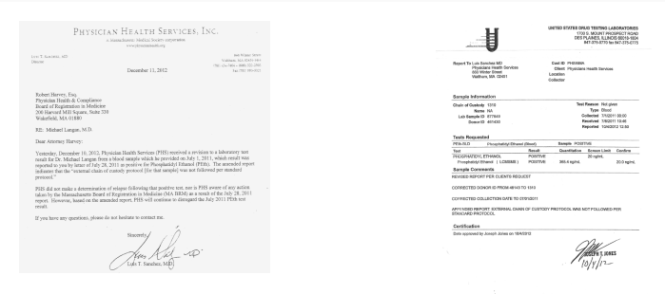
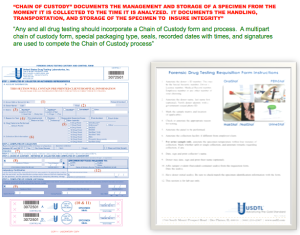
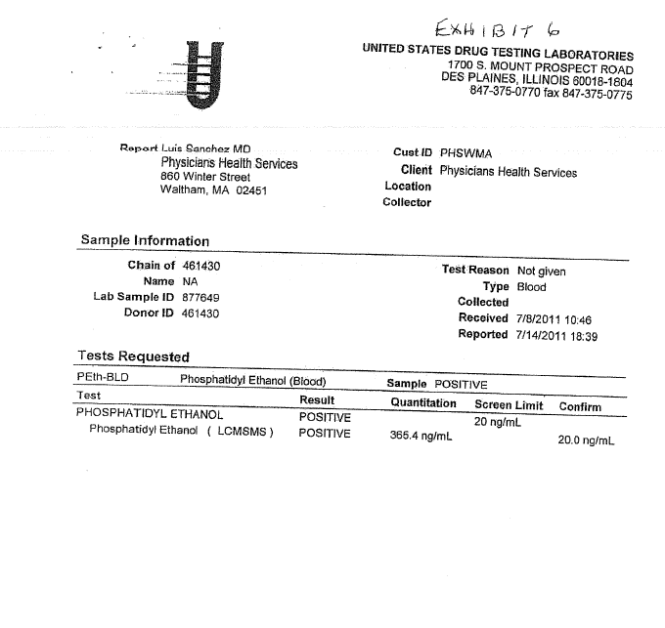
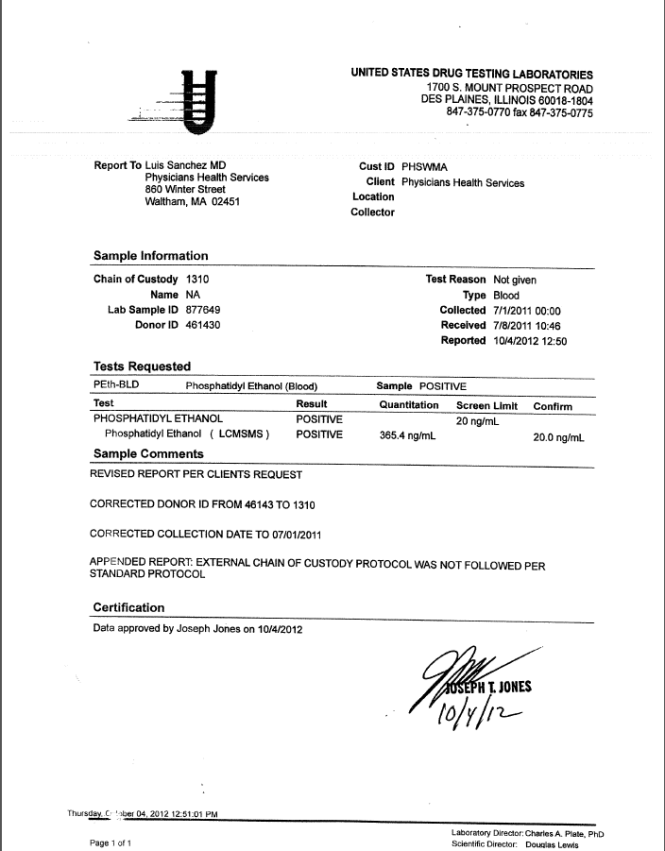
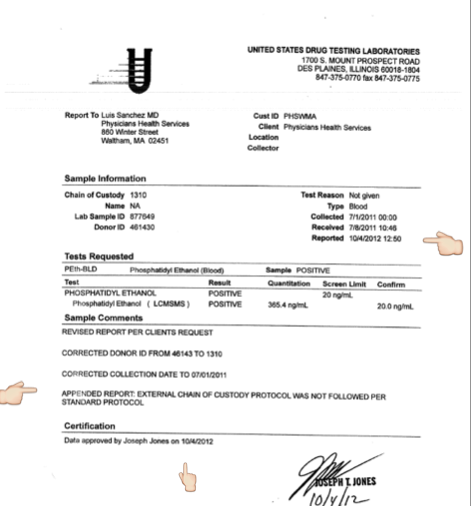
The documents are part of the “litigation packet” for a PEth test that was drawn July 1, 2011 and reported as a positive on July 19, 2011. A litigation packet is al legal document generated with any forensic test to document chain of custody.
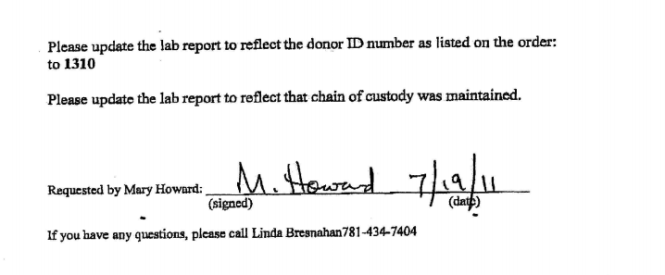
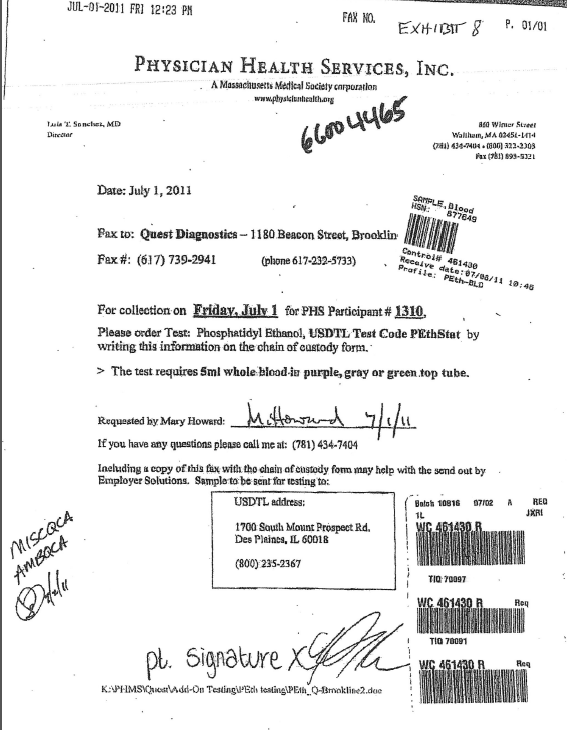
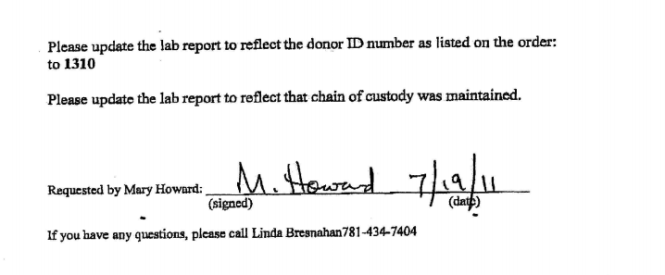
It includes a faxed memo from PHS to USDTL 7/19/2011 requesting an identifying ID# and a “chain of custody” be added to an already positive test. Seldom is a document available that shows how the perpetrators of laboratory fraud do it–this is complete from start to finish.
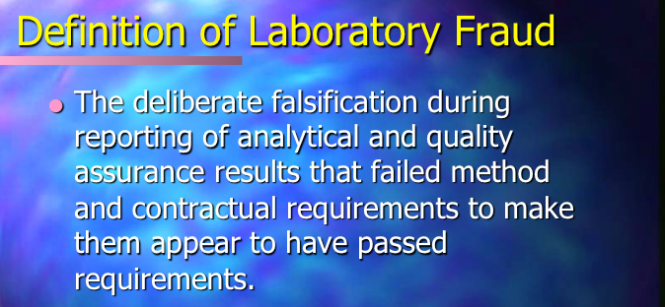
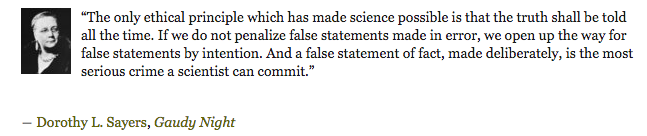
A chain of custody is generated in real time. It cannot be done retroactively.
To do so constitutes fraud.
With no compunction, concern, or consternation this sociopathic mercenary subordinates science in to put coins in his purse and complies with this improper request and adds a unique ID number to an already positive specimen.
Moreover, when the test was questioned the, PHP requested that USDTL support the test as a valid positive. And Joseph Jones did so with full knowledge there was no chain-of-custody and the ID # and date of collection were added.
This is flagrantly antithetical to the process of MRO review (required of all forensic tests before they are reported as positive).
Like an arsonist firefighter, Jones does the exact opposite of what he is supposed to. With complete disregard of the basic codes of conduct and MRO guidelines he reports as positive a test that would not meet the minimum requirements for clinical test let alone forensic.
A test with multiple fatal flaws and no chain of custody, collection date, or unique identifier was reported as a positive to please a client and it is egregious, indefensible, and illegal.
Positive drug and alcohol tests can end lifetime careers, tear apart families, and trigger suicides. And I am hearing of more and more suicides caused by these laboratory tests done by Dr. Jones and corrupt illegitimate authority like Dr. Sanchez.
The consequences are grave and far reaching. An organizational culture capable of willing participation and continued support of forensic fraud cannot be trusted.
Cognizant that the consequences to the donor are significant and possibly irreversible and catastrophic exhibits a careless disregard for truth that is unconscionable. That this was done without hesitation or thought is egregious.
It is purposeful and with undeniable malice. It represents institutional and sinister corruption. And it exemplifies the top-down sociopathic, predatory, and uncaring organizational culture that is undermining democracy and eroding civil liberties.
But the most disturbing fact of this is that those who should do something about it blind themselves.
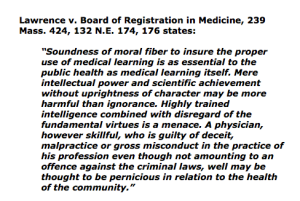
The Board of Registration in Medicine protects Dr. Sanchez. He is apparently allowed to commit any crimes he wants and it is worth reading through all of the documentation as he compounds felonies over time.
The political abuse of psychiatry and false diagnoses are acts that violate the most basic and fundamental medical and social ethical codes. They should be met with zero tolerance by the medical community as well as society at large.
Remarkably the Massachusetts Department of Health and Human Services is also aware of this. Apparently learning nothing from the Annie Dookhan case, certain individuals have hemmed and hawed for over six months without any response in a torpid stasis. As protectors of the public health one would think there would be some urgency to address the fact that a state contracted agency is engaging in undeniable laboratory misconduct and fraud.
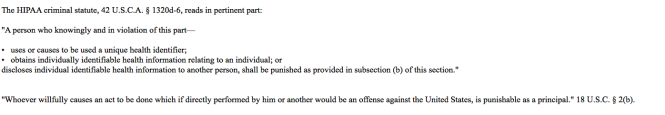
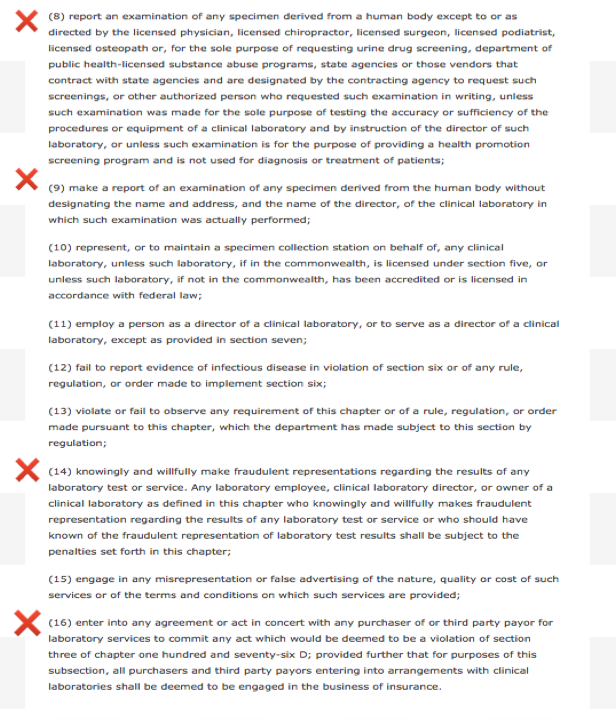
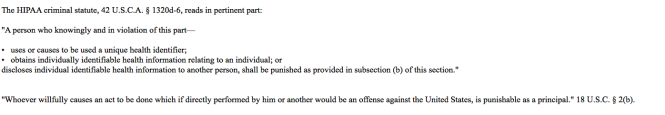
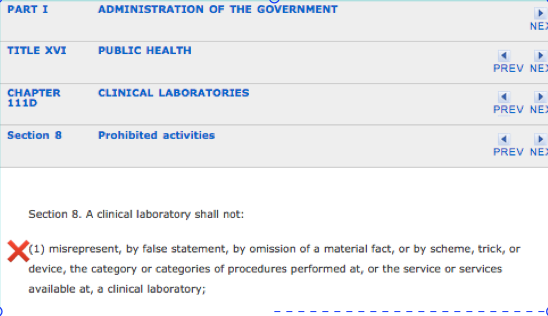
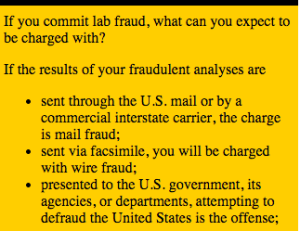
The crimes are many and include state and federal crimes as well as violation of the HIPAA criminal statute as they changed a “forensic” sample to “clinical” in order to bypass chain of custody. They then changed it back to “forensic” and misrepresented it as such up until recently.
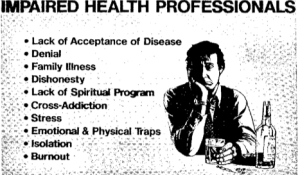
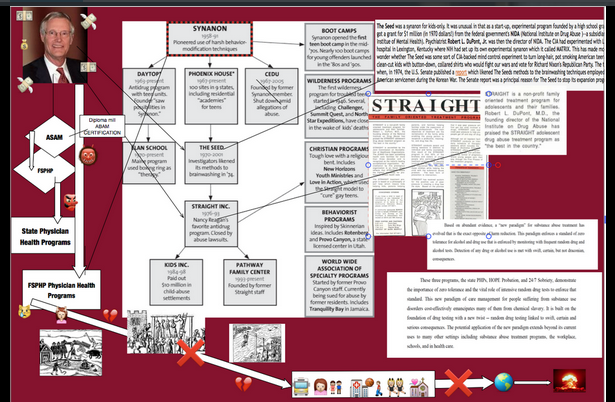
This needs to get be addressed outside the medical profession. As a society and culture within a society and culture the prevalence of thinking has become destructive rather than ameliorative under the influence of the “impaired physicians movement.” The ease with which pernicious ideas and attitudes have pervaded the regulatory and organizational and regulatory culture of medicine is frightening.
The fact that medical boards and public health department are aware of criminal acts being committed by this “authority” yet do nothing to address its existence will inevitably lead to worse .
If dictatorships can be defined as systems in which there is a prevalence of thinking in destructive rather than ameliorative terms then the “physician wellness” paradigm” shoe fits. There are multiple warning signs that the profession of medicine is becoming subordinated to the guiding philosophy of the “physician wellness” movement,
One thing is for certain. There should be zero-tolerance for forensic fraud perpetrated by those in positions of power. Any intentional laboratory fraud guided by malice is egregious but the scope and severity of what was done here involving collusion to fabricate evidence to coverup the crime, and concealment of the truth when the lab was forced to correct the test by an outside agency is particularly egregious. The fact that Dr. Luis Sanchez hid the fact that he was made aware of the corrected test on October 4, 2012 and reported non-compliance with requirements that directly resulted from that very test for “damage control” under “color of law” is unconscionable. But the fact that he did these things and lied about it is undeniable. The facts are self-evident.
This is much worse than Annie Dookhan as her victims were abstractions. She did not see the damage that resulted from her laboratory misconduct. These people knew what they were doing, knew it was wrong and did it anyway. And unlike Annie Dookhan, Sanchez saw the damage he was causing as that was his intent.
As far as I can find, these documents are the most elaborate and complete representation of the mechanics of forensic fraud. They show the sequential steps between the party requesting it and the response of the complicit lab. The documents illustrate how easy laboratory misconduct is accomplished and the moral detachment of the involved parties. The fact that it involves top-down corruption cannot be overestimated.
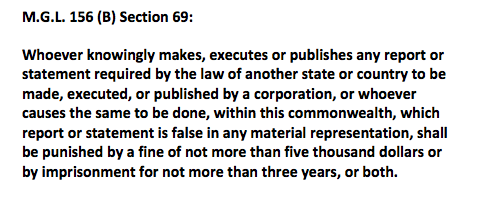
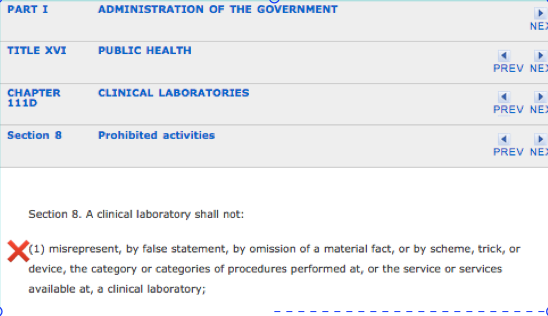
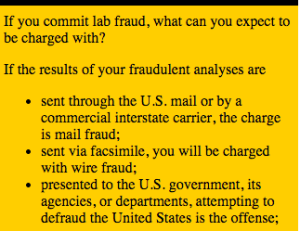
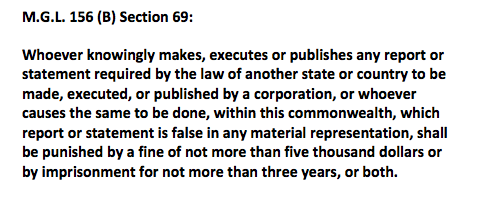
The most obvious crime is the violation of M.G.L 156 (B) section 69 involving reporting false statements.

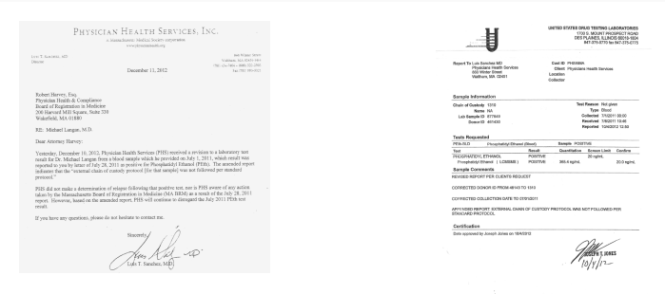
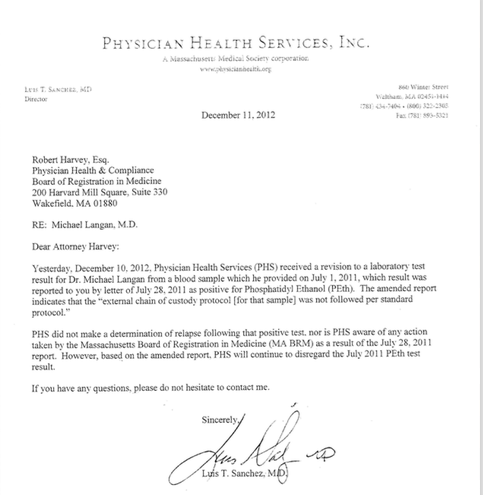
December 11, 2012 Sanchez writes to Board of Registration in Medicine that he “just found out” about test the day before. USDTL report to Dr. Sanchez October 4, 2012 reporting the corrected test. Sanchez concealed this and the next week took action against my license by reporting “noncompliance” for damage control. Documentary evidence undeniable.
The fact that this was test was ordered as a “forensic” specimen then changed to a “clinical” specimen makes it a HIPPA violation as changing it to “clinical” created “protected health information” (PHI). In fact, the only reason I was able to obtain the October 4, 2012 document proving Dr. Sanchez lied was due to a change in the HIPPA-Privacy Rule enabling “patients’ to obtain laboratory results without authorization from the agency that ordered it. Without this allowance Sanchez would still be maintaining he did not find out about the correction until December. Well the documentary proof shows he lied.
Moreover, PHS is not a treatment provider and cannot order clinical specimens. It is an ultra vires act outside of their designated scope of authority as a non-profit organization.
What Sanchez did here is also in violation of the HIPAA criminal statute.

The elements of a criminal offense under HIPAA are fairly straightforward. To commit a “criminal offense” under HIPAA, a person must knowingly and in violation of the HIPAA rules do one (or more) of the following three things.: use or cause to be used a unique health identifier, obtain individually identifiable health information relating to an individual or disclose individually identifiable health information to another person. Criminal penalties under HIPAA, tiered in accordance with the seriousness of the offense, range from a fine of up to $50,000 and/or imprisonment up to a year for a simple violation to a fine up to $100,000 and/or imprisonment up to five years for an offense committed under a false pretense and a fine up to $250000 and/or imprisonment up to ten years for an offense committed with intent to sell, transfer, or use individually identifiable health information for commercial advantage , personal gain, or malicious harm.
Requesting the sample be changed to “clinical” created PHI and the fact that it was under false pretense and intended to cause malicious harm is quite evident.
Although PHS is not a covered entity Quest Diagnostics is and as a business associate they can be linked by the conspiracy statute:

And that is why outside forces need to be involved. These are serious crimes and they have created serious consequences. I have heard of multiple suicides in doctors caused by these tests. How many doctors have died as a result of Jones colluding with individuals just like Sanchez? The results of these tests can have grave, far reaching and even permanent consequences. They can ruin careers and destroy families. Sanchez and Jones know this. Their moral disengagement here shows an absence of empathy and complete disregard of what consequences may result.
The Board of Registration in Medicine is protecting Dr. Sanchez and the DPH has its head in the sand.
It is my understanding that groups like PHS have led law enforcement to believe that all matters involving doctors should be handled by the medical community. This has created barriers as doctors reporting crimes have found it difficult to get them investigated or even reported let alone charged.
Law enforcement needs to address this. This needs to be exposed.
.I have been told that in other states where similar situations exist in which the truth is unable to penetrate the proper channels it should go directly to the Governor.
I would like to get these documents to Governor Charlie Baker and any help in making this happen would be appreciated.





“A body of men holding themselves accountable to nobody ought not to be trusted by anybody.”
― Thomas Paine
USDTL drug testing laboratory claims to advance the”Gold Standard in Forensic Toxicology.” “Integrity: Results that you can trust, based on solid science” is listed as a corporate value. “Unlike other laboratories, our drug and alcohol testing begins and ends with strict chain of custody.” “When people’s lives are on the line, we don’t skip steps.” Joseph Jones, Vice President of Laboratory Operations explains the importance of chain-of-custody in this USDLT video presentation.
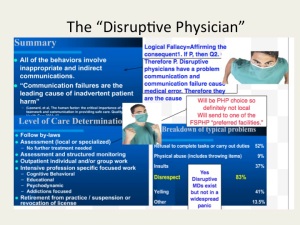
Dr. Luis Sanchez, M.D. recently published an article entitled Disruptive Behaviors Among Physicians in the Journal of the American Medical Association discussing the importance of of a “medical culture of safety” with “clear expectations and standards.” Stressing the importance of values and codes-of-conduct in the practice of medicine, he calls on physician leaders “commit to professional behavior.”
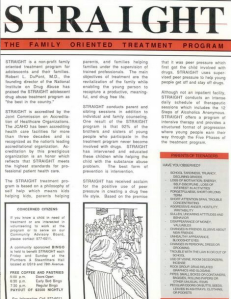
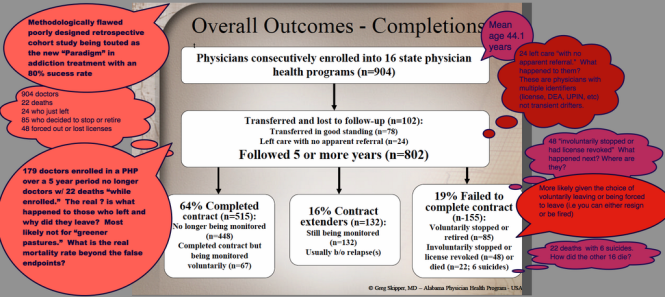
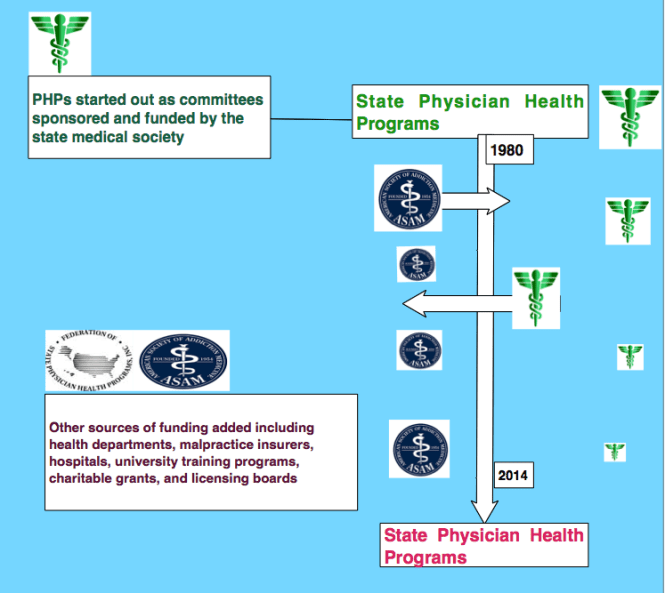
Sanchez is Past President of the Federation of State Physician Health Programs (FSPHP). According to their website the FSPHP “serves as an educational resource about physician impairment, provides advocacy for physicians and their health issues at local, state, and national levels, and assists state programs in their quest to protect the public.” In addition the FSPHP “helps to establish monitoring standards.” The FSPHP is the umbrella organization of the individual State PHPs.
Sanchez is also the previous Medical Director of the Massachusetts state PHP, Physician Health Services, Inc. (PHS). According to their website PHS is a “nonprofit corporation that was founded by the Massachusetts Medical Society to address issues of physician health. PHS is designed to help identify, refer to treatment, guide, and monitor the recovery of physicians and medical students with substance use disorders, behavioral health concerns, or mental or physical illness.”
PHPs recommend referral of physicians if there are any concerns such as getting behind on medical records. As PHS Associate DirectorJudith Eaton explains “when something so necessary is not getting done, it is prudent to explore what else might be going on.” If the PHP feels that doctor needs an assessment they will send that doctor to a “PHP-approved” facility “experienced in the assessment and treatment of health care professionals.” The physician must comply with any and all recommendations of the assessment center. To assure this the physician must sign a monitoring contract with the PHP (usually five years). USDTL is one of the labs PHPs have contracted with for forensic drug and alcohol testing.
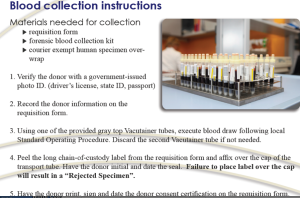
Forensic Drug and Alcohol Tests: The Need For Integrity and Accountability of the Sample
“Forensic” drug-testing differs from “clinical” drug-testing in how the results are used. “Clinical” tests are used for medical purposes in diagnosing and treating a patient.
A “forensic” test is used for non-medical purposes. It is not used for patient care, but for detecting licit and illicit substances in those who should not be using them. Pre-employment and employee assistance and professional monitoring programs are examples.
Forensic testing is held to a higher standards because the consequences of a positive result can be grave and far reaching. A positive forensic test can result in loss of rights of the individual being tested and his or her loved ones. Mistakes are unacceptable.
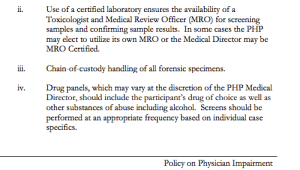
The Federation of State Medical Boards Policy on Physician Impairment supports this position stating “chain-of-custody forensic testing is critical” (page 14) and the “use of a Medical Review Officer (MRO) for screening samples and confirming sample results” (page 21).
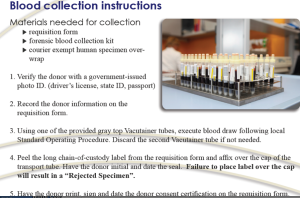
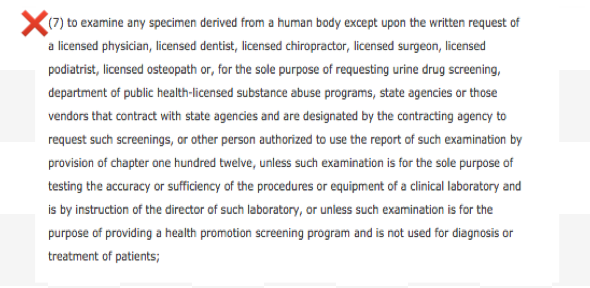
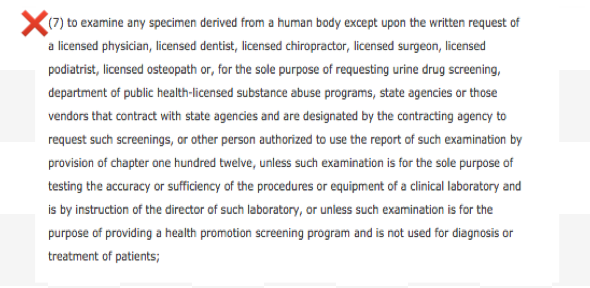
Any and all drug testing requires chain-of-custody. The custody-and-control form is given the status of a legal document because it has the ability to invalidate a test that lacks complete information. Chain-of-custody provides assures specimen integrity. It provides accountability.
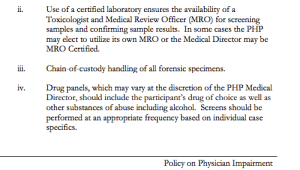 The job of the MRO is to ensure that the drug testing process is followed to the letter and reviews the Custody and Control form for accuracy. The MRO also rules out any other possible explanations for a positive test (such as legitimately prescribed medications). Only then is the test reported as positive.
The job of the MRO is to ensure that the drug testing process is followed to the letter and reviews the Custody and Control form for accuracy. The MRO also rules out any other possible explanations for a positive test (such as legitimately prescribed medications). Only then is the test reported as positive.
The legal issues involved in forensic testing mandate MRO review. According to The Medical Review Officer Manual for Federal Workplace Drug Testing Programs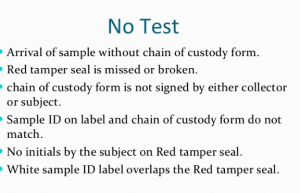
“the sole responsibility of the MRO is to”ensure that his or her involvement in the review and interpretation of results is consistent with the regulations and will be forensically and scientifically supportable.”
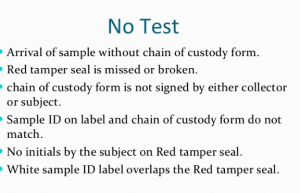
“Fatal flaws” such as lack of chain-of-custody form, missing tamper proof seal, missing signatures, or a mismatch of the sample ID and chain of custody ID invalidate the test. It is not reported. Tight chain-of-custody and MRO review is critical for the accountability and integrity of the sample.
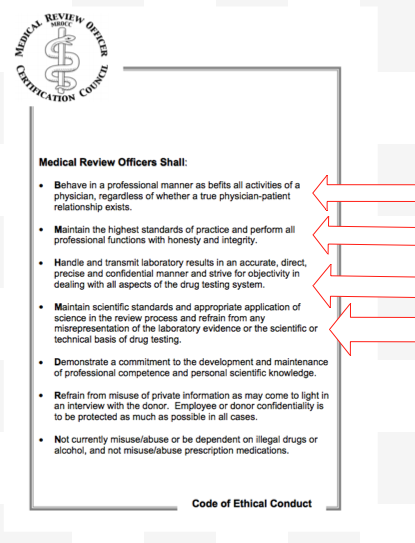
The Medical Review Officer Certification Council provides a certification process for MROs. They  also follow their own Code of Ethics. In accordance with these standards PHS has an MRO to review all positive tests. As added assurance the FSPHP guidelines state that all positive tests must be approved by the Medical Director.
also follow their own Code of Ethics. In accordance with these standards PHS has an MRO to review all positive tests. As added assurance the FSPHP guidelines state that all positive tests must be approved by the Medical Director.
Regulation and the Medical Profession–The need for Integrity and Accountability in Physician Leadership and Health Care Policy.
Good leadership requires correct moral and ethical behavior of both the individual and the organization. . Integrity is necessary for establishing relationships of trust. It requires a true heart and an honest soul. People of integrity instinctively do the “right thing” in any and all circumstances. The majority of doctors belong to this group.
Adherence to ethical codes of the profession is a universal obligation. It excludes all exceptions. Without ethical integrity, falsity will flourish.
The documents below show fraud. It is intentional. All parties involved knew what they were doing, knew it was wrong but did it anyway. The schism between pious rhetoric and reality is wide.
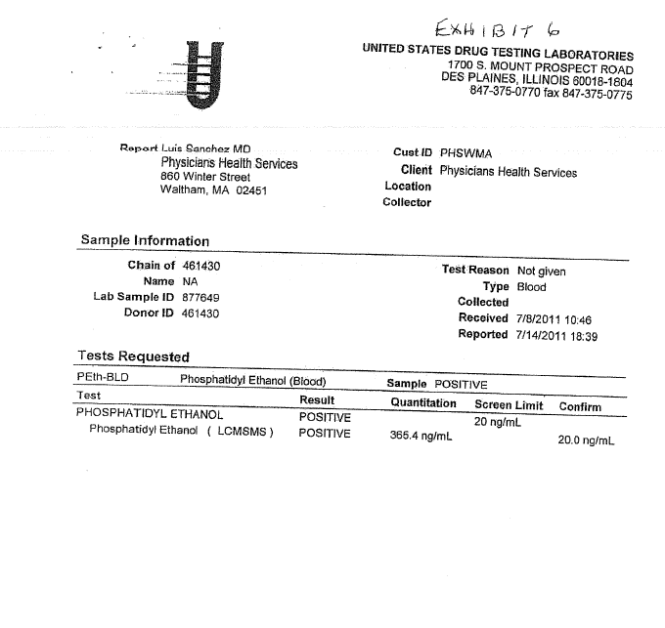
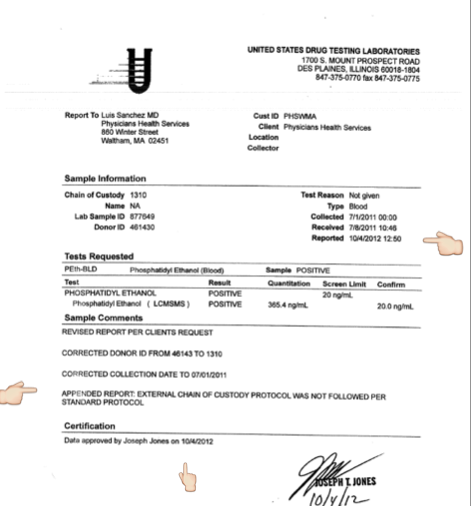
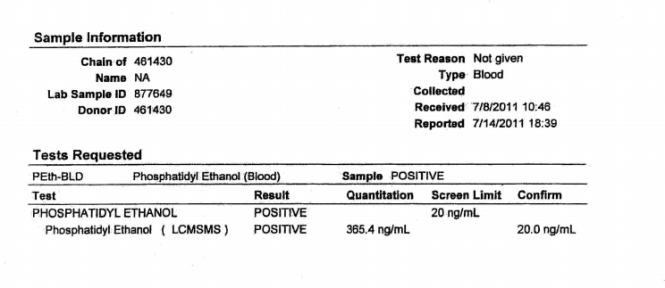
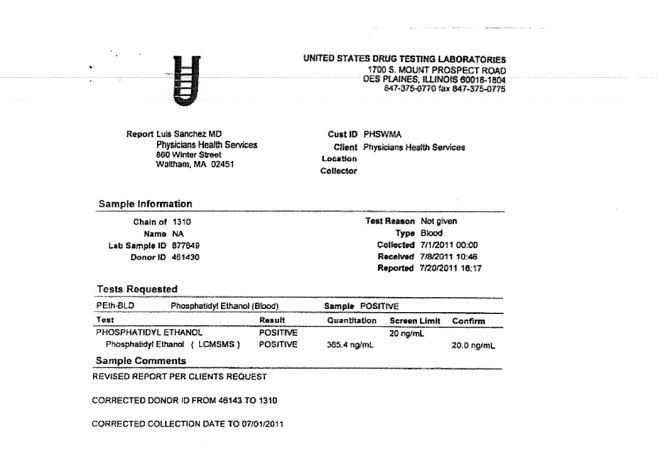
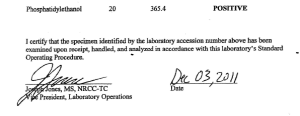
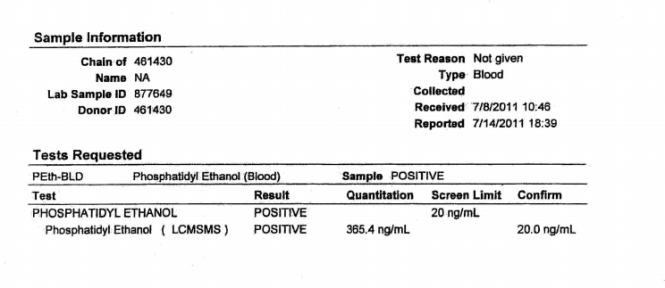
Positive Phosphatidyl Ethanol test at level of 365.4 (cutoff =20) No date of collection. place of collection or name of collector. Donor ID # = 461430 My Unique Identifier #1310 is nowhere on this document.
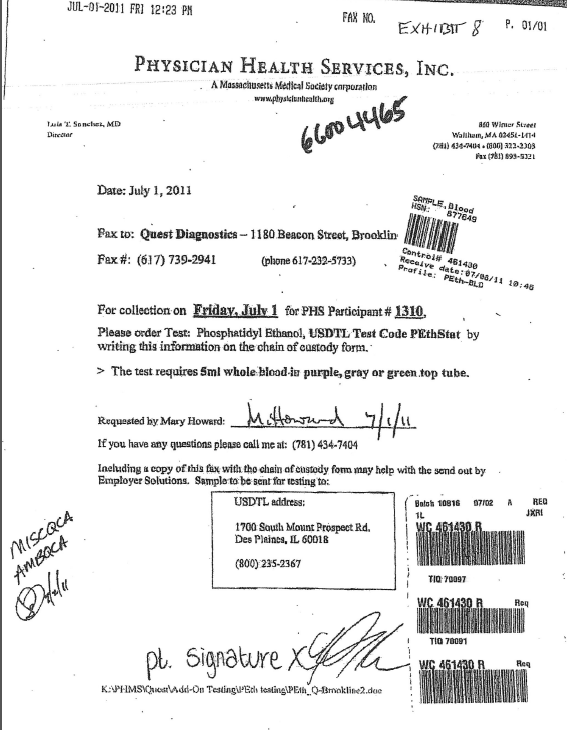
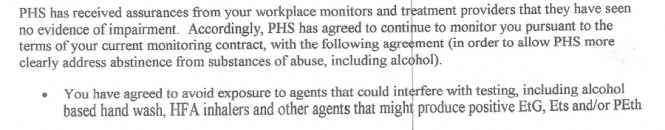
The July 19th, 2011 fax from PHS seen below is in reference to the lab report from USDTL seen above. In it PHS requests the report be “updated”to donor ID number “1310” and to “reflect that the chain of custody was maintained.”
The lab report is a positive test for the alcohol biomarker (Phosphatidyl Ethanol) or PEth, an alcohol biomarker introduced by the Federation of State Physician Health programs and marketed by USDTL and other labs to detect covert alcohol use..
There is no record of where, when or by whom it was collected.
 Both the donor ID # and chain of custody are listed as 461430.
Both the donor ID # and chain of custody are listed as 461430.
The purpose of chain-of-custody is to document the location of a specimen in real time. “Updating” it is not an option. It is prohibited. Updating the “chain of custody to reflect that chain of custody was maintained” is a clear indicator that it was not maintained.
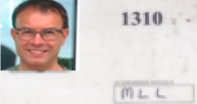
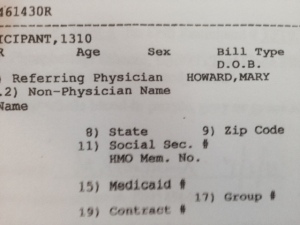
ID #1310 is the unique identifier I was issued by PHS. It is used as a unique identifier, just like a name or social security number, to link me to any sample collected for random drug and alcohol screening. #1310 identifies me as me in the chain-of-custody. On July 1st, 2011 I had a blood test collected at Quest Diagnostics.
The sample was collected at Quest Diagnostics on July 1, 2011 but these documents were not obtained until December 3, 2011 and were included in the “litigation packet” which documents chain-of-custody and is generated on any and all forensic drug testing. It provides proof that the test was done on who it was supposed to have been done and that all required procedure and protocol was followed. It protects the donor form being falsely accused of illicit substance use. In most employee drug-testing programs the litigation-packet is provided on request immediately. It is a transparent process. This is not the case, however, at PHS.
I requested the litigation packet immediately after the positive test was reported on July 19, 2011. PHS first refused, then tried to dissuade me. They finally agreed but warned there would be “unintended consequences. The entire litigation packet can be seen here: Litigation Packet 12:3:2011
The positive sample has no chain-of-custody linked to me, no date, and no indication where it was collected or who collected it. In addition there was no “external” chain of custody for the sample. The custody-and-control form was missing.
With multiple fatal flaws (6/6) rendering it invalid, USDTL should have rejected it by their own written protocol.
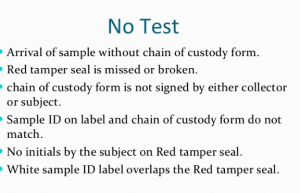
6/6 Fatal Flaws–Just one invalidates the Test
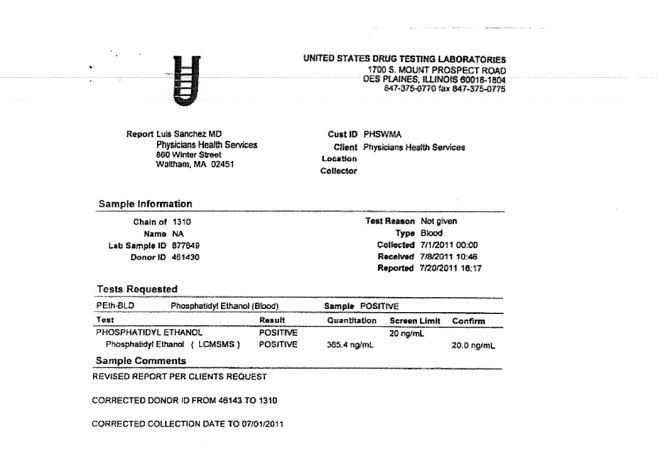
USDTL did not reject it. The document below shows that USDTL added my ID # 1310 and added a collection date of July 1, 2011–the day I submitted the sample.
“REVISED REPORT PER CLIENTS REQUEST”
And in doing so the lab that claims “integrity” and “strict chain of custody” readily, and with no apparent compunction” manufactured a chain-of-custody and added a unique identifier by faxed request.
The litigation packet was signed by Joseph Jones on December 3, 2011. There was no record of where the sample was from July 1st to July 8, 2011. No external chain-of-custody or custody-and-control form was evident in the litigation packet.
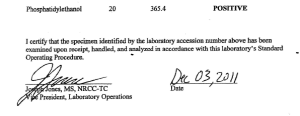
The V.P. for Laboratory operations for the lab that claims “strict chain of custody” and that “doesn’t skip steps” “when “peoples lives are on the line” verified a positive test as positive with no custody and control form, no external chain of custody and 6/6 fatal flaws. What is so shocking is that this was done without compunction or pause. As a forensic test ordered by a monitoring program Jones knew full well it would result in significant consequences for someone. He knew that someones “life was on the line,” knew it was wrong, and did it anyway.
A person of conscience would never do this. It is unethical decision making that goes against professional and societal norms. A “moral disengagement” that represents a lack of empathy and a callous disregard for others. I would not consider doing something like this for any price and here it appears to be standard operating procedure.
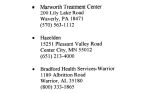
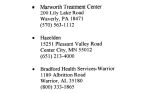
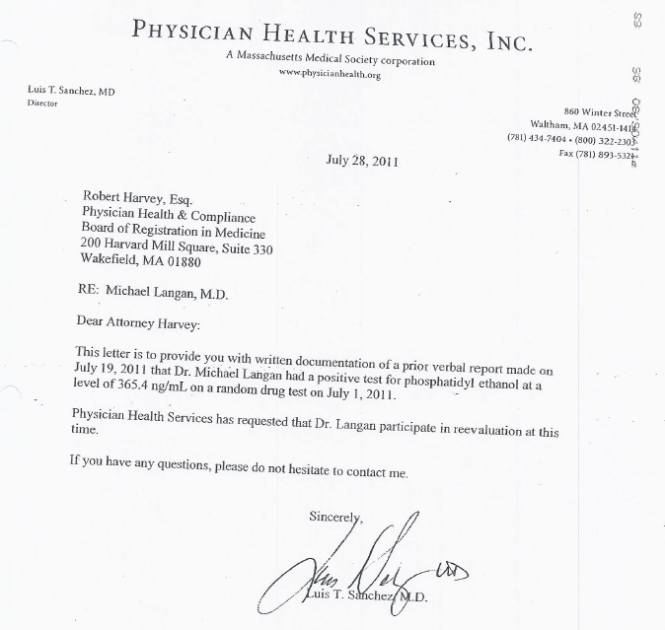
PHS reported the positive test to the Medical Board on July 19, 2011 Positive PEth July 19, 2011-1. It was used as a stepping-stone to request an evaluation at one of three “PHP-approved” facilities (Marworth, Hazelden and Bradford). The Medical Directors of all three facilities can be seen on this list list called “Like-Minded Docs.” The MRO for PHS, Dr.Wayne Gavryck, whose job was to review the chain-of-custody and validate its integrity before reporting it as positive is also on the list. See this simplified schematic of how it works in Massachusetts. It shows how this is a rigged game.
Expecting to be diagnosed with a non-existent problem and admitted for non-needed treatment I requested an evaluation at a non-12 step facility with no conflicts-of-interest. Both PHS and the Medical Board refused this request in one of four violations of the Establishment Clause of the 1st amendment.
I chose Hazelden. The Medical Director was aware that I had just signed a patent license agreement for an epinephrine auto-injector and he had a child with a peanut allergy. We talked about the device and discussed the problems with current management. I think it was because of this added personal interaction that he did not “tailor my diagnosis” as PHS most certainly requested. Seeing me as a person rather than an object, I believe, enabled his conscience to reject it. My discharge diagnosis found no history of alcohol issues but they could not explain the positive test. Unable to rule out that I drank in violation of my PHS contract they recommended I attend AA.
PHS mandated that I attend 3 12-step meetings per week and requested that I obtain names and phone numbers of fellow attendees so they could contact them to verify my attendance. They also mandated that I discontinue my asthma inhalers (as the propellant contains small amounts of ethanol) that had been controlling my asthma and preventing serious attacks for the previous ten years. I was threatened that if I had to use the inhalers or one day late on the increased payments I would be reported to the Board and lose my license.
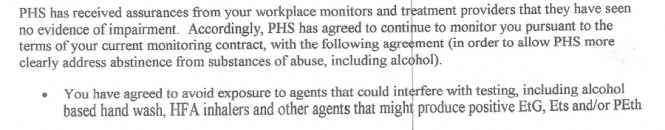
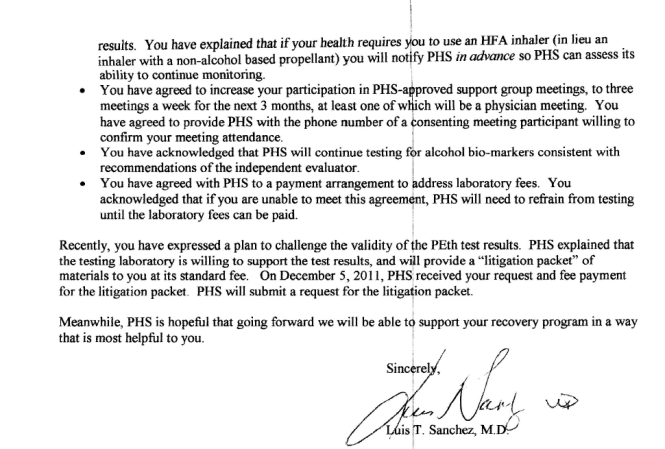
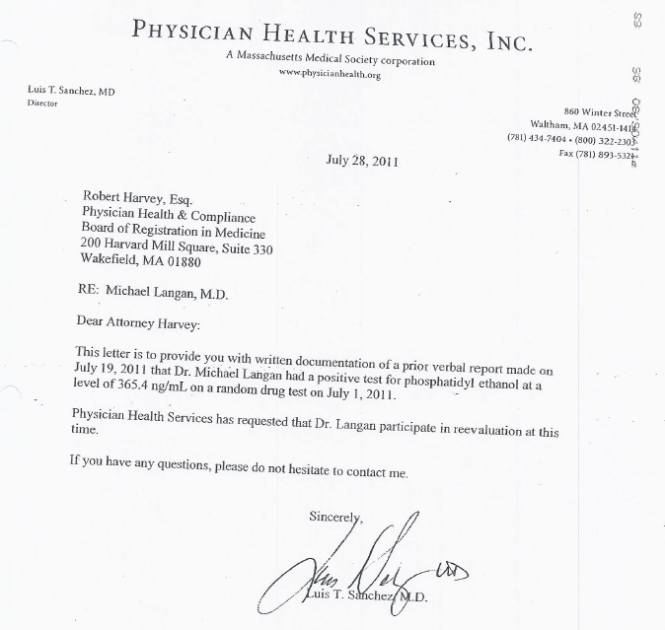
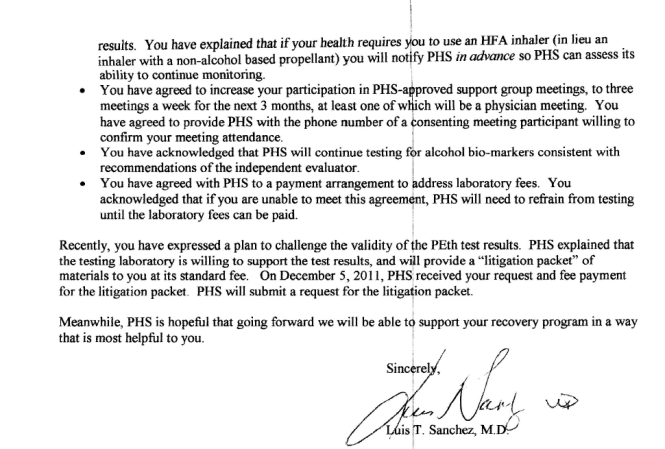
Sanchez states that my request for the “litigation packet” was processed on December 5, 2011 (two days after Jones signed off on it) and adds the “testing laboratory is willing to support the test results.”
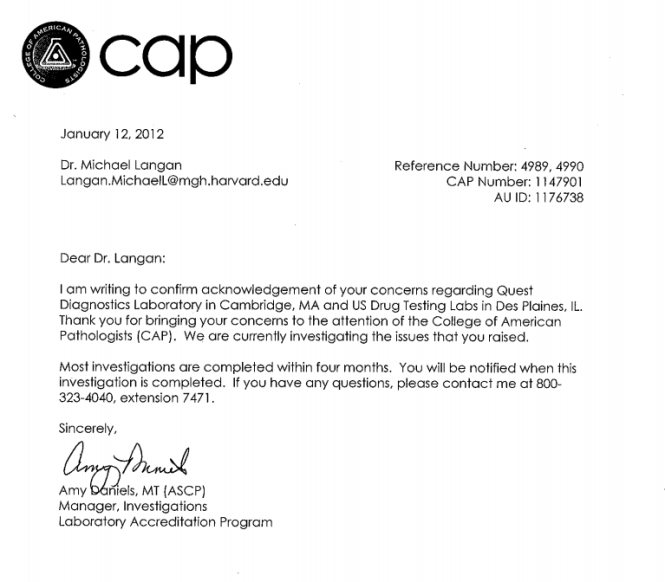
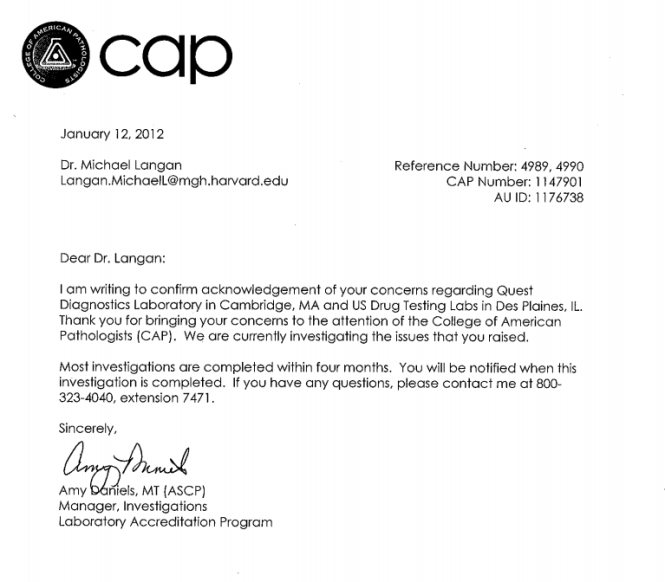
In the interim I filed a complaint with the College of American Pathologists. I also requested the missing external chain of custody documents from Quest.
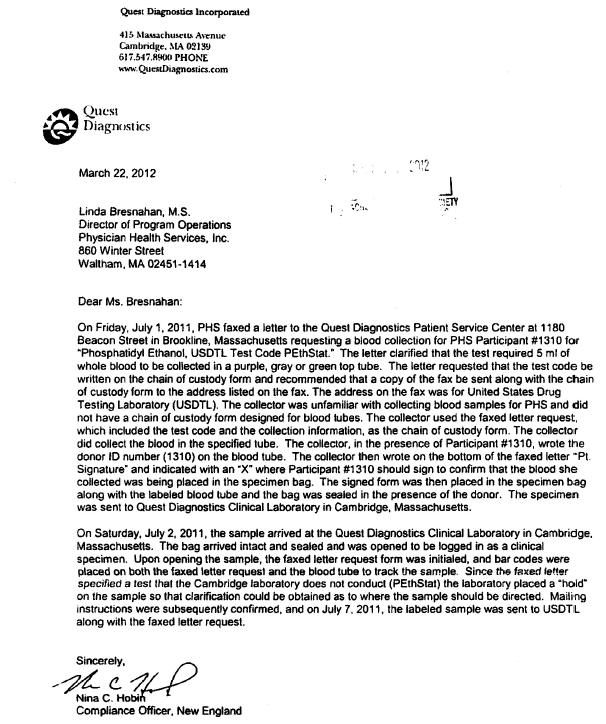
I never received the chain of custody from Quest. Instead I received a letter from Nina Tobin, Compliance Manager for Quest documenting all the errors but written to sound as if some sort of protocol was maintained. Tobin claimed the specimen was inadvertently logged as a clinical specimen but sent on to USDTL a week later. (See Quest Letter )
The Chief of Toxicology at MGH wrote a letter to the Board documenting all of the misconduct and irregularities stating that it was an “intentional act” perpetrated by PHS. MLLv3finalJacob_Hafter_Esq_copy.
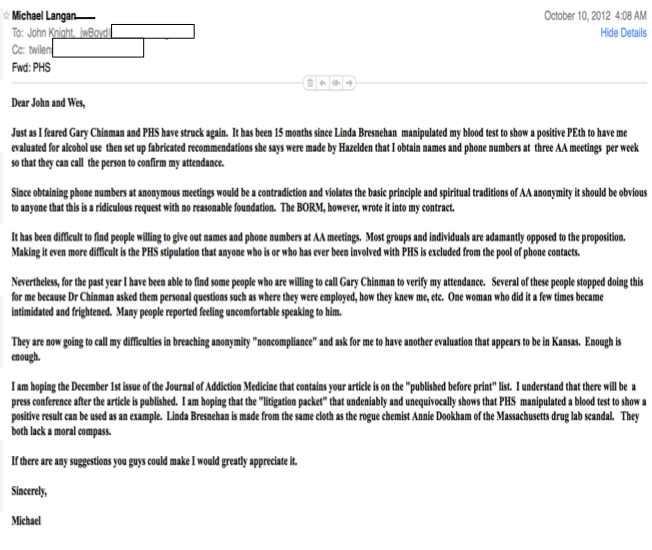
This letter, as well as the opinions of everyone outside of PHS was ignored. So too were any opinions of my two former Associate Directors at PHS. The e-mail below dated October 10th, 2011 is to to Drs. John Knight and J. Wesley Boyd and I am referring to their article Ethical and Managerial Considerations Regarding State Physician Health Programs that was about to be published. We had hoped that it would draw more attention to the problems with PHPs.
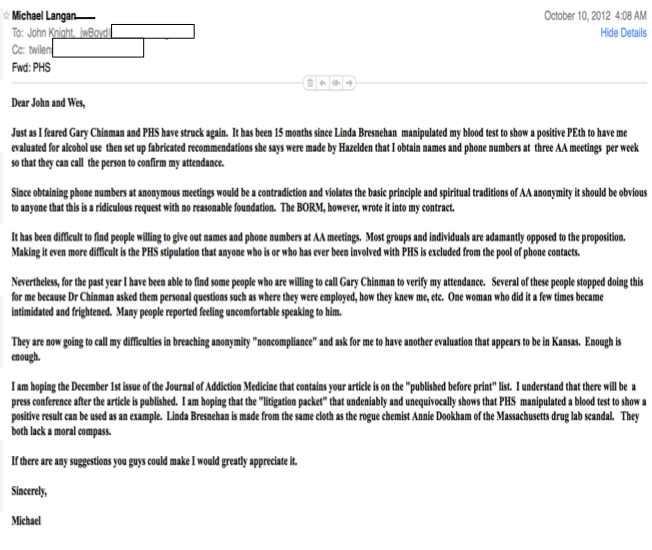
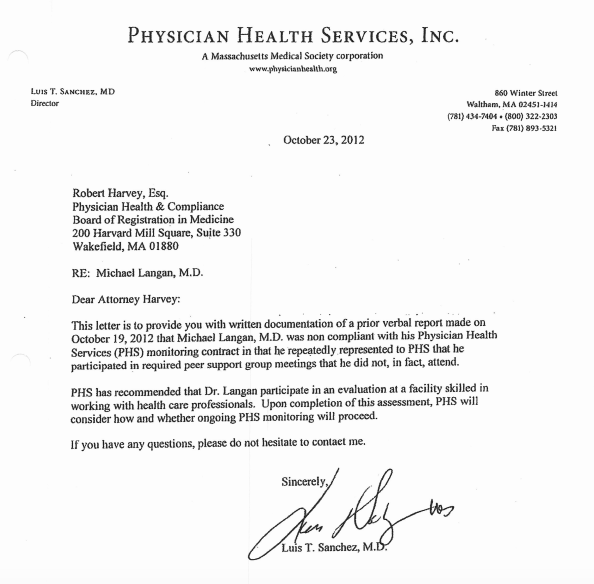
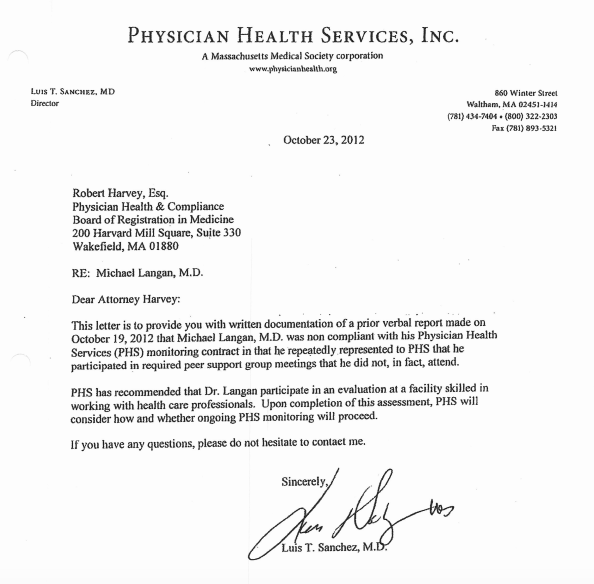
I was subsequently reported as “non-compliant” with AA meetings. They could not give any details of where or when. They then misrepresented a declaration of fact (I stated that I had started going to a specific meeting on a specific date) as an admission of guilt by saying I was referring to a different meeting. 10:23:12 PHS Letter to BORM-noncompliance.
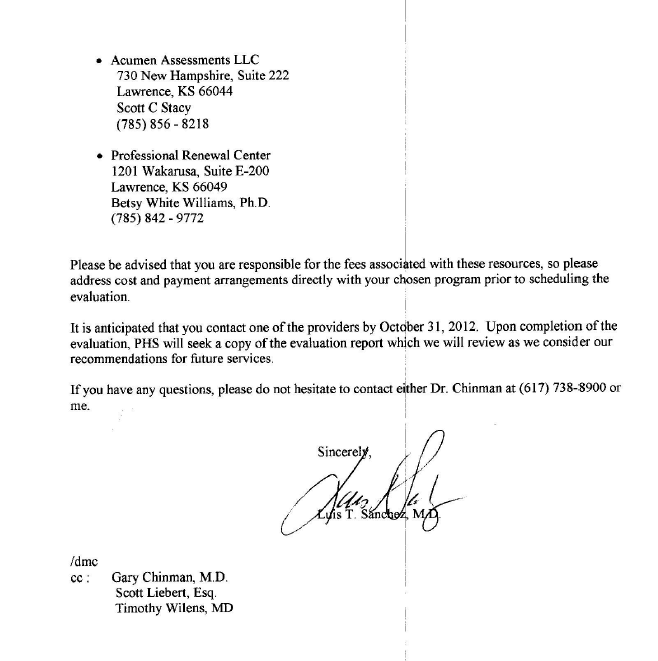
My Chief at MGH, his Chief and others held a conference with PHS and attempted to remove me from PHS and replace the monitoring contract with one of their own. They refused. When confronted with the fabricated test they dismissed it and focused on sending me to Kansas to one of the “disruptive physician” Psikhuskas where they are using polygraphs (despite the AMAs stance that it is junk science) and non-validated neuropsychological instruments that detect “character defects” to pathologize the normal.
I refused. Had I gone to Kansas I would have been given a false diagnosis and my career would be over. This is what they do.
Amy Daniels, the investigator for the College of American Pathologists contacted me in December of 2012 to see how things were going since USDTL “amended” the test. Daniels told me that the College of American Pathologists confirmed my allegations and, as an Accrediting Agency for Forensic Toxicology mandated that USDTL correct it. (Labs can lose accreditation if they do not comply with CAP Standards for Forensic Drug Testing). This was done on October 4, 2012.
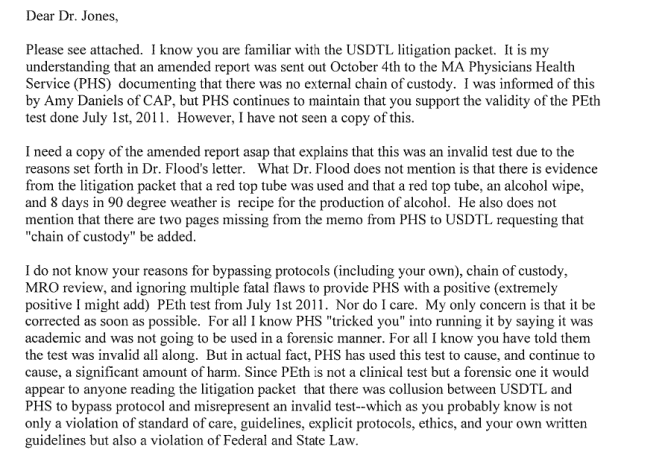
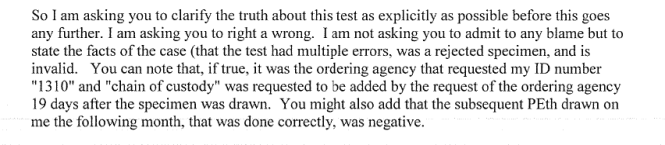
PHS denied any knowledge of an amended test. I also wrote an e-mail to Joseph Jones requesting the document but he did not reply.
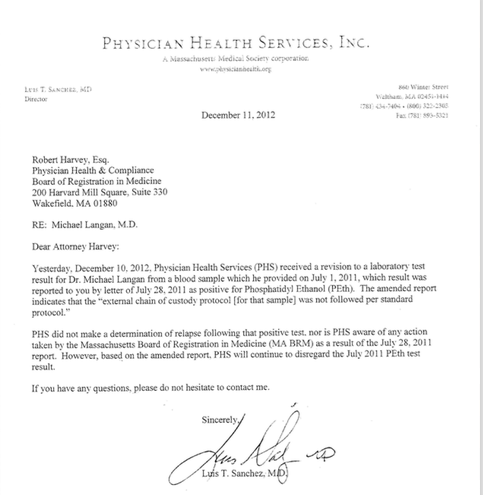
I contacted CAP. On December 11, 2012 Dr. Luis Sanchez wrote a letter stating “Yesterday, December 10 2012, Physician Health Services (PHS) received a revision to a laboratory test result”
“The amended report indicates that the external chain of custody protocol [for that sample] was not followed per standard protocol]”
Sanchez dismisses this test as irrelevant, rationalizing neither PHS nor the Board based any actions on the test and they would “continue to disregard” it.
The logic is that it was my behavior that resulted in any consequences. My “non-compliance” in October led to my suspension and the test had nothing to do with it. The sole reason for reporting me to the Board in 2011 was the positive test. There is no other pretext to use. It is misattribution of blame as without the test, now invalidated, there would have been no AA meetings to say I was non-compliant with.
In response to a civil complaint PHS, Quest and USDTL all took the position that the results of the fraudulent testing had absolutely nothing to do with anything.
And in response to the allegations of forensic fraud the labs claimed there was no forensic fraud because this was not a “Forensic” test but a “clinical” test. The argument was that “clinical” tests do not require chain-of-custody and it was his behavior not these tests that resulted in consequences.
As a “clinical” test I knew it was considered Protected Health Information (PHI) under the HIPAA-Privacy Rule. A patient must give written consent for any outside entities to see it. Obtaining lab tests previously required the consent of both the patient and the ordering provider. What PHS and the labs were apparently unaware of was the changes to the HIPAA-Privacy rule giving patients increased rights to access their PHI. The changes removed the ordering provider requirements. A patient has a right to obtain lab test results directly from the labs and has 30 days to do it. CAP agreed. USDTL sent me all of the documents. They can be seen below:
August 6, 2014 to Langan with health materials.
The documents sent by USDTL are notable for two things:
1. The e-mail from me to Joseph Jones dated December 10, 2012. It can be seen on page 22 of the USDTL documents. 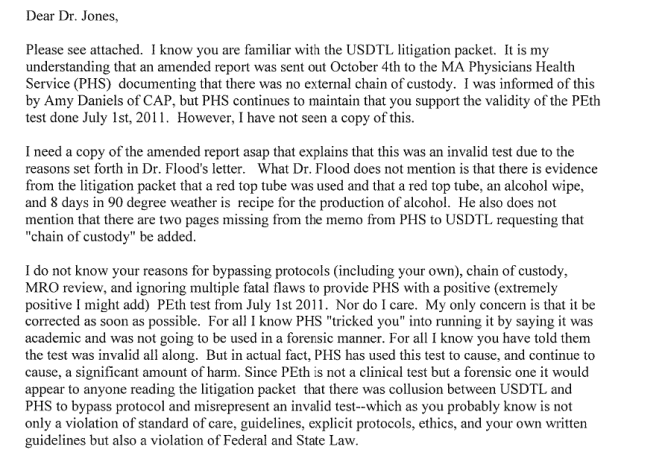
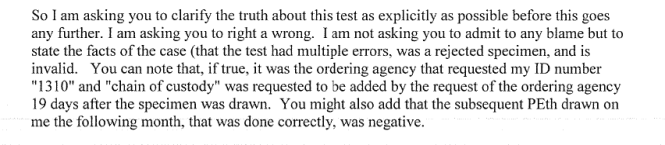
2. USDTL document confirming PHS knew the test was amended 67-days before they said they did.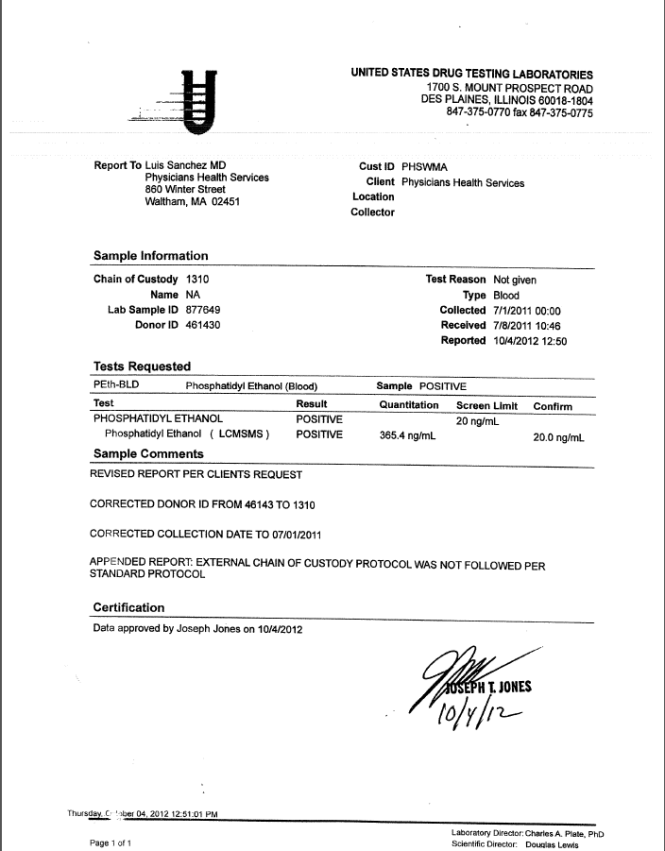
The document shows PHS and Sanchez were aware of the invalidity of the test on October 4, 2012. Instead of correcting things they initiated machinations to throw me under the bus. They officially reported me to the Board for non-compliance on October 19, 2012.
The December 11, 2012 letter signed by Sanchez states “Yesterday, December 10, 2012, PHS received a “revised report” regarding the test. The documents show he knew about it 67-days prior.
Although USDTL complied with the HIPAA-Privacy Rule and CAP, Quest did not. Quest Diagnostics refused to send me copies of their lab reports claiming it was confidential and protected information that required PHS consent. Quest required I sign a consent form with multiple stipulations regarding PHS. I refused and contacted the Department of Justice -Office of Civil Rights. The DOJ-OCR agreed with me and I received the Quest documents
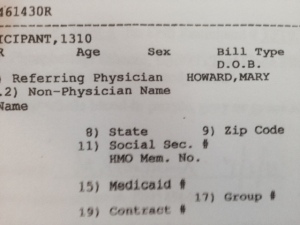
Remember a “clinical” test can only be ordered by a physician in the course of medical treatment. It requires authorization from the patient to obtain a “clinical” specimen and it requires written authorization as to who sees it. Referring physician was Mary Howard.
And below is the fax from PHS to Quest from July 1, 2011 also requested by Mary Howard. The signature on the front is not mine. In addition I gave the blood at 9:30 and was in my clinic at MGH at 12:23 so it couldn’t be. The WC 461430 R are dated July 2, 2011. This is a “clinical” not “forensic” sticker. The “R” indicates a red top tube. The other sticker is USDTL and indicates it was logged in on July 8, 2011.
What does it all mean? Blood left in a red top tube ferments. This is basic chemistry. The PEth test needs to be refrigerated and shipped overnight to prevent this. In addition it needs to be collected with a non-alcohol wipe in a tube that has an anti-coagulant or preservative so that it does not ferment. It requires strict procedure and protocol.
When I gave my blood on July 1st, 2011 it was as a “forensic” test per my contractual agreement with PHS.
On July 2, 2011 it was changed to “clinical.” Why? because “forensic” protocol would have invalidated it.
The only conceivable reason for doing this was to bypass chain-of-custody procedures. My unique identifier #1310 was removed and the clinical specimen number was used for chain-of-custody. The R in 461430R indicates a red top tube.
By holding on to it for one week the blood fermented. As it was July with an average temperature close to 90 they overshot their mark a bit. My level of 365 is consistent with heavy alcohol use–end stage half-gallon a day type drinking.
Quest then forwarded it to USDTL with specific instructions to process it as a “clinical” sample. USDTL complied and processed it as a clinical specimen which was reported it to PHS on July 14, 2011.
PHS then asked USDTL to add my forensic ID # 1310 and add a collection date of July 1, 2011 so it would appear “forensic” protocol was followed. The reason Jones signed the “litigation packet” on December 3, 2011 was because that was when the “litigation packet” was manufactured. A “clinical” sample does not produce one.
USDTL willingly complied with this request.
PHS then reported this as a “forensic” test to the Medical Board on July 19, 2011 and requested a reevaluation.
The distinction between “forensic” and “clinical” drug and alcohol testing is black and white. PHS is a monitoring program not a treatment provider. The fact that a monitoring agency with an MRO asked the lab to process and report it as a clinical sample and then used it forensically is an extreme outlier in terms of forensic fraud. The fact that they collected it forensically, removed the forensic components and let it sit in a warehouse for a week is abhorrent. The fact they then specifically requested it be processed as a clinical sample deepens the malice. The fact that they then reported it to the Board as a forensic sample and maintained it was forensic up until just recently makes it egregious. But the fact that the test was changed from “positive” to “invalid” on October 4th, 2012 and they then reported me to the Board on October 8th, 2012 for “noncompliance,” suppressed it and tried to send me to Kansas where I would be given a non-existent diagnosis to delegitimize me for damage control makes it wantonly egregious. This is political abuse of psychiatry.
Accountability requires both the provision of information and justification of what was done.
For doctors it is very difficult to obtain the information. As seen here, they put up a gauntlet to prevent the provision of what is immediate in all other drug testing programs. I now have all of the information. What it shows is clear. This was intentional. It was no accident. They knew what they were doing, knew it was wrong but did it anyway.
Accountability also requires that those who commit misconduct suffer consequences. The PHPs have also put up barriers to this. With no regulation or oversight they have no apparent accountability.
My understanding is that it works this way. The Medical Board, Medical Society and Departments of Public Health have no oversight. The MMS has an ethics committee but all they can do is “educate” the person if they feel there was a violation. The DPH won’t even look at it and the Board is complicit.
My understanding is that they have convinced law enforcement that this is a “parochial” issue that is best kept within the medical community. They have also created the impression that they are “friends” of law enforcement. I have heard from many doctors that they have tried to report misconduct, civil rights violations and crimes to the police, AGO, and other law enforcement agencies only to be turned back over to the PHP. By saying the physician is “impaired” it delegitimizes and invalidates the truth. “He’s just a sick doctor, we’ll take care of him.” That physician then suffers consequences effectively silencing the rest.
PHS uses the Board to enforce punitive measures and temporize. The Board puts blind faith in PHS. Blind faith that defies common sense ( mandating phone numbers at anonymous meetings) and disregards the law (Establishment Clause violations that are clear and well established). The Board also temporizes to cause damage.
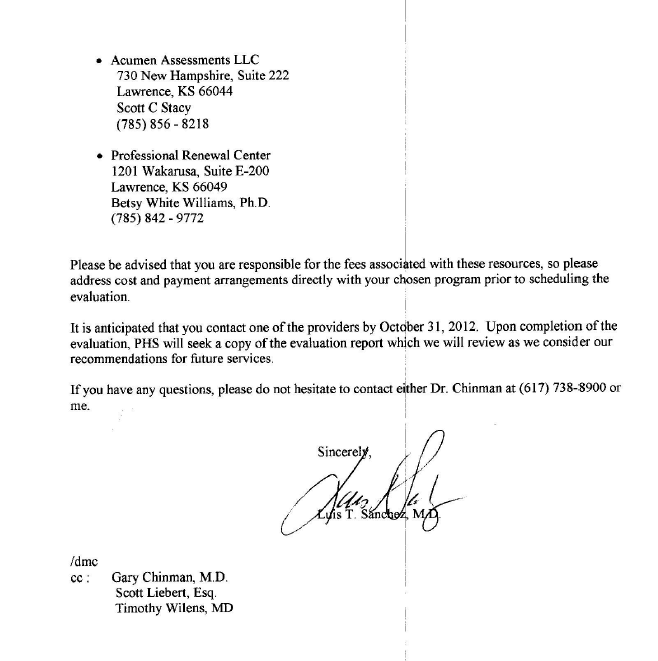
In my case they required a psychiatric behavioral evaluation. I was given the choice of Kansas and a few other Like-minded assessment centers.
After petitioning for multiple qualified psychiatrists that were summarily rejected months later for no reason one of the Board Attorneys suggested Dr. Patricia Recupero, M.D., J.D. who is Board Certified in Forensic Psychiatry and Addiction Psychiatry. The Board had used her in the past but not recently. Seeing that she had been used by the Board for fit-for-duty evaluations in the past the Board accepted my petition.
Dr. Recupero wrote an 87-page report. She concluded I was safe to practice medicine without supervision, that I had never had an alcohol use, abuse or dependence problem, and that PHS request for phone numbers was inappropriate. She also documented PHS misconduct throughout my contract and concluded it was PHS actions, not mine, that led to my suspension. What she describes is consistent with criminal harassment. She documents the falsification of neuropsychological tests and confirms the forensic fraud. What did the Board do? Ignored their very own recommended and approved evaluator.
One measure of integrity is truthfulness to words and deeds. These people claim professionalism, ethics and integrity. The documents show otherwise. The careers and lives of doctors are in these peoples hands.
Similar fraud is occurring across the country. This is an example of the institutional injustice that is killing physicians. Finding themselves entrapped with no way out, helpless and hopeless they are feeling themselves bereft of any shade of justice and killing themselves. These are nothing more than bullies and accountability is essential. The “disruptive physician” moral panic has harmed the Medical Profession.
Dr. Clive Body in his book Corporate Psychopaths writes that “Unethical leaders create unethical followers, which in turn create unethical companies and society suffers as a result.” And according to Dr. Robert Hare in Without Conscience “If we can’t spot them, we are doomed to be their victims, both as individuals and as a society. ”
Wes Boyd notes that valid complaints from physicians are often dismissed as “bellyaching” by the PHPs. Complacent that these are just good guys helping doctors and protecting the public the complaints are dismissed, tabled, deflected or otherwise ignored. Bellyaching?? Is this bellyaching.
It is my opinion that what you see here is indefensible Procedurally, Ethically, and Legally.
Procedurally it goes beyond negligence and represents fraud. It violates every procedural guideline, regulation and standard of care including their very own.
Ethically it violates everything from the Hippocratic Oath to AMA Medical Ethics to the MRO Code of Conduct.
And where was PHS MRO Wayne Gavryck? By my count he violated at least 4 of the 6 Codes of Ethical Conduct.
What was done here violates the most fundamental ethical principles of Medicine -Autonomy, Beneficence, Nonmaleficence and justice.
Intentionally falsifying a laboratory or diagnostic test to refer for an evaluation or support a diagnosis or give unwarranted “treatment” is unconscionable. Abuse under the utility of medical coloration is especially egregious.
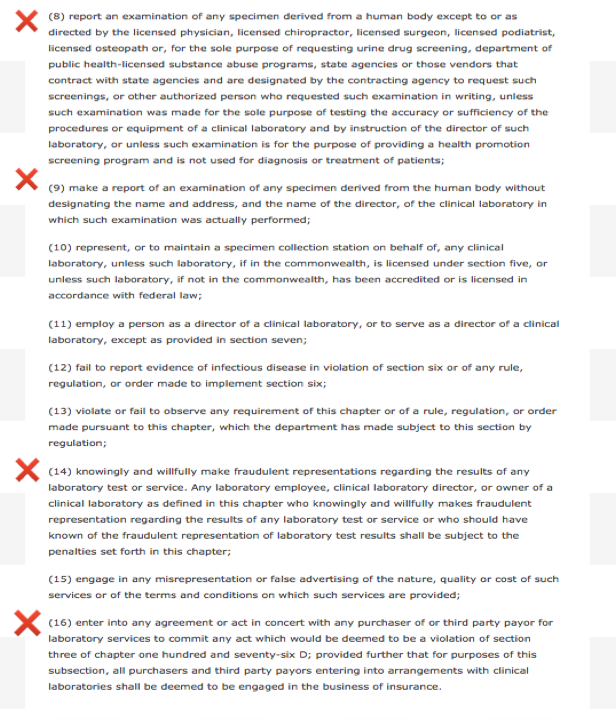
The information provided herein should negate any “peer-review” protection or immunity afforded PHS as it is undeniably and egregiously in “bad faith.” Moreover, the ordering a “clinical” test is outside PHS scope, practice, and function of PHS. According to M.G.L. c. 111, § 203 (c):
An individual or institution, including a licensed or public hospital, physician credentialing verification service operated by a society or organization of medical professionals for the purpose of providing credentialing information to health care entities, or licensed nursing home reporting, providing information, opinion, counsel or services to a medical peer review committee, or participation in the procedures required by this section, shall not be liable in a suit for damages by reason of having furnished such information, opinion, counsel or services or by reason of such participation, provided, that such individual or institution acted in good faith and with a reasonable belief that said actions were warranted in connection with or in furtherance of the function of said committee or the procedures required by this section.
Dr. Luis Sanchez and Dr. Wayne Gavryck need to be held to the same professional standards as the rest of us.
If you can support either of them procedurally, ethically, or legally, any one of them, then I will turn in my medical license with a bow on it. If they did not commit negligent fraud by standards of care and procedural guidelines, egregious moral disengagement in violation of ALL ethical codes for the medical profession and society and break the law then disprove me. Just one will do.
But you can’t do this then I ask that you speak up and take a stand. Either defend them or help me hold them accountable. If a crime is committed it needs to be addressed. Ignoring encourages more of the same.
And if this cannot be supported procedurally, ethically or legally then I want to know what is going to be done about it?
How low does the moral compass have to go before someone takes action?
Doctors are dying across the country because of people just like this. They have set up a scaffold that removes the usual checks and balances and removed accountability. It is this institutional justice that is driving many doctors to suicide.
So the evidence is above. Either defend them or help me draw unwanted attention to this culture of bullying and abuse. So I am asking you to contemplate if what you see here is ethically, procedurally or legally sound. If you can show just one of these then I stand corrected. But if you cannot justify this on any level then I want you to help me expose this criminal enterprise. Either defend it or fight it. Silence and obfuscation are not acceptable.




























 also follow their own
also follow their own 
 Both the donor ID # and chain of custody are listed as 461430.
Both the donor ID # and chain of custody are listed as 461430.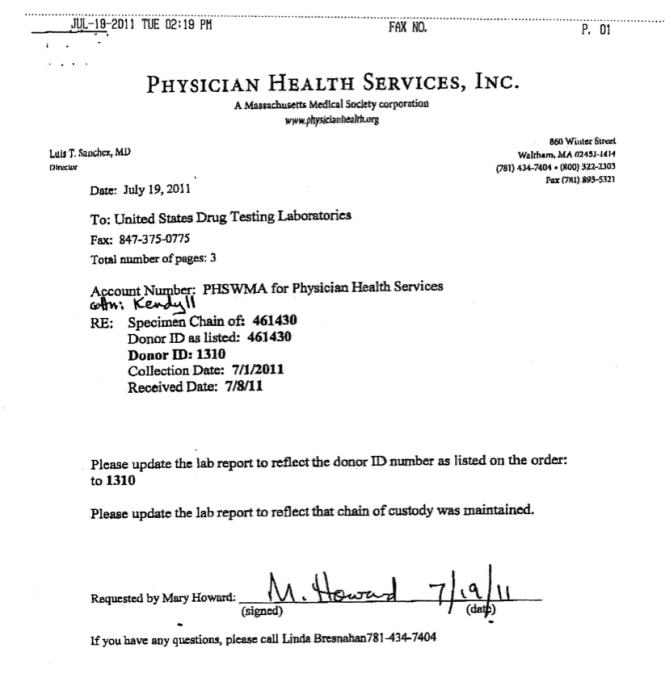





 Accountability needs to be rooted in organizational purpose and public trust.
Accountability needs to be rooted in organizational purpose and public trust. ce of unchecked power. The only two factors that constrain corruption are moral virtue and deterrence.
ce of unchecked power. The only two factors that constrain corruption are moral virtue and deterrence. arketed it as the PEthStat.
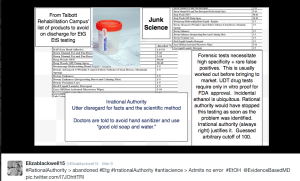
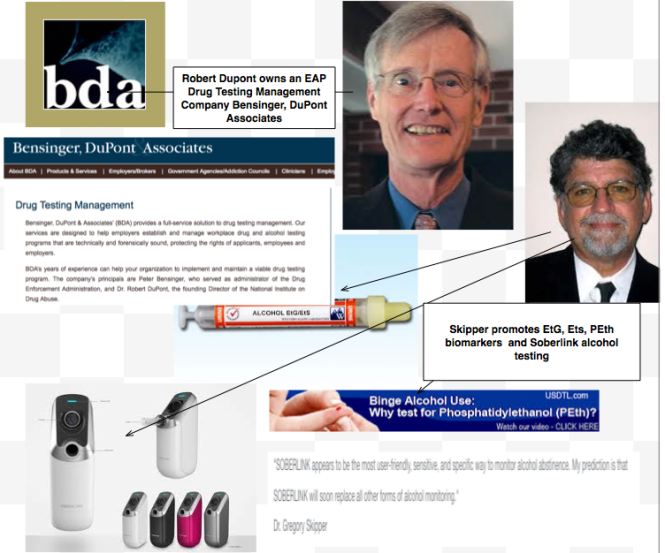
State Physician Health Programs are now using the EtG and adding the PEth to confirm alcohol ingestion. And just as they did with the EtG the claims of reliability are grand but without foundation.
All speculative A=B oversimplified thinking that ignores the myriad other factors involved. The science is empty if you remove the dregs of filler and puff. And the conflicts of interest are mind-boggling.
arketed it as the PEthStat.
State Physician Health Programs are now using the EtG and adding the PEth to confirm alcohol ingestion. And just as they did with the EtG the claims of reliability are grand but without foundation.
All speculative A=B oversimplified thinking that ignores the myriad other factors involved. The science is empty if you remove the dregs of filler and puff. And the conflicts of interest are mind-boggling.