Posted on the Texas Medical Licensing Law Blog December 17, 2014
Physician Health Programs
Clinical Psychiatry News (Letter to the editor) PHPs: part of the problem
I was heartened to read Doug Brunk’s recent article on the need to address the problem of physician suicide within the medical profession (“Medicine grapples with physician suicide,” February 2015, p. 1). As a physician who knows of many suicides of good doctors, I have been working with Dr. Pamela Wible to expose this phenomenon gradually (as it is difficult to get one’s head around if presented all at once) and have been making some gains.
Another issue tied to the incredible stresses endured by physicians is rooted in the groupthink within state physician health programs (PHPs).
Dr. John R. Knight and Dr. J. Wesley Boyd (who collectively have more than 25 years’ experience with the Massachusetts PHP) have been trying to expose the ethical and managerial issues tied to the “diversion” or “safe haven” programs for physicians with alcohol or drug problems (J. Addict. Med. 2012;6:243-6). My posts on disruptedphysician.com also examine these issues.
Meanwhile, a 2014 performance audit of the North Carolina Physicians Health Program found that “abuse could occur but not be detected” and revealed conflicts of interest between the state’s PHP programs and “PHP-approved” assessment centers. Another key finding is the PHP “created the appearance of conflicts of interest” by allowing treatment centers that receive referrals to fund its retreats and scholarships for physicians who could not afford treatment directly to treatment centers. The audit also uncovered other disturbing practices that lead to undue pressure on North Carolina’s physicians. For details, check out the report here.
More recently, several health professionals have filed a class action suit in the Eastern District of Michigan against several entities, including the state’s Health Professional Recovery Program. The lawsuit alleges, among other things, that the involuntary program has become a “highly punitive” one in which “health professionals are forced into extensive and unnecessary substance abuse/dependence treatment.”
Getting the word out about the impact of PHPs on physicians (and other health care professionals) has proven difficult for many reasons, but we must remain vigilant. The health of our fellow physicians and the medical profession depends on it.
Michael Lawrence Langan, M.D.
Brookline, Mass.
Citation Details
Title: PHPs: part of the problem.(Letter to the editor)
Author: Michael Lawrence Langan
Publication: Clinical Psychiatry News (Magazine/Journal)
Date: April 1, 2015
Publisher: International Medical News Group
Volume: 43 Issue: 4 Page: 14(1)
May 3rd, 2013–Dr. Steve Adelman: The Mentality of What’s in Charge and Proof that Stupidity Often Reigns!
As the oldest medical society in the United States the Massachusetts Medical Society can count some of the greatest minds in the history of American medicine as members but this guy is not one of them. My how far we have fallen! This same author has also unintelligibly and bizarrely compared the medical profession to Barbra Streisand’s face and tried to send a medical student who (naively) presented to him with “sleep apnea” for an evaluation in Kansas for “schizophrenia.” He also opportunistically blamed the Boston Marathon bombing on “marijuana withdrawal” as seen below:
Physician Suicide: The Role of Hopelessness, Helplessness and Defeat.
Although no reliable statistics yet exist, anecdotal reports suggest a marked rise inphysician suicide in recent years. From the reports I am receiving it is a lot more than the oft cited “medical school class” of 400 per year.
This necessitates an evaluation of predisposing risk factors such as substance abuse and depression, but also requires a critical examination of what external forces may be involved. What acute and cumulative situational and psychosocial factors are involved in the descent from suicidal ideation to planning to completion? What makes suicide a potential option for doctors and what acute events precipitate and trigger the final act?
Depression and Substance Abuse no Different from General Population
The prevalence of depression in physicians is close to that of the general population1,2 and, if one looks critically at the evidence based literature, substance abuse in medical professionals approximates that of the general population. Controlled studies using DSM diagnostic criteria indicate that physicians have the same rates (8-14%) of substance abuse and dependence as the general population,3 and slightly lower rates compared to other occupations.4,5 Epidemiological surveys reveal the same. Hughes, et al.6 reported a lifetime prevalence of drug or alcohol abuse or dependence in physicians of 7.9%, markedly less than the 14.6% prevalence reported in the general population by Kessler.7
Job Stress and Untreated Mental Illness Risk Factors
Job stress coupled with inadequate treatment for mental illness may be factors contributing to physician suicide according to one recent study. Using data from the National Violent Death Reporting System, Gold, Sen, & Schwenk, 2013 8 compared 203 physicians who had committed suicide to more than 31,000 non-physicians and found that having a known mental health disorder or a job problem that contributed to the suicide significantly predicted being a physician.
Physicians were 3.12 times more likely to have a job problem as a contributing factor. In addition, toxicology testing showed low rates of medication treatment. The authors concluded that inadequate treatment and increased problems related to job stress are potentially modifiable risk factors to reduce suicidal death among physicians. They also warned that the database used likely underestimated physician suicides because of “underreporting and even deliberate miscoding because of the stigma attached.”8
Few studies have evaluated the psychosocial stressors surrounding physician suicide but there is no reason to believe they are any different from the rest of the population. Although the triggering life events and specific stressors may vary outside, the inner psyche and undercurrent of thoughts and feelings should remains the same. Perhaps the same drivers of suicide identified in other populations are contributing to physician suicide.

Perceived Helplessness, Hopelessness, Bullying and Defeat
Perceived helplessness is significantly associated with suicide as is9Hopelessness10,11 Bullying is known to be a predominant trigger for adolescent suicide12-14 One study found that adolescents in custody who were bullied were 9.22 times more likely to attempt suicide than those were not bullied.15
Heightened perceptions of defeat and entrapment are known to be powerful contributors to suicide.16,17
The “Cry of Pain” model 18,19 specifies that people are particularly prone to suicide when life experiences are interpreted as signaling defeat which is defined as a sense of “failed struggle” or loss of social position and resources.. The person is unable to identify an escape from or resolution to a defeating situation, a sense of entrapment proliferates with the perception of no way out, and this provides the central impetus for ending ones life. There is a helplessness and hopelessness that precipitates the descent from ideation, to planning, and then to finality.
Organizational Justice Important Protective Factor
In a study on Italian and Swedish female physicians, degrading experiences and harassment at work were found to be the most powerful independent variables contributing to suicidal thoughts.20 Degrading work experiences harassment, and lack of control over working conditions were found to be associated with suicidal thoughts among Italian and Swedish male university physicians.21
Evidence exists for the role of rescue factors (i.e. social support) as buffers against suicide in the face of varying degrees of life stress.22,23 The study of female physicians revealed meetings to discuss stressful work experiences as a potential protective factor, 20 and support at work when difficulties arose appeared to be a protective factor for the male physicians.21 In line with this, studies of Finnish physicians found that control over one’s work and organizational justice were the most important determinants of work-related wellbeing.24,25 Organizational justice has been identified as a psychosocial predictor of health and wellbeing. 26 27 Low organizational justice has been identified as a notable risk factor for psychological distress and depression.28,29

Historical Precedent-the Suicides at Ridgeview
Could these factors be playing a role in physician suicide? They evidently did at the Ridgeview Institute, a drug and alcohol treatment program for impaired physicians in Metropolitan Atlanta created by G. Douglas Talbott.
Talbott helped organize and served as past president of the American Society of Addiction Medicine (ASAM) and was a formative figure in the American Medical Association’s (AMA’s) Impaired Physician Program. He has owned and directed a number of treatment facilities for impaired professionals, most recently the Talbott Recovery Campus in Atlanta, one of the preferred referrals for physicians ordered into evaluation and treatment by licensing boards.
After creating the DeKalb County Impaired Physicians Committee for the Medical Association of Georgia, Talbott founded the Georgia Disabled Doctors Program in 1975 in part because “traditional one-month treatment programs are inadequate for disabled doctors.” According to Talbott, rehabilitation programs that evaluate and treat the rest of the population for substance abuse issues are incapable of doing so in doctors as they are unlike others. He bases this uniqueness on “incredibly high denial”, and what he calls the “four MDs,” “M-Deity”, “Massive Denial” “Militant Defensiveness”, and “More Drugs.”30
Contingency Management = Extortion Using Medical License
According to Talbott, “impaired doctors must first acknowledge their addiction and overcome their ‘terminal uniqueness’ before they can deal with a drug or alcohol problem.” “Terminal uniqueness “ is a phrase Talbott uses to describe doctors’ tendency to think they can heal themselves. “M-Deity” refers to doctors “being trained to think they’re God,”31 an unfounded generalization considering the vast diversity of individuals that make up our profession. This attitude, according to some critics, stems from the personal histories of the treatment staff, including Talbott, who are recovering alcoholics and addicts themselves. One such critic was Assistant Surgeon General under C. Everett Koop John C. Duffy who said that Ridgeview suffered from a “boot-camp mentality” toward physicians under their care and “assume every physician suffering from substance abuse is the same lying, stealing, cheating, manipulating individual they were when they had the illness. Certainly some physicians are manipulative, but it’s naïve to label all physicians with these problems.”32
American Society of Addiction Medicine (ASAM) President (1981-1983) LeClair Bissell was also highly critical of Talbott’s approach. Bissell, co-author of the first textbook of ethics for addiction professionals 33 when asked if there was any justification to the claim that doctors are sicker than other people and more vulnerable to addiction replied:
“Well, based on my treatment experience, I think they are less sick and much easier to treat than many other groups. I think one reason for that is that in order to become a physician…one has to have jumped over a great many hurdles. One must pass the exams, survive the screening tests and the interviews, be able to organize oneself well enough to do examinations and so on, and be observed by a good many colleagues along the way. Therefore I think the more grossly psychotic, or sicker, are frequently screened out along the way. The ones we get in treatment are usually people who are less brain-damaged, are still quite capable of learning, are reasonably bright. Not only that, but they are quite well motivated in most cases to hang on to their licenses, the threat of the loss of which is frequently what puts them in treatment in the first place. So are they hard to treat? No! Are they easy patients? Yes! Are they more likely to be addicted than other groups? We don’t know.”34
“I’m not much for the bullying that goes along with some of these programs,” Bissell commented to the Atlanta Journal and Constitution in 1987.31
The Constitution did a series of reports after five inpatients committed suicide during a four-year period at Ridgeview.35 In addition there were at least 20 more who had killed themselves over the preceding 12 years after leaving the treatment center.32
 Bissell, the recipient of the 1997 Elizabeth Blackwell Award for outstanding contributions to the cause of women and medicine remarked: “When you’ve got them by the license, that’s pretty strong leverage. You shouldn’t have to pound on them so much. You could be asking for trouble.” 31
Bissell, the recipient of the 1997 Elizabeth Blackwell Award for outstanding contributions to the cause of women and medicine remarked: “When you’ve got them by the license, that’s pretty strong leverage. You shouldn’t have to pound on them so much. You could be asking for trouble.” 31
According to Bissell: “There’s a lot of debate in the field over whether treatment imposed by threats is worthwhile…To a large degree a person has to seek the treatment on his own accord before it will work for him.”31
A jury awarded $1.3 million to the widow of one of the deceased physicians against Ridgeview,36 and other lawsuits initiated on behalf of suicides were settled out of court.35
The Constitution reported that doctors entered the program under threats of loss of licensure “even when they would prefer treatment that is cheaper and closer to home.” 37
The paper also noted that Ridgeview “enjoys unparalleled connections with many local and state medical societies that work with troubled doctors,” “licensing boards often seek recommendations from such groups in devising an approved treatment plan,” and those in charge are often “physicians who themselves have successfully completed Ridgeview’s program.”37
The cost of a 28-day program for nonprofessionals at Ridgeview in 1987 was $10,000 while the cost was “higher for those going through impaired-health professionals program,” which lasted months rather than 28 days.32
In 1997 William L. White interviewed Bissell whom he called “one of the pioneers in the treatment of impaired professionals.” The interview was not published until after hear death in 2008 per her request. Noting her book Alcoholism in the Professions 38 “remains one of the classics in the field”, White asked her when those in the field began to see physicians and other professionals as a special treatment population. She replied:
“When they started making money in alcoholism. As soon as insurance started covering treatment, suddenly you heard that residential treatment was necessary for almost everybody. And since alcoholic docs had tons of money compared to the rest of the public, they not only needed residential treatment, they needed residential treatment in a special treatment facility for many months as opposed to the shorter periods of time that other people needed.”39

Talbott claimed a “92.3 percent recovery rate, according to information compiled from a five-year follow-up survey based on complete abstinence and other treatment.”40
“There is nothing special about a doctor’s alcoholism,” said Bissel
“”These special facilities will tell you that they come up with really wonderful recovery rates. They do. And the reason they do is that any time you can grab a professional person by the license and compel him or her into treatment and force them to cooperate with that treatment and then monitor them for years, you’ll get good outcomes—in the high 80s or low 90s in recovery rates—no matter what else you do.”39
“The ones I think are really the best ones were not specialized. There were other well-known specialty clinics that claimed all the docs they treated got well, which is sheer rot. They harmed a great many people, keeping them for long, unnecessary treatments and seeing to it that they hit their financial bottom for sure: kids being yanked out of college, being forced to sell homes to pay for treatment, and otherwise being blackmailed on the grounds that your husband has a fatal disease. It’s ugly.”39
Stanton Peele’s “In the Belly of the American Society of Addiction Medicine Beast” describes the coercion, bullying, threats and indoctrination that are standard operating procedure in Talbott’s facilities.41 Uncooperative patients, “and this covers a range of sins of commission or omission including offering one’s opinion about one’s treatment,” are “threatened with expulsion and with not being certified-or advocated for with their Boards.”41 The cornerstone of treatment is 12-step spiritual recovery. All new patients are indoctrinated into A.A. and coerced to confess they are addicts or alcoholics. Failure to participate in A.A. and 12-step spirituality means expulsion from the program with the anticipated result being loss of one’s medical license.

Fraud, Malpractice, False Diagnoses and False imprisonment
In May 1999 Talbott stepped down as president of the American Society of Addiction Medicine (ASAM) as a jury awarded Dr. Leonard Masters a judgment of $1.3 million in actual damages and an undisclosed sum in punitive damages for fraud, malpractice, and the novel claim of false imprisonment.42 The fraud finding required a finding that errors in the diagnosis were intentional. After being accused of excessive prescribing of narcotics to his chronic pain patients, Masters was told by the director of the Florida PHP that he could either surrender his medical license until the allegations were disproved or submit to a four-day evaluation. Masters agreed to the latter, thinking he would have an objective and fair evaluation, but was instead diagnosed as “alcohol dependent” and coerced into the Talbott recovery program. He was forced to stay in the program under threat of his medical license as staff would routinely threaten to report any doctor who questioned any aspect of their diagnosis or treatment to their state medical boards “as being an impaired physician, leaving necessary treatment against medical advice”42 which would mean the loss of his licensure.
However, Masters was not an alcoholic. According to his attorney, Eric. S. Block, “No one ever accused him of having a problem with alcohol. Not his friends, not his wife, not his seven children, not his fellow doctors, not his employees, not his employers, No one.” 43 He was released 4 months later and forced to sign a five-year “continuing care” contract with the PHP, also under continued threat of his medical license. Talbott faced no professional repercussions and no changes in the treatment protocols were made. Talbott continued to present himself and ASAM as the most qualified advocate for the assessment and treatment of medical professionals for substance abuse and addiction up until his death last year.44

Same System Imposed on Doctors Today—Institutional Injustice Worse due to Laboratory Developed Tests. Fortified Scaffold and Tightened the Noose.
In almost all states today any physician referred for an assessment for substance abuse will be mandated to do so in a facility just like Ridgeview. There is no choice. There is one difference however. When the Ridgeview suicides occurred the plethora of laboratory developed tests were not yet introduced.
A decade ago Dr. Gregory Skipper introduced the first laboratory developed test for forensic testing and used it on doctors in physician health programs. These non-FDA approved tests of unknown validity presented a new unpredictable variable into the mix with a positive test necessitating another assessment at an out of state treatment facility—a “PHP-approved” assessment facility. The addition of this laboratory Russian Roulette renders the current system much worse than it was at the time of the Ridgeview suicides.
And if a positive test occurs there are no safeguards protecting the donor. LDTs are unregulated by the FDA. There is no oversight and no one to file a complaint with.
In addition state PHPs have no oversight or regulation. They police themselves. Medical boards, departments of public health and medical societies provide no oversight. Accountability is absent.
Moreover they have apparently convinced law enforcement that when it comes to doctors it is a “parochial issue” best handled by the medical community. I have been hearing from doctors all over the country who have tried to report crimes to the local police, the state Attorney General and other law enforcement agencies only to be turned back over to the very perpetrators of the crimes. “He’s a sick doctor, we’ll take care of him.”
The “swift and certain consequences” of this are an effective means of keeping the majority silent. Likewise doctors have been going to the media only to have the door slammed in their faces because the media has generally bought in to the “impaired” and “disruptive” physician construct these same people developed through propaganda, misinformation and moral panics.
Urgent Need to Admit to the Problem
There has been an increase in physician suicide in the past decade. By my estimate the numbers are going to be far higher than the oft-cited 400 per year. The speculation as to cause has been unenlightening and in fact frustrating. Knowledge of anatomy, access to dangerous drugs, increased workload and even student loans have been proposed as contributing factors. Although there has been some tangential mention of physician health programs it has been indirect.
Direct and defined discussion is necessary and state PHPs need to be named as a possible contributor to suicide. Admitting the possibility there is a problem is the first crucial step in defining and addressing the problem. The 1980s historical precedent is correlated with physician suicide. The current system is not only based on Ridgeview but has been fortified in scope and power. The physician health movement has effectively removed due process from doctors while removing answerability and accountability from themselves.
And they have not only fortified the scaffold but widened it from substance abusing doctors to all doctors. “Potential impairment” and “relapse without use” were introduced without any meaningful resistance and they are now using a panoply of non-FDA approved laboratory developed tests of unknown validity to test for substances of abuse in a zero-tolerance abstinence based monitoring program.
With no regulatory oversight the stage is set not only for error but misuse as witch-pricking devices for punishment and control. Doctors across the country are complaining of the very same abuses Leonard Masters did–false diagnoses, misdiagnosis, unneeded treatment and fraud.
In summary, any doctor who is referred to their state PHP today is required to have any assessment and treatment at a “PHP-approved” facility based on Ridgeview. It is mandated. There is no choice. Coercion, control and abuse at Ridgeview was associated with multiple suicides in doctors in the 1980s.
The use of non-FDA approved tests of unknown validity worsens the abuse and fits the “cry of pain” model of hopelessness, helplessness and despair.
Locus of control is lost. Organizational justice is absent. The temporal relationship is clear.
Why is this still the elephant in the room?
This needs to be named, defined and openly discussed and debated. How many more must die before we speak up?
Please help me get the conversation going. I need allies.

- Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Archives of internal medicine. Jul 13 1998;158(13):1422-1426.
- Frank E, Dingle AD. Self-reported depression and suicide attempts among U.S. women physicians. The American journal of psychiatry. Dec 1999;156(12):1887-1894.
- Brewster JM. Prevalence of alcohol and other drug problems among physicians. JAMA : the journal of the American Medical Association. Apr 11 1986;255(14):1913-1920.
- Anthony J, Eaton W, Mandell W, al. e. Psychoactive Drug Dependence and abuse: More Common in Some Occupations than in Others? Journal of Employee Assistance Res. 1992;1:148-186.
- Stinson F, DeBakely S, Steffens R. Prevalence of DSM-III-R Alcohol abuse and/or dependence among selected occupations. Alchohol Health Research World. 1992;16:165-172.
- Hughes PH, Brandenburg N, Baldwin DC, Jr., et al. Prevalence of substance use among US physicians. JAMA : the journal of the American Medical Association. May 6 1992;267(17):2333-2339.
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication.Archives of general psychiatry. Jun 2005;62(6):593-602.
- Gold KJ, Sen A, Schwenk TL. Details on suicide among US physicians: data from the National Violent Death Reporting System. General hospital psychiatry. Jan-Feb 2013;35(1):45-49.
- Rivers I, Noret N. Potential suicide ideation and its association with observing bullying at school.The Journal of adolescent health : official publication of the Society for Adolescent Medicine. Jul 2013;53(1 Suppl):S32-36.
- Lester D, Walker RL. Hopelessness, helplessness, and haplessness as predictors of suicidal ideation. Omega. 2007;55(4):321-324.
- Beck AT. Hopelessness as a predictor of eventual suicide. Annals of the New York Academy of Sciences. 1986;487:90-96.
- Hinduja S, Patchin JW. Bullying, cyberbullying, and suicide. Archives of suicide research : official journal of the International Academy for Suicide Research. 2010;14(3):206-221.
- Hertz MF, Donato I, Wright J. Bullying and suicide: a public health approach.The Journal of adolescent health : official publication of the Society for Adolescent Medicine. Jul 2013;53(1 Suppl):S1-3.
- Kim YS, Leventhal B. Bullying and suicide. A review. International journal of adolescent medicine and health. Apr-Jun 2008;20(2):133-154.
- Kiriakidis SP. Bullying and suicide attempts among adolescents kept in custody. Crisis.2008;29(4):216-218.
- Taylor PJ, Gooding P, Wood AM, Tarrier N. The role of defeat and entrapment in depression, anxiety, and suicide. Psychological bulletin. May 2011;137(3):391-420.
- Lester D. Defeat and entrapment as predictors of depression and suicidal ideation versus hopelessness and helplessness. Psychological reports. Oct 2012;111(2):498-501.
- Williams JMG. Cry of Pain. Harmondsworth: Penguin; 1997.
- Williams JMG, Crane C, Barnhofer T, Duggan DS. Psychology and suicidal behavior: elaborating the entrapment model. In: Hawton K, ed. Prevention and treatment of suicidal behavior: from science to practice. Oxford: Oxford University Press; 2005:71-89.
- Fridner A, Belkic K, Marini M, Minucci D, Pavan L, Schenck-Gustafsson K. Survey on recent suicidal ideation among female university hospital physicians in Sweden and Italy (the HOUPE study): cross-sectional associations with work stressors. Gender medicine. Apr 2009;6(1):314-328.
- Fridner A, Belkic K, Minucci D, et al. Work environment and recent suicidal thoughts among male university hospital physicians in Sweden and Italy: the health and organization among university hospital physicians in Europe (HOUPE) study. Gender medicine. Aug 2011;8(4):269-279.
- Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: Risks and protectors.Pediatrics. 2001;107(485).
- Clum GA, Febbraro GAR. Stress, social support and problem-solving appraisal/skill: Prediction of suicide severity within a college sample. Journal of Psychopathology and Behavioral Assessment. 1994;16:37-46.
- Lindfors PM, Meretoja OA, Toyry SM, Luukkonen RA, Elovainio MJ, Leino TJ. Job satisfaction, work ability and life satisfaction among Finnish anaesthesiologists. Acta anaesthesiologica Scandinavica. Aug 2007;51(7):815-822.
- Heponiemi T, Kuusio H, Sinervo T, Elovainio M. Job attitudes and well-being among public vs. private physicians: organizational justice and job control as mediators. European journal of public health. Aug 2011;21(4):520-525.
- Elovainio M, Kivimaki M, Vahtera J. Organizational justice: evidence of a new psychosocial predictor of health. Am J Public Health. Jan 2002;92(1):105-108.
- Lawson KJ, Noblet AJ, Rodwell JJ. Promoting employee wellbeing: the relevance of work characteristics and organizational justice. Health promotion international. Sep 2009;24(3):223-233.
- Hayashi T, Odagiri Y, Ohya Y, Tanaka K, Shimomitsu T. Organizational justice, willingness to work, and psychological distress: results from a private Japanese company. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. Feb 2011;53(2):174-181.
- Lang J, Bliese PD, Lang JW, Adler AB. Work gets unfair for the depressed: cross-lagged relations between organizational justice perceptions and depressive symptoms. The Journal of applied psychology. May 2011;96(3):602-618.
- Gonzales L. When Doctors are Addicts: For physicians getting Molly Kellogg is easy. Getting help is not. Chicago Reader. July 28, 1988, 1988.
- King M, Durcanin C. The suicides at Ridgeview Institute: A Doctor’s treatment program may be too tough, some say. Atlanta Journal and Constitution.December 18, 1987a, 1987: A12.
- Durcanin C, King M. The suicides at Ridgeview Institute: Suicides mar success at Ridgeview with troubled professionals. Atlanta Journal and Constitution.December 18, 1987, 1987: A13.
- Bissell L, Royce JE. Ethics for Addiction Professionals. Center City, Minnesota: Hazelden; 1987.
- Addiction Scientists from the USA: LeClair Bissell. In: Edwards G, ed.Addiction: Evolution of a Specialist Field. 1 ed: Wiley, John & Sons, Incorporated; 2002:408.
- Durcanin C. The suicides at Ridgeview Institute: Staff members didn’t believe Michigan doctor was suicidal. Atlanta Journal and Constitution. December 18, 1987, 1987: A8.
- Ricks WS. Ridgeview Institute loses $1.3 million in suit over suicide. Atlanta Journal and Constitution. October 11, 1987, 1987: A1.
- King M, Durcanin C. The suicides at Ridgeview Institute: Many drug-using doctors driven to Ridgeview by fear of losing licenses. Atlanta Journal and Constitution. December 18, 1987b, 1987: A1.
- Bissell L, Haberman PW. Alcoholism in the Professions. Oxford University Press; 1984.
- White W. Reflections of an addiction treatment pioneer. An Interview with LeClair Bissell, MD (1928-2008), conducted January 22, 1997. Posted athttp://www.williamwhitepapers.com. 2011.
- Williams c. Health care field chemical dependency threat cited. The Tuscaloosa News. January 16, 1988, 1988: 16.
- Peele S. In the Belly of the American Society of Addiction Medicine Beast. The Stanton Peele Addiction Website (accessed March 28, 2014)http://web.archive.org/web/20080514153437/http://www.peele.net/debate/talbott.html.
- Ursery S. $1.3M verdict coaxes a deal for doctor’s coerced rehab. Fulton County Daily Report.May 12, 1999b 1999.
- Ursery S. I was wrongly held in alcohol center, doctor charges. Fulton Count y Daily Report. April 27, 1999a 1999.
- Parker J. George Talbott’s Abuse of Dr. Leon Masters MD (http://medicalwhistleblowernetwork.jigsy.com/george-talbott-s-abuse-of-leon-masters ).Medical Whistelblower Advocacy Network.

The Proposed Expansion of PHPs. Illegitimate and Irrational Authority and the Urgent need for a critical analysis of the “PHP-Blueprint”
“If you tell a lie big enough and keep repeating it, people will eventually come to believe it.” –Joseph Goebbels

1. National Physician Health Program Blueprint Study Publications List
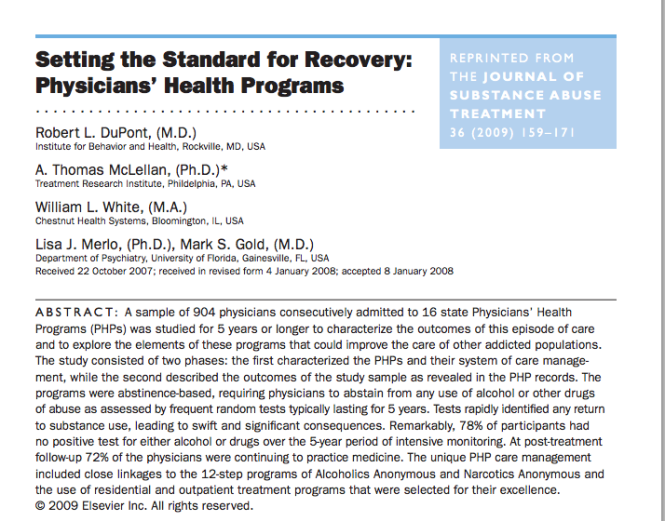
2. Setting the Standard for Recovery: Physicians’ Health Programs
Physician Health Programs (PHP) claimed “gold standard” for addiction treatment. “80% success rate” being used to promote “new paradigm” to other populations.
PHPs are essentially Employee Assistance Programs (EAPs) for doctors. The vast majority of people know little or nothing about Physician Health Programs (PHPs).
Physician Health Programs (PHPs) are being called the “gold-standard” for EAPs. Claims of unparalleled success are being used to promote PHPs to other populations as a “replicable model of recovery.”
Drs. Robert Dupont and Gregory Skipper are promoting PHPs as “A New Paradigm for Long-Term Recovery” claiming an 80% success rate in doctors.
An article entitled “What Might Have Saved Philip Seymour Hoffman,” claims PHPs “ought to be considered models for our citizenry” and the “best evidence-based addiction treatment system we have going.” The author repeats the 80% success rate for doctors and claims Philip Seymour Hoffman might still be alive if he had been treated using the PHP model.
The basis for these claims is a 2009 study published in the Journal of Substance Abuse Treatment entitled Setting the Standard for Recovery: Physicians’ Health Programs and authored by Robert Dupont, A. Thomas McLellan, William White, Lisa Merlo and Mark Gold.
This study is the cornerstone of the “PHP-blueprint.” It is the very foundation on which everything else is based, a Magnum opus used to lay claim to supremacy that has been endlessly repeated and rehashed in a plethora of self-promotion and treatment community blandishment.
To date there has been no academic analysis of the “PHP-Blueprint.” There has been no Cochrane type analysis or critical review. There has been no opposition to its findings or conclusions which are paraded as fact and truth without challenge or question and there is a general lack of concern from those both within and outside the medical profession.
The Expansion of Physician Health Programs (PHPs) to Other Populations
1. Although these programs claim to help doctors they may actually be harming many and contributing to suicide.
2. The plan is to greatly expand these programs to other populations and you could be next.
In 2012 Robert Dupont delivered the keynote speech at the Drug and Alcohol Testing Industry Association annual conference and described a “new paradigm” for addiction and substance abuse treatment and proposed expansion of this paradigm to other populations including workplace, healthcare, and schools.
It is therefore critical that the “PHP-blueprint” be examined using critical reasoning and evidence base. All of this needs to be assessed in terms of legitimacy and intent.
Lack of Evidence-Base and Conflicts of Interest
A cursory analysis of the study on which this success rate is based reveals very little evidence base.
The claim of 80% success rate in physicians is based on Setting the Standard for Recovery: Physicians’ Health Programs is unfounded. The study is a poorly designed using a single data set (a sample of 904 physician patients consecutively admitted to 16 state PHP’s).
It is non-randomized and non-blinded rendering the evidence for effectiveness of the PHP treatment model over any other treatment model (including no treatment) poor from a scientific perspective. The study contains multiple flaws in both reasoning (type I and type II errors) and statistical analysis that render its conclusions invalid.
In addition the impact of undeclared but substantial financial conflicts-of-interest (including funding by drug testing and addiction treatment industries) and personal ideological biases (including personal 12-step recovery from addictions) in the authors of this study also needs to be considered.
Moreover the misdiagnosis and over-diagnosis of addiction in physicians in this paradigm incentivized by lucrative self-referral dollars for expensive 90-day treatment programs is a significant factor.
False Endpoints and High Mortality Rate
The mean age of the 904 physicians was 44.1 years. They report that 24 of 102 physicians were transferred and lost to follow “left care with no apparent referral.”
What happened to them? These are physicians with multiple identifiers (state license, DEA, UPIN, etc) not transient drifters.
Of the 802 left in the program they report 155 failed to complete the contract. Of these, 48 involuntarily stopped or had their license revoked and 22 died with 6 of those being suicides. This study is looking at defined endpoints while being monitored so 6 killed themselves while being actively monitored by the program. But what about the 24 that left with no apparent referral? It is unlikely the just left on a whim. There must have been some precipitant event.
More importantly what happened to those 48 who were reported to the Medical Board for noncompliance and had their licenses revoked–that would be the critical time when this population would be at most risk for completing a suicide. That would be when hope was lost and the coerced physician, knowing that the fight was over, would take that step.
The outcomes they used were the last reported status of the PHP participant enrolled in the program. Measuring success of program completion in doctors compared to the general population is meaningless as the short-term outcomes are quite different in terms of the external consequences imposed. The consequence of not completing a PHP is the invariably career ending. So what happened to the 24 of who “left care with no apparent referral,” the 85 who “voluntarily stopped or retired,” and the 48 who “involuntarily stopped or license revoked.”
Whether you leave a PHP voluntarily, involuntarily, or with no apparent referral it is the end game and your career is over. Comparing this to other populations where the consequences of failing to complete the program are not so final is inappropriate. Claiming superiority over programs with a 40% success rate is unfounded because for most of those people the consequences are not so final and may mean nothing more than an increase in testing frequency.
The big question is what happened to the 157 physicians who left or stopped? How many of them killed themselves. With an average age of 44 there were 6 reported suicides 22 deaths, and another 157 no longer doctors. I would venture to say the number of suicides is a lot higher than they claim. But using the last recorded PHP status as the final outcome obfuscates this.
Due to the severity of the consequences a 20% failure rate is quite concerning. This is of particular concern because many doctors (if not most) monitored by PHPs are not addicts.
Imposed 12-step ideology and use of non-FDA Approved Drug and Alcohol Testing
As noted above, PHPs are essentially Employee Assistance Programs (EAPs) for doctors. Most EAPs, however, were developed in the presence of trade unions and other organizations working on behalf of the best interests of the employee. This collaborative effort led to EAPs that were more or less “organizationally just” with procedural fairness and transparency.
No such organizations exist for doctors. Due to the absence of oversight and accountability PHPs have been able to use non-FDA approved laboratory developed tests of unknown validity on doctors without any opposition.
The distinction between professional and private life as a fundamental value of our society and the importance of this boundary was also upheld by these groups.
In the PHP paradigm no procedural fairness or transparency exists and the boundary between professional and private life has eroded.
PHPs impose 12-step ideology on all doctors referred to these programs. State Medical Boards enforce this in violation of the Establishment Clause of the 1st Amendment yet there is little recourse for doctors as they are threatened with non-compliance and loss of licensure.
Selling the PHP Paradigm
The use of 12-step is most likely not ideologically driven but profit driven. Abstinence based 12-step programs justify the use of frequent drug and alcohol testing with ongoing lifelong assessment and treatment. As with drug-courts, PHPs provide a lucrative model to the drug and alcohol testing, assessment and treatment industry.
The plan to expand this to other populations is outlined in the ASAM White Paper.
This concerns all of us. The first step needs to be a critical appraisal of Setting the Standard for Recovery: Physicians’ Health Programs, the foundation of their claims of an 80% success rate and a conflict-of-interest analysis of its authors. The legitimacy of the study and its claims needs to be questioned.
It does not take a Cochrane review to see that the emperor has no clothes. This is not difficult. It is straightforward and simple.
 As an illegitimate and irrational authority it is necessary that this opinion remain unchallenged. We need to challenge it.
As an illegitimate and irrational authority it is necessary that this opinion remain unchallenged. We need to challenge it.
Historical, political, economic and social analysis reveals that the “PHP-blueprint” is a false-construct built on circumnavigation and obfuscation. An evidence-based scrutiny of the literature would reveal it to be invalid and of little probative value.
But if nobody speaks up it is inevitable that they will expand the “PHP blueprint” to other employee assistance programs and schools.
This is not just about doctors. You too are at risk for coercion, control, conformity and forced adherence to a lifetime of abstinence and 12-step indoctrination and if you do not speak up now it won’t be a risk but a certainty.
American Medical Association (AMA) Seeks to Test Older Physicians: The Aging Physician–Goodbye Dr. Welby!
The AMA is seeking to test older physicians. This is no doubt due to the influence and lobbying of the “impaired physicians movement” and the “addiction medicine” specialists who brought us the “impaired” and “disruptive” physician constructs. As do all groups of this ilk, they want to expand. It is predictable and that is what we are seeing here.
Originally posted on Disrupted Physician:
The Aging Physician—Goodbye Dr. Welby!

As a specialist in geriatric medicine I have experience in taking care of a number of doctors who were referred to me for suspected memory problems. Still operating and teaching residents in his 70s, my first was a well-respected surgeon, a pioneer or Maverick who had made advances in his particular subspecialty. Known for his detailed knowledge of the history of medicine and sharp clinical acumen, he had not seemed himself for a while. His colleagues noted he appeared slower, fatigued and forgetful at times (not remembering his keys, having trouble finding the right word). An internist friend and co-worker who knew him for 50 years curb-sided me and asked if I would see him. He did not have a primary care physician or even seen a doctor professionally for decades (a common phenomenon in this age cohort of doctors).
I met him the next week and he readily admitted to having difficulty concentrating and having trouble with his short term memory. On taking his history he told me of his life and career which started as an intern in Boston in 1942 and he was on duty the night 492 people were killed in the Cocoanut Grove fire with many of the victims transported to his hospital. “I can see every detail as if it were yesterday–beautiful young women wearing fashionable dresses and gowns and young men in formal evening wear who looked as if they were sleeping but were dead.”
“Gastric reflux ” was the only medical problem he reported, adding it was well controlled for the better part of a decade with anti-reflux medications from the office sample closet. I tested his memory with several cognitive scales which showed some mild deficits in short-term memory and sent him to a neuropsychologist for more comprehensive testing. His physical examination, including a comprehensive neurological exam was normal. I ordered the usual lab work up for dementia to look for possible metabolic causes and his B12 level returned markedly low–a result of his long-term use of proton pump inhibitors. He was given an intramuscular injection and started on high doses of oral B12. As one of the “reversible’ causes of dementia he was back to his usual sprightly self several months later.
Another, a 70 old psychiatrist still teaching medical students and residents had asked a third-year psychiatric resident out on a date on two separate occasions. She reported him to administration on the second request. When I asked him about the incident he replied he didn’t see what was wrong with what he did and it was being blown out of proportion. “She’s in her 20’s” I said to which he replied “Well I’m only 36.” Still giving lectures to first year medical students without error or pause from knowledge he learned long ago, he could not identify a pencil or a watch when I pointed to them and asked what there were. He knew neither the month, season or year. After an MRI and neuropsychological testing he was given a diagnosis of probable Alzheimers disease. He had no spouse or children and his work was his life. After that he became profoundly depressed and six months later was dead.
Another elderly doctor, an internist, had a fairly sudden sudden onset of memory problems and symptoms of delirium. It turned out he was having trouble sleeping and his cardiologist prescribed him Dalmane, a benzodiazepine similar to Valium (medications that have a whole host of adverse effects in older patients including memory problems and falls). But valium has a half-life of hours whereas Dalmane has a half life of days. The medication was stopped and he was back to normal after a few days.
Aging is associated with an increased decline in many areas including cognition, motor-skills, muscle strength, and vision that can individually or cumulatively create risk to the person or others in a variety of situations (driving, living situation, occupation).
With advancing age comes advancing risk and the recognition and vigilance of others is often necessary for intervention. If the risk is recognized the problem can be addressed by the appropriate healthcare providers and specialists.
Doctors are not immune from cognitive impairment or dementia and the perspicacity of others is necessary should this occur.
Recognition and awareness are important. So too is an assessment by a qualified physician Board Certified in Neurology, Geriatrics or Geriatric Psychiatry who has education and experience in the diagnosis and treatment of memory disorders.
Recognition, Insight and Education Essential
In 2009 Dr. Ralph Blasier, M.D, J.D., published an article in the Journal Clinical Orthopaedics and Related Research entitled “The Problem of the Aging Surgeon: When Surgeon Age Becomes a Surgical Risk Factor” discussing the ability of older physicians to practice medicine safely and effectively.
His primary message is that a decline in physical and cognitive abilities is associated with the aging process and that these issues are especially pertinent to the field of medicine.
An area little researched, Blasier gives anecdotal examples such as a surgeon in his late 80s who had to regularly depend on younger colleagues to finish his operations. He concludes that these anecdotal examples suggest many surgeons lack insight into the degradation of their own skills and suggests recognition, insight, and education can help facilitate retirement of the aging surgeon before a decline in competency and skill creates a problem.
The awareness, education and insight of others is necessary to identify age associated illness in doctors who can then be referred to the proper specialists for evaluation. And although no evidence base exists, anecdotal reports such as these caused some groups to see an opportunity to increase the grand scale of the hunt.
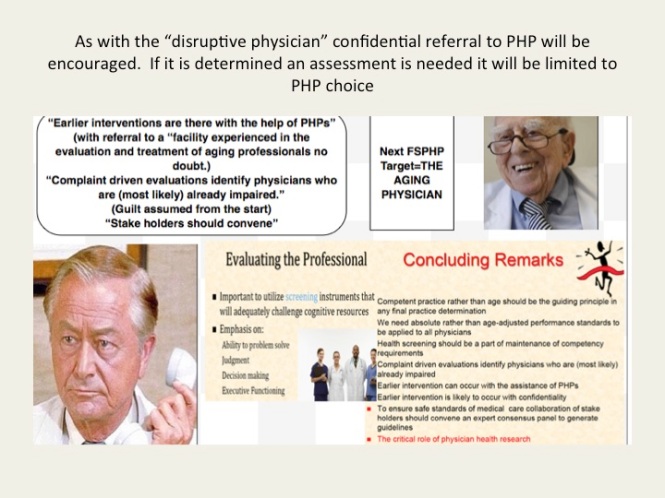
Aging Physicians Next Target of Physician Health Programs
As with the “impaired” and “disruptive” physician, the “physician health and wellness movement” organized as the Federation of State Physician Health Programs (FSPHP) is linking the “aging” physician with threats to patient safety and hospital liability. “Experts say doing nothing could result in lawsuits, higher liability insurance rates, ruined reputations for practices and all involved, and even possible losses of practices and the licenses of non-reporting physicians.”
And if you look at the articles and presentations aimed at the administrative, regulatory, and legal arenas of medicine it appears a new moral panic is percolating in the “physician wellness” cauldron.
Labelling a group dangerous and creating fear in those responsible for that group is an effective means to sway policy and opinion.
With absolutely no evidence base these groups have acted as “moral entrepreneurs ” and used this same methodology to successfully change policy and regulation in the medical profession and advance their goals. The methodology is to
1. Label a group and link that group to danger
2. Offer to assist in identifying and eliminating that danger
3. Corner the market and control all aspects including assessment, testing and monitoring by swaying those in authority to make it public policy and regulation. 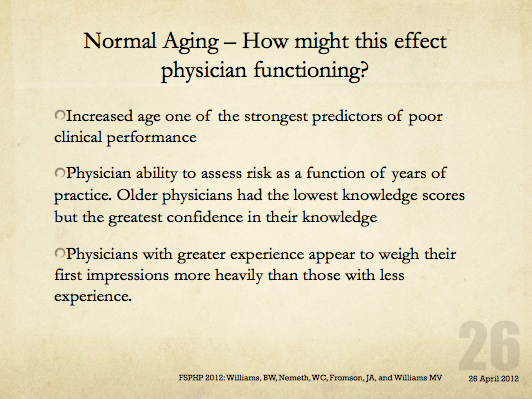
The methodology is not new–witches are real, witches are dangerous and witches need to be identified and exterminated at all costs. Convince the authorities to assist you in protecting the public from harm and advance the greater good
In this manner the FSPHP has convinced state medical boards to adopt and enforce policies that have incrementally and systematically increased their autonomy, scope and power since they first cultivated a relationship with the Federation of State Medical Boards (FSMB). This occurred in 1995 when they took an uninvited seat at the table of power by offering a non-disciplinary “safe harbor” as an alternative to discipline for doctors impaired by drugs or alcohol.
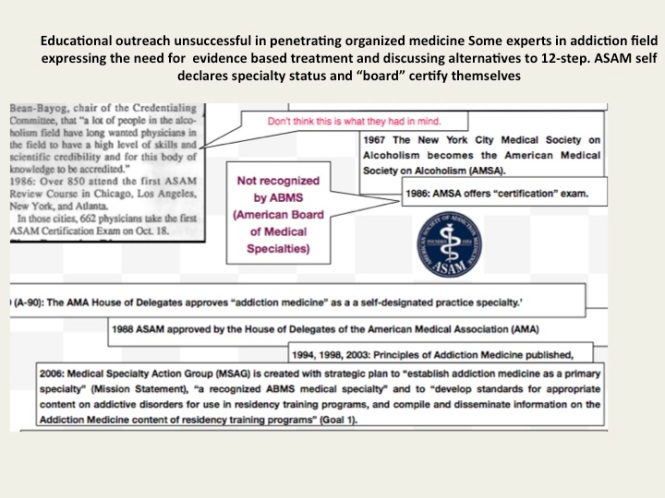
Since then they have increased their scope from the “impaired” to the “disruptive” to everything else. Arising from the “impaired physicians movement” as “addiction specialists” these doctors whose specialty of addiction is not even recognized by the American Board of Medical Specialties have now become the “experts” in all matters related to physician health. Jacks of all trades covering neurology, psychiatry, geriatrics, and occupational medicine.
A 2011 updated FSMB Policy on Physician Impairment states that Medical Boards should recognize the state Physician Heath Program (PHP) as their experts in all matters relating to licensed professionals with “potentially impairing illness,” and these include those potentially impairing maladies that increase as we age.
They are also using “everyone else does it why don’t we?” logical fallacy. According to a Washington Post article “other professions are subject to age-related regulations. For example, airline pilots must undergo regular health screenings staring at age 40 and must retire at age 65. FBI agents must retire at age 57.”
Proposing drug testing in doctors a JAMA article uses this same logic stating when sentinel events occur in the airline, nuclear power and railway industry the get drug tested. However all of these industries use FDA approved tests, certified labs, strict chain-of-custody and MRO review in their drug testing. One of the authors of the JAMA paper, Dr. Greg Skipper, introduced the non-FDA approved and unvalidated Laboratory Developed Tests currently used in PHPs such as EtG. He claims no conflicts-of-interest. Comparing drug testing to industries that use the highest quality of testing and safeguards to protect the donor from false-positives to the junk science used in PHPs is comparing apples to oranges. Which one do you think they’s be using in the random drug testing of doctors?
Furthermore, airline pilots, railway engineers and nuclear power plant employees have a choice of assessment and treatment centers should they get a positive test. Doctors do not. They are mandated to “PHP-approved” facilities. This is enforced by state medical boards as they adhere to an ASAM Public Policy Statement recommending only “PHP approved” treatment centers be used for assessment and treatment and a recent audit found the PHP in North Carolina could not provide any measurable indices or qualitative indicators of how an assessment center is stamped “approved.” The best they could come up with is “reputation” and other ‘informal sources. What the audit missed is all of the 19 out-of-state “PHP-approved” centers Medical Directors can be found on this list.
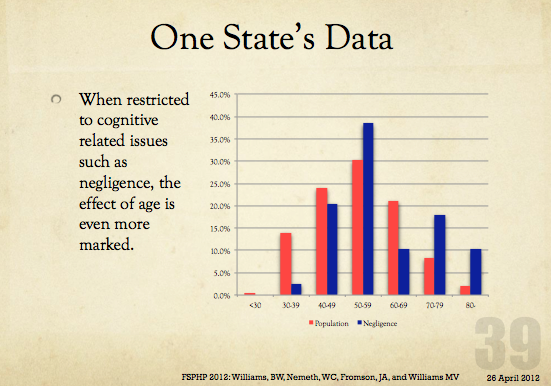
And what will happen with the “aging physician” is the same. Doctors will be forced into “assessments” at “PHP-approved” facilities where they will be misdiagnosed, over-diagnosed and forced into monitoring contracts under threat of loss of licensure. Goodbye Dr. Welby!


The “Impaired Physician Movement” takeover of state Physician Health Programs (PHPs).
“The impaired physician movement is characterized by a number of evangelical recovered alcoholic and addict physicians, whose recovery has been accompanied by an involvement in medical society and treatment programs. Their ability to make authoritative pronouncements on physician impairment is based on their own claim to insider’s knowledge.”–G.V. Stimson (1)
Forget what you see; Some things they just change invisibly–Elliott Smith (Between the Bars)
Physician Impairment
The Sick Physician: Impairment by Psychiatric Disorders, Including Alcoholism and Drug Dependence, published by the American Medical Association’s (AMA) Council on Mental Health in The Journal of the American Medical Association in 1973, (2) recommended that physicians do a better job of helping colleagues impaired by mental illness, alcoholism or drug dependence. The AMA defined an “impaired physician” as “a physician who is unable to practice medicine with reasonable skill and safety to patients because of mental illness or excessive use or abuse of drugs, including alcohol.”
Recognition of physician impairment in the 1970s by both the medical community and the general public led to the development of “impaired physician” programs with the purpose of both helping impaired doctors and protecting the public from them.
 The 1975 media coverage of the deaths of Drs. Stewart and Cyril Marcus brought the problem of impaired physicians into the public eye.
The 1975 media coverage of the deaths of Drs. Stewart and Cyril Marcus brought the problem of impaired physicians into the public eye.  Leading experts in the field of Infertility Medicine, the twin gynecologists were found dead in their Upper East Side apartment from drug withdrawal that New York Hospital was aware of but did nothing about. Performing surgery with trembling hands and barely able to stand, an investigation revealed that nothing had been done to help the Marcus brothers with their addiction or protect patients. They were 45 –years old.
Leading experts in the field of Infertility Medicine, the twin gynecologists were found dead in their Upper East Side apartment from drug withdrawal that New York Hospital was aware of but did nothing about. Performing surgery with trembling hands and barely able to stand, an investigation revealed that nothing had been done to help the Marcus brothers with their addiction or protect patients. They were 45 –years old.
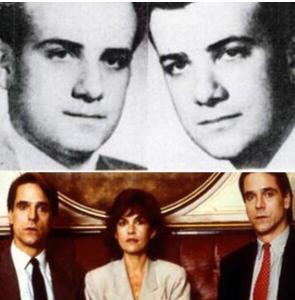
Top: Twin Gynecologists Stewart and Cyril Marcus
Bottom: The Movie “Dead Ringers” starring Jeremy Irons based on the Marcus twins
Although the New York State Medical Society had set up its own voluntary program for impaired physicians three years earlier, the Marcus case prompted the state legislature to pass a law that doctors had to report any colleague suspected of misconduct to the state medical board and those who didn’t would face misconduct charges themselves.
Physician Health Programs
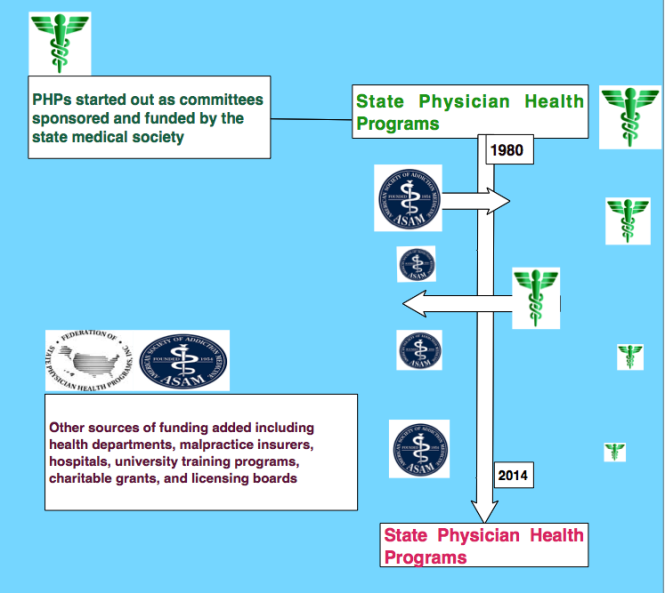
Physician health programs (PHPs) existed in almost every state by 1980. Often staffed by volunteer physicians and funded by State Medical Societies, these programs served the dual purpose of helping sick colleagues and protecting the public. Preferring rehabilitation to probation or license revocation so long as the public was protected from imminent danger, most medical boards accepted the concept with support and referral.
As an alternative to discipline the introduction of PHPs created a perception of medical boards as “enforcers” whose job was to sanction and discipline whereas PHPs were perceived as “rehabilitators” whose job was to help sick physicians recover. One of many false dichotomies this group uses and it is perhaps this perceived benevolence that created an absence of the need to guard.
Employee Assistance Programs for Doctors
Physician Health Programs (PHPs) are the equivalent of Employee Assistance Programs (EAPs) for other occupations. PHPs meet with, assess, and monitor doctors who have been referred to them for substance use or other mental or behavioral health problems.
Most EAPs, however, were developed with the collaboration of workers unions or some other group supporting the rights and best interests of the employees. PHPs were created and evolved without any oversight or regulation.
The American Society of Addiction Medicine can trace its roots to the 1954 founding of theNew York City Medical Society on Alcoholism (NYCMSA) by Ruth Fox, M.D whose husband died from alcoholism.
The society, numbering about 100 members, established itself as a national organization in1967, the American Medical Society on Alcoholism (AMSA).
By 1970 membership was nearly 500.
In 1973 AMSA became a component of the National Council on Alcoholism (NCA) in a medical advisory capacity until 1983.
But by the mid 1980’s ASAM’s membership became so large that they no longer needed to remain under the NCADD umbrella.
In 1985 ASAM’s first certification exam was announced. According to Dr. Bean-Bayog, chair of the Credentialing Committee, “a lot of people in the alcoholism field have long wanted physicians in the field to have a high level of skills and scientific credibility and for this body of knowledge to be accredited” (3). And in 1986 662 physicians took the first ASAM Certification Exam.
By 1988 membership was over 2,800 with 1,275 of these physicians “certified” as “having demonstrated knowledge and expertise in alcoholism and other drug dependencies commensurate with the standards set forth by the society.” (4) The formation of State Chapters began with California, Florida, Georgia, and Maryland submitting requests.(5)
In 1988 the AMA House of Delegates voted to admit ASAM to the House. According to ASAM News this “legitimizes the society within the halls of organized medicine. (3)

By 1993 ASAM had a membership of 3,500 with a total of 2,619 certifications in Addiction Medicine. The Membership Campaign Task Force sets a goal to double its membership of 3,500 to 7,000 by the year 2000 to assure “the future of treatment for patients with chemicals. It represents a blueprint for establishing addiction medicine as a viable entity.” (6)
Many of these physicians joined state PHPs and over time have taken over under the umbrella of the FSPHP.
Others became medical directors of treatment centers such as Hazelden, Marworth and Talbott.
1. Stimson GV. Recent developments in professional control: the impaired physician movement in the USA. Sociology of health & illness. Jul 1985;7(2):141-166.
2. The sick physician. Impairment by psychiatric disorders, including alcoholism and drug dependence. JAMA : the journal of the American Medical Association. Feb 5 1973;223(6):684-687.
3. Four Decades of ASAM. ASAM News. March-April 1994, 1994.
4. American Medical Society on Alcoholism & Other Drug Dependencies Newsletter. Vol III. New York, NY: AMSAODD; 1988:12.
5. AMSAODD News. Vol III. New York, NY: American Medical Society on Alcoholism & Other Drug Dependencies; 1988.
6. Membership Campaign Update. ASAM News. Vol VIII: American Society of Addiction Medicine; 1993:11.
The Medical Profession under Dictatorship–Revisiting Dr. Leo Alexander’s prescient warnings from 1949
“Let it be considered, too, that the present inquiry is not concerning a matter of right, if I may say so, but concerning a matter of fact.”–Adam Smith
“Most men endure the sacrifice of the intellect more easily than the sacrifice of their daydreams. They cannot bear that their utopias should run aground on the unalterable necessities of human existence” -Ludwig von Mises
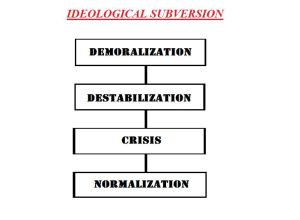
The guiding philosophic principle is Hegelian or “rational utility” and “corresponding doctrine and planning”, Alexander said “replaced moral, ethical and religious values” and Nazi propaganda was highly effective in perverting public opinion and public conscience. He explains how this expressed itself in a rapid decline in standards of professional ethics in the medical profession. This all “started from small beginnings” with subtle shifts in the attitudes of physicians to accept the belief that there is such a thing as “a life not worthy to be lived.”
In 1985 the British Sociologist G.V. Stimson wrote of a new form of professional control in the United States that had emerged in the preceding decade whose “success rests on the ability to take certain areas of conduct such as alcoholism and drug abuse (which are formally disciplinary issues) and handle them as diseases.”2
Stimson writes:
“The impaired physician movement is characterized by a number of evangelical recovered alcoholic and addict physicians, whose recovery has been accompanied by an involvement in medical society and treatment programs. Their ability to make authoritative pronouncements on physician impairment is based on their own claim to insider’s knowledge.”2
Among these authoritative pronouncements was the use of specialized treatment centers. Many professionals were critical of these programs including Assistant Surgeon General John C. Duffy who criticized the “boot-camp mentality”4 toward doctors and American Society of Addiction Medicine President Leclair Bissel who when asked in a 1997 interview when the field began to see physicians as a specialized treatment population replied “when they started making money..” .” 5
Amid reports of abuse, coercion and control in facilities using a doctor’s medical license as “leverage,” the Atlanta Journal Constitution ran a series of reports in 1987 documenting the multiple suicides of health care practitioners at one of these programs (5 while in the facility and at least 20 after discharge).6 Neither these suicides nor a large settlement against the same facility (finding a non-alcoholic doctor was intentionally misdiagnosed as an alcoholic and forced into months of treatment) for fraud, malpractice, and false imprisonment involving intentional misdiagnosis7 generated any interest among the medical community at large.
And by 1995 the door had closed as the Federation of State Physician Health Programs ( FSPHP ) relationship with the Federation of State Medical Boards (FSMB), the national organization responsible for the licensing and discipline of doctors, was forged. A 1995 issue of The Federal Bulletin: The Journal of Medical Licensure and Discipline, contains articles outlining the high success rates of these programs in 8 states with an editorial comment from the FSMB that concludes:
“cooperation and communication between the medical boards and the physician health programs must occur in an effort to protect the public while assisting impaired physicians in their recovery.”8
The Federation of State Medical Boards (FSMB) has approved any and all policy and regulation put forth by the impaired physician movement then organized under the Federation of State Physician Health Programs (FSPHP) with no apparent inquiry or opposition.
In 2003 Dr. Gregory Skipper, one of the key players of the impaired physician movement partnered with NMS labs to develop the alcohol metabolite ethyl-glucuronide (EtG) as a laboratory developed test13 14 he proposed be used as a monitoring tool for covert alcohol use in physicians after a pilot study involving just 14 psychiatric inpatients.15
The policy entrepreneurship this group so effectively uses to advance their goals can be seen in the August 25, 2004 Journal of Medical Licensure and Discipline which contains articles both presenting the problem 11 and providing the solution.11 The EtG was then introduced as an accurate and reliable indicator of covert alcohol use and the impact of this cannot be underestimated as it introduce to the market not only unregulated non FDA approved tests for forensic use but tests reaching further back into history then those used by workplace drug-testing programs.
The limitations of any test needs to be understood both in the forensic and clinical context but there is a lot less flexibility in the forensic context when people’s liberties, freedoms or property rights ( as with a medical license) are in jeopardy.
Sensitivity and specificity need to be carefully considered. The positive predictive value of a test is the true positives over the true positives plus false positives. If you are going to sanction somebody as a result of a single test that test needs to have 100% sensitivity.
When workplace drug testing was introduced debates over both the accuracy and scope of tests occurred. The employees right to privacy and the employers right to have a drug-free workplace were discussed with the general consensus being testing for impairment was a legitimate concern but preservation of private life should remain.
What was done here dissolves both.
PHP programs require abstinence from all substances including alcohol and strict adherence to 12-step doctrine9 yet many of the physicians monitored by them are neither addicts nor alcoholics. Requiring abstinence from drugs and alcohol while using non-FDA approved Laboratory Developed Tests in monitoring programs is a dangerous combination. The suicides reported by the Atlanta Journal Constitution in 1987 were prior to the introduction of these tests. Adding these tests of unknown validity to an already abusive program of coercion and control would only worsen the situation.
I have been hearing of multiple suicides involving both the fear of results and false results. I have also been hearing of doctors who have killed themselves because they were suffering from depression but did not seek help as their fear of being ensnared into the PHP outweighed the need to get help.
Three decades after G.V. Stimson so accurately defined the impaired physician movement the impaired physician movement defines the professional control of medicine.. Their involvement in medical society physician health programs (PHPs) and treatment programs has evolved into absolute control of both. Pronouncements on physician impairment have evolved from insider’s claims to written edict. And their reach has extended from impairment due to drugs and alcohol to “potential impairment” and “relapse without use.” Their reach has extended from drug and alcohol impairment to all other aspects of medicine and the impact has been profound. Medicine has been subordinated to the guiding philosophy of the impaired physician movement and doctors are dying in droves du to institutional injustice.
How does the profession of medicine reconcile the fact that we have allowed an as yet non ABMS recognized “self-certification” specialty full reign over those who are ABMS recognized? How is it that we allow non-FDA approved Laboratory Developed Tests (LDTs) of unknown validity on doctors coerced into state Physician Health Programs (PHPs)? A recent debate in Washington calling for regulation of “clinical” LDTs just took place and the fact that they are being used for “forensic” purposes in doctors is incomprehensible. Has anyone noticed it is the same people introducing the tests who are claiming PHPs are the “gold standard,” trying to push them on other EAPs and calling for more widespread use of these tests?
The use of non-FDA approved Laboratory Developed Tests (LDTs) for drug and alcohol testing is currently limited to PHPs and the criminal justice system. (i.e. monitoring programs in which those doing the testing have power and those being tested have no power). That may soon change. See Drug Testing and the Future of American Drug Policy and The American Society of Addiction Medicine White Paper on Drug Testing describing the plans for widespread expansion of this drug testing to other groups including kids.
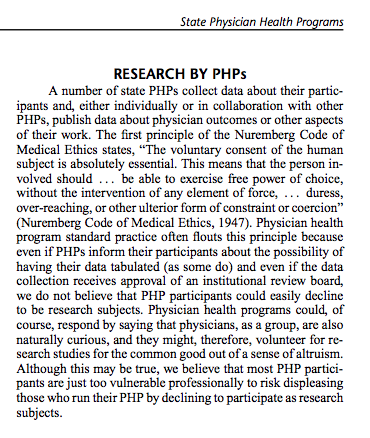
Those involved in the Massachusetts General Hospital Laboratory Medicine, Toxicology and addiction medicine departments looked critically at these tests and decided hands down against using them. Why? Because no evidence base exists and the potential harm far outweighs any perceived benefit. “Research” has been done on those being monitored by PHPs and the criminal justice system and Drs. J Wesley Boyd, M.D., PhD, and John Knight, M.D. of Harvard Medical School who collectively have over two decades of experience as Associate Directors with the Massachusetts PHP, Physician Health Services, Inc. addressed this research in a 2012 article published in the Journal of the American Society of Addiction Medicine entitle Ethical and Managerial Considerations Regarding State Physician Health Programs. The allegations that PHPs are engaging in research in violation of the Nuremberg code ( that was a direct result of the Nuremberg trials for which Dr. Alexander acted as consultant ) should have raised some eyebrows. It hasn’t.
What do you think will happen when ASAM gets recognized by the ABMS in 2 years as is expected? These “addiction medicine” specialists will inevitably join hospital formulary , clinical lab, toxicology and ethics panels to do the same thing they have done to get where they are today. They will do the same thing they have done with state PHPs. Those with a hidden agenda will be able to outvote those of good conscience and thoughtful intelligence and patient care will then be subordinated to the guiding philosophy of the impaired physicians movement.
This system of institutional injustice is killing doctors by suicide as the medical societies and Departments of Public Health have given PHPs full autonomy and authority and it is poised to impact patient care.
I challenge you to name any other company, organization, group or agency within or related to the profession of medicine and the field of science that is bereft of absolutely all transparency, regulation or oversight? It does not exist.
The PHP scaffold has deliberately removed themselves from all aspects of accountability including answerability, justification of actions and the ability of outside actors to hold them in judgment of any information provided by answerability. Heads I win, tails you lose. That is a big red flag in itself. and those not currently being held accountable they may very well be after you next as their plans include expansion to other groups includes EAPs, the Department of Transportation, athletes, students and even kids!
Doctors are afraid to talk about this for fear of being ensnared themselves. Those already in these programs will not speak for fear of punishment. This is a legitimate concern and needs to be discussed openly and publicly. I need allies!
Help me get the word out –too many doctors are dying. Three died by suicide in one month alone who were being monitored by the Oklahoma PHP and these suicides did not even make the local papers let alone national news! They need to.
In The Argument of Fascism Ludwig von Mises wrote:
It cannot be denied that Fascism and similar movements aiming at the establishment of dictatorships are full of the best intentions and that their intervention has, for the moment, saved European civilization. The merit that Fascism has thereby won for itself will live on eternally in history. But though its policy has brought salvation for the moment, it is not of the kind which could promise continued success. Fascism was an emergency makeshift. To view it as something more would be a fatal error.
Making the Data fit the Hypothesis is not Science: The American Society of Addiction Medicine (ASAM), “Weasel Phrases,” “Framing” and “Data-Dredging.”
This is an example of language framing. Language framing uses words and phrases to direct attention to a point of view to advance a vested interest.
In this case the use of the phrase “honest and denial free” in the context of physician reporting imparts associative meaning to the reader.
As denial is a recurring motif and cardinal attribute of physician addiction according to the paradigm, the connotation is that the reports by physicians may have been influenced by dishonesty and denial while face-to-face interviews done by “trained” interviewers were not.
“Framing” is another propaganda technique designed to tell the audience how to interpret the information given through context. The message here is that the somewhat less lifetime prevalence of substance abuse and addiction in physicians found by anonymous mail survey may be underreported as a result of both methodology and denial.
But in actual fact there is a large body of research regarding “social desirability bias” that shows the converse to be true.
 Principles of Addiction Medicine devotes a chapter to Physician Health Programs. Written by Paul Earley, M.D., FASAM,1 Earley states that the lifetime prevalence of substance abuse or addiction in physicians found by Hughes2 is “somewhat less than the percentage in the general population reported by Kessler” of 14.6%.3
Principles of Addiction Medicine devotes a chapter to Physician Health Programs. Written by Paul Earley, M.D., FASAM,1 Earley states that the lifetime prevalence of substance abuse or addiction in physicians found by Hughes2 is “somewhat less than the percentage in the general population reported by Kessler” of 14.6%.3
Although he specifies the numerical percentage “in physicians at 7.9%,”3 he avoids the use of numbers (14.6%) in the general population. He instead uses the qualifier “somewhat less.” Why is this?
My guess is because it understates the statistical fact that the prevalence found by Kessler in the general population was almost twice that found by Hughes in physicians.
You see, “Somewhat less” is a “detensifier.” It creates an impression of a small disparity between doctors and the general population.
In propaganda this is what is known as a “weasel phrase.” Weasel phrases are used to obfuscate the…
View original post 645 more words
In Mechanics and Mentality the Physician Health Program “Blueprint” is Essentially Straight, Inc. for Doctors.
Propaganda and misinformation is designed to sway public opinion and it is all hidden from public view and scrutiny. Absolutely no oversight or regulation from outside agencies exists for Physician or Professionals Health Programs (PHPs) and very little exists for the “PHP-approved” up-front cash only assessment and rehabilitation facilities.
The commercial drug-testing labs using non-FDA approved LDTs have no accountability either. No agencies exist to hold them accountable for errors or even intentional misconduct.
The College of American Pathologists (CAP) is the only avenue for complaint and CAP is an accreditation agency that can only “educate” not “discipline.” It is a system that fosters and fuels misconduct as no consequences exist for wrongdoing and they built it that way.
The American Society of Addiction Medicine erected this scaffold state-by-state. And that is how it must be removed. It is a system of coercion, control and fear. Crimes like the ones being committed here in Massachusetts must be investigated as crimes. The perpetrators must be held accountable.
In 2012 former Nixon Drug Czar Robert Dupont, MD delivered the keynote speech at the Drug and Alcohol Testing Industry Association (DATIA) annual conference and described a “new paradigm” for addiction and substance abuse treatment. He advocated zero tolerance for alcohol and drug use enforced by monitoring with frequent random drug and alcohol tests. Detection of any substances is met with “swift and certain consequences.”
And then he proposed expansion of this paradigm to other populations including workplace, healthcare, and schools.