Physician Health Programs: More Harm Than Good?
State-Based Programs Under Fire
Pauline Anderson
|August 19, 2015
There is growing scrutiny of US physician health programs (PHPs), which are state-based plans for doctors with substance abuse or other mental health problems.
Detractors of the PHP system claim physicians who voluntarily disclose they have mental health or drug problems can be forced into treatment without recourse, face expensive contracts, and are frequently sent out of their home state to receive the prescribed therapy. Some physicians allege that during their interaction with the treatment centers, large amounts of money were demanded up front before any assessment was even conducted.
In addition, critics assert that there is no real oversight and regulation of these programs.
Called by turns coercive, controlling, and secretive, with possible conflicts of interest, some say the PHP experience has led vulnerable physicians to contemplate suicide.
Two states ― North Carolina and Michigan ― have already been asked to step in and investigate many of the issues raised by PHP critics. In North Carolina, the state agreed with many of the concerns raised and recommended “better oversight” by its medical board and society. And in Michigan, litigation in the form of a class action lawsuit has been launched against the Health Professional Recovery Program (HPRP), a program similar to PHPs.
Michael Langan, MD, an internal medicine specialist in Boston, has first-hand experience with a PHP.
Dr Langan was at Massachusetts General and Harvard University in Boston when he approached the Massachusetts state PHP to help him get off an opioid analgesic. He had begun taking the drug to help him sleep after developing shingles and said he spent several months in prescribed PHP treatment after “signing on the dotted line.”
On his first day at the assessment center, Dr Langan said he was asked how he was going to pay $80,000 cash. “This was before they even evaluated me,” he told Medscape Medical News. Subsequently, Dr Langan said he underwent an independent hair and fingernail analysis that turned out to be negative “for all substances of abuse.”
Since then, he has been documenting possible cases of negative interaction with these organizations. The system, he says, leaves physicians “without rights, depersonalized and dehumanized.”
He fears that the role of PHPs has expanded well beyond its original scope, becoming monitoring programs that have the power to refer physicians for evaluation and treatment even on the basis of administrative failings, such as being behind on chart notes, he said.
He has heard reports of “disruptive physicians” being diagnosed with “character defects.” The monitored physician, he added, “is forced to abide by any and all demands of the PHP ― no matter how unreasonable ― under the coloration of medical utility and without any evidentiary standard or right to appeal. Once in, it’s a nightmare.”
Disempowered, Without Recourse
It is estimated that 10% to 12% of physicians will develop a drug or alcohol problem at some point during their careers.
PHPs were initially established to help physicians grappling with a substance abuse or mental health problem and to provide them with access to confidential treatment while avoiding professional investigation and potential disciplinary action.
Often staffed by volunteer physicians and funded by state medical societies, the original intent of these programs was to help health professionals recover while protecting the public from potentially unsafe practitioners.
PHPs assess and monitor the physicians referred to them. In most states, physicians who comply with PHP recommendations can continue to work, provided they undergo regular drug testing and other testing to ensure sobriety.
Some PHPs are run by independent nonprofit corporations, others by state medical societies. Still others receive support from state medical licensing boards. The relationship of each PHP to the state medical board varies. The scope of services offered through PHPs also differs.
Today, such programs exist in every state except California, Nebraska, and Wisconsin and are represented by an umbrella organization known as the Federation of State Physician Health Programs (FSPHP).
According to its mission statement, the FSPHP’s mandate is to “support physician health programs in improving the health of medical professionals, thereby contributing to quality patient care.”
Coercive Process
Concerns about the PHP system have been percolating for a number of years. In 2012, an editorial by J. Wesley Boyd, MD, PhD, Cambridge Health Alliance and Harvard Medical School, and John R Knight, MD, Boston Children’s Hospital and Harvard Medical School, published in the Journal of Addiction Medicine brought many of the issues to the profession’s attention.
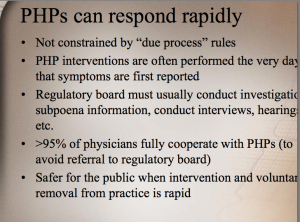
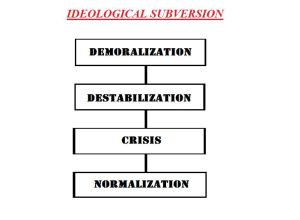
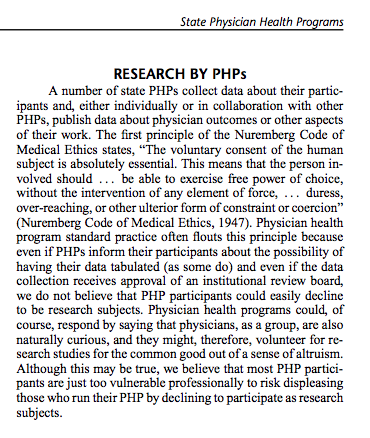
In their editorial, Dr Boyd and Dr Knight alleged that once a mental health issue has been disclosed, doctors are “compelled” to enter a PHP and are instructed to comply with any PHP recommendations or face disciplinary action.
“Thus, for most physicians, participation in a PHP evaluation is coercive, and once a PHP recommends monitoring, physicians have little choice but to cooperate with any and all recommendations, if they wish to continue practicing medicine.”
In an interview with Medscape Medical News, Dr Boyd, who was associate director of the Massachusetts PHP for 6 years, elaborated on what he sees as the lack of due process afforded physicians by such programs.
“In general, these programs are given a free pass because it’s doctors helping doctors, and the feeling is that they wouldn’t be doing that if they weren’t generally nice people concerned about the well-being of others.”
Although many PHPs and the individuals running them are well intentioned, “there are generally few avenues for meaningful appeal” for doctors wishing to dispute PHP treatment recommendations, said Dr Boyd.
Approached on this question, the FSPHP’s director of program operations, Linda Bresnahan, maintains in a written response to Medscape Medical News that “options exist for a physician to seek an additional independent evaluation” and to appeal to the medical board or workplace.
Not so, said Dr Boyd, who counters that physicians have been made to feel “disempowered” and without recourse. “People tend to think that if you raise complaints, you’re just bellyaching and your complaint can’t be legitimate.”
Dr Boyd also said he has heard anecdotal reports of a number of doctors whose interactions with a PHP were so difficult they became suicidal.
“It’s not surprising that if you have your licensing board crawling up your rear end, rates of depression go up and rates of suicide go up,” he said.
Regular Audits in Order?
More and more physicians, even those involved in a PHP, feel that regular monitoring of such programs is in order. For example, Dr Boyd said there should be routine audits “to ensure that rampant abuses of power are not happening.”
Asked whether she believes random audits for state PHPs are warranted, the FSPHP’s Bresnahansaid that the federation “supports quality assurance processes, utilizing both internal and external approaches, and is working to develop guidelines for PHPs to promote accountability, consistency, and excellence.”
Michael Myers, MD, professor of clinical psychiatry, Department of Psychiatry and Behavioral Sciences, SUNY Downstate Medical Center, in New York City, who is on the advisory board of the New York PHP, also favors audits.
Dr Myers has been in practice for 35 years, the last 20 of which have been devoted to caring for physicians and their families. There is no doubt, he told Medscape Medical News, that his state’s PHP program has been “absolutely lifesaving” for some doctors.
However, he acknowledged that there have also been “a lot of unhappy campers” who took issue with the program’s process. At the same time, though, he can recall only one physician who made a formal complaint. Dr Myers noted that the PHP program was initiated on the premise, “if we don’t govern ourselves, then someone else will do it for us.”
“We are trying to have some autonomy, but if a person is unhappy, there isn’t the same mechanism that would exist, say, at a university, where there’s a whole protocol that a professor with a grievance can follow.”
This lack of mechanism for due process was at issue in a recent Michigan class action lawsuit launched by three health care professionals (two registered nurses and one physician assistant), who claim in the statement of complaint to represent the “hundreds, and potentially thousands of licensed health professionals injured by the arbitrary application of summary suspension procedures.”
Although the state program was originally designed to simply monitor the treatment of health professionals recommended by providers, the HPRP has recently “unilaterally expanded its role to include making treatment decisions,” according to the complaints.
They state that “the mandatory requirements of HPRP, coupled with the threat of summary suspension, make involvement in HPRP an involuntary program circumventing the due process rights of licensees referred to the program.”
They also claim the “involuntary” nature of HPRP policies and procedures and the unanimous application of suspension procedures upon HPRP case closure “are clear violations of procedural due process under the Fourteenth Amendment,” the plaintiffs claim.
Initially, the three plaintiffs had their licenses arbitrarily suspended. But in each case, the suspension was promptly overturned by a judge.
For some who have been watching these events, this lawsuit just might be the catalyst to make much needed changes to physician health programs across the country.
“Kafkaesque Nightmare”
Jesse Cavenar, Jr, MD, vice chairman and professor emeritus, Department of Psychiatry, Duke University School of Medicine, Durham, North Carolina, calls the PHP experience a “Kafkaesque nightmare.” Although he himself has not been referred to a PHP, he said a psychiatrist colleague of his, who was anonymously accused of smelling like alcohol, was evaluated and subsequently diagnosed with alcohol abuse.
According to Dr Cavenar, there was nothing to support the diagnosis. The doctor also claimed that the “thorough” physical examination noted in his record was never conducted. In the end, said Dr Cavenar, the psychiatrist was in treatment for 13 months. His medical and legal bills topped $90,000.
Dr Cavenar, who obtained power of attorney in this case, tried but failed to communicate with the treatment facility on behalf of his colleague. He also failed to obtain the medical record.
“When you have a facility that has made a diagnosis and they refuse to talk to anybody about how they made that diagnosis, you say, ‘Something is wrong here.’ ”
During his brush with the PHP system, Dr Cavenar also discovered that at least one evaluation facility has an “understanding” with the referring PHP that a physician will be diagnosed and spend a minimum 90-day interaction period in the treatment facility.
Medscape Medical News spoke to another knowledgeable, highly placed source, who asked not to be identified. He supported Dr Cavenar’s assertion of a mandatory 90-day assessment period, saying he had heard from two other physicians who had undergone treatment in the PHP system that there was in fact such a mandatory period proscribed for them in advance even of an evaluation to determine their level of need.
“I’m no bleeding heart; if you do the crime, you do the time,” said Dr Cavenar. “That’s not what we’re seeing here. We’re seeing people who didn’t do the crime but who are getting tapped with time.”
Bresnahan told Medscape Medical News via email that FSPHP is not aware of a blanket “90-day minimum interaction period” with treatment centers. Rather, among the many treatment centers familiar to PHPs, there are a variety of “programs” within the treatment centers that vary in length, and a variety of programs such as outpatient, intensive outpatient to residential treatment, and variations of residential treatment.
“Treatment centers often offer a 1- to 5-day multidisciplinary evaluation to determine treatment needs, including length of stay and outpatient vs inpatient treatment options. In general, residential treatment centers offer different programming that vary in length of stay from 30-day treatment programs to 45-day treatment programs to 90-day treatment programs.
“Along with these options, PHPs do utilize treatment centers that will provide clients with a variable number of days of treatment. In these examples, the treatment center determines the recommended length of stay during the course of treatment based on clinical needs,” she notes.
Asked about treatment costs to physicians, Bresnahan responded that she is unaware of reports of large lump sums expected on admission.
“FSPHP is unaware of excessive up-front fees in the $80,000 range,” she writes. “It is our understanding that a treatment phase can range from $5000 to $50,000 depending upon the days and the type of programs.
“A number of healthcare professional programs are now having progress with insurance reimbursement to offset portions of the cost,” she adds. “Some offer financial assistance based on a needs assessments, and some may also offer payment plans,” Bresnahan told Medscape Medical News.
Dr Cavenar felt so strongly about his colleague not having due process that he lobbied for an audit of North Carolina’s PHP.
His initial efforts were ignored by the state medical board, he said, so he approached the state governor’s office. Finally, Dr Cavenar said he and three other concerned psychiatrists successfully secured a state audit of North Carolina’s PHP system, the results of which were released in April 2014.
PHP Originator Speaks Out
According to psychiatrist Nicholas Stratas, MD, one of the problems with the North Caroline PHP is that decisions regarding a referred physician are vetted by a legal team.
Dr Stratas has a unique vantage point. He was the originator of the North Carolina PHP, was the first-ever psychiatrist and president of the North Carolina Medical Board, and still holds numerous affiliations with both Duke University and the University of North Carolina.
“In our state, the PHP has turned into something that was never intended…. [It] has become bureaucratized and legalized,” he told Medscape Medical News. “When I was on the board, we had one attorney; now, they must have six or seven attorneys, and the whole job of triaging physicians is left to the legal department.”
Dr Stratas said that at least until the state audit, the North Carolina PHP left physicians with no legal recourse once they were referred to a treatment facility.
“They have taken the position that because they are a peer review mechanism, they don’t have to comply with the nationally recognized condition that everybody should have access to their own records; they will not provide records to the physician.”
Dr Stratas related the case of a psychiatrist who after a detailed assessment was determined to have no addiction or mental health problems. This psychiatrist got caught up in the PHP system after an anonymous caller complained about “weird” behavior, according to Dr Stratas.
On questionable advice from his attorney, the psychiatrist voluntarily suspended his medical licence, thinking it was temporary and would help sort the situation out, but now he cannot get it back until he undergoes “treatment,” said Dr Stratas. After almost 2 years, said Dr Stratas, this psychiatrist is still without his medical licence.
Auditor’s Report: Potential for Undetected Abuse
The state auditor’s report found no abuse by North Carolina’s PHP. However, there was a caveat ― the report determined that abuse could occur and potentially go undetected.
It also found that the North Carolina PHP created the appearance of conflicts of interest by allowing the centers to provide both patient evaluation and treatments and that procedures did not ensure that physicians receive quality evaluations and treatment because the PHP had no documented criteria for selecting treatment centers and did not adequately monitor them.
“Abuse could occur and not be detected…because physicians were not allowed to effectively represent themselves when disputing evaluations… [and because] the North Carolina Medical Board did not periodically evaluate the Program and the North Carolina Medical Society did not provide adequate oversight,” the auditor’s report noted.
The North Carolina PHP “did not use documented criteria to select treatment centers” and “did not conduct periodic evaluation of the treatment centers to ensure compliance with established operating criteria.”
The auditor added that the program’s “predominant” use of out-of-state treatment centers placed an undue burden on physicians.
Furthermore, according to the report, the North Carolina PHP “created the appearance of conflicts of interest by allowing treatment centers that receive Program referrals to fund its retreats, paying scholarships for physicians who could not afford treatment directly to treatment centers, and allowing the center to provide both patient evaluations and treatments.”
The report recommended that physicians have access to “objective independent due process procedures” developed by the state medical board and medical society and that plans be implemented for “better oversight” of the program.
The report also stated that North Carolina’s PHP was required to make it clear that physicians “may choose separate evaluation and treatment providers” and that the PHP undertake efforts to identify qualified in-state treatment centers for physicians.
Since its release almost a year ago, many of these recommendations have been addressed by the North Carolina Medical Board.
“We absolutely embrace the auditor’s recommendations and are working really hard to implement them,” Thom Mansfield, the board’s chief legal counsel, told Medscape Medical News.
North Carolina’s PHP has undertaken to provide periodic reports to the medical board, and an independent audit of the program will be carried out every 3 years, Mansfield added.
Physicians who disagree with their assessment or treatment can now have their case reviewed by a committee independent of the PHP compliance committee and of the medical board, he said.
Mansfield also noted that the state PHP has established criteria for identifying suitable centers to conduct assessments and offer treatment, with an emphasis on developing more in-state resources. “I know the PHP is now referring people to at least two in-state centers,” he said.
In taking these actions, said Mansfield, the North Carolina Medical Board hopes it is “showing leadership” for other states.









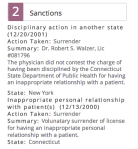

 committee for the first certification exam and ASAM president surrendered her medical license after being accused of sexually abusing one of her patients, a Harvard medical student who subsequently died by suicide.
committee for the first certification exam and ASAM president surrendered her medical license after being accused of sexually abusing one of her patients, a Harvard medical student who subsequently died by suicide.












Hi Mr.Goldsmith,
Currently, these ‘PHP approved evaluation’ centers are the exact same facilities as the PHP ‘treatment’ centers. There centers also have financial relationships with PHP programs and PHP directors.
They charge upwards of $5,000 dollars to the physician plus travel and lodging expenses, because they are often out-of-state.
Former ASAM leader and PHP director Dr.Talbott owned such a facility with a judge as a co-investor. Dr.Talbott was convicted by a jury in a US court of law of coercing a doctor into unnecessary ‘treatment’ for financial gain. How many of these 78% recovery rate come from physicians falsely diagnosed? Dr.Fata, the Michigan doctor convicted of giving false cancer diagnoses, also touted his high ‘treatment success rate’
We’d like you to correct these current questionable practices by ASAM and PHPs. A true independence of diagnosticians and PHPs is a good place to start, with strict oversight and auditing to eliminate all and any financial ties and conflicts of interest. PHP leadership and directors should be replaced by physicians with demonstrated commitment to ethics and personal rights.
Do these steps sound reasonable to you?