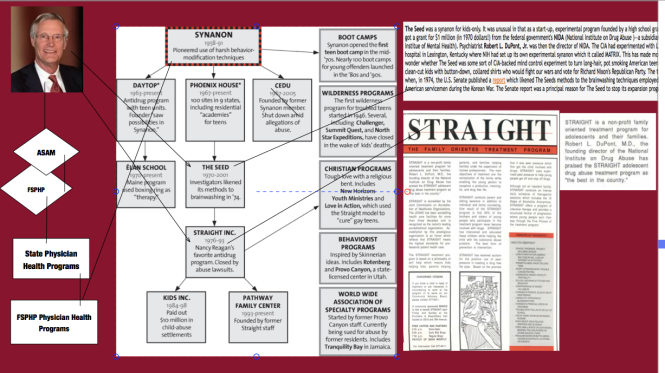
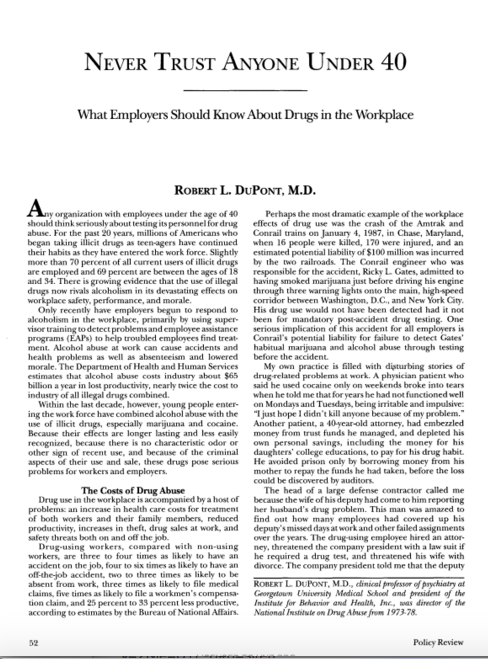
Before the 2012 Drug and Alcohol Testing Industry Association (DATIA) annual conference, Dr. Robert Dupont delivered a speech entitled “Drug Testing and the Future of American Drug Policy.” He describes a “New Paradigm” for substance abuse treatment that enforces “zero tolerance for alcohol and drug use” enforced by monitoring with frequent random drug and alcohol tests in which any positive test is “met with swift, certain” consequences.” The paradigm is based on the current Physician Health Programs blueprint. Dupont states:
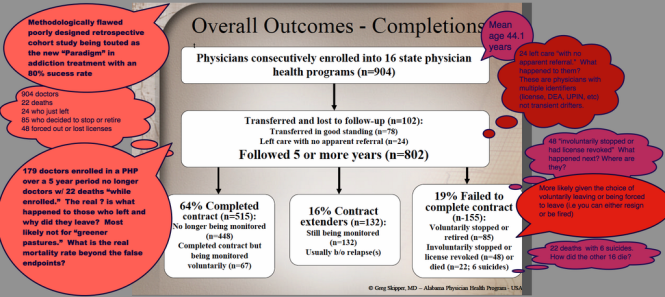
“…physician health programs , have set the standard for effective use of drug testing. These pioneering state programs provide services to health care professionals with substance use disorders. The programs are run by physicians, some of whom in recovery themselves. PHPs feature relatively brief but highly focused treatment followed by active lifelong participation in the 12-step fellowships of Alcoholics Anonymous and Narcotics Anonymous. The key to the success of the PHP system of care management is the enforcement of the standard of zero tolerance for any alcohol or other drug use by intensive long-term random testing for both alcohol and drugs with swift and certain consequences for even a single use of alcohol or any other drugs of abuse. PHPs use drug panels of 20 or more drugs. The PHPs commonly use EtG and EtS tests to detect recent alcohol use. Similar comprehensive programs have been developed for commercial pilots and attorneys. These innovative programs of care management produce unprecedented long-term, outcomes.”
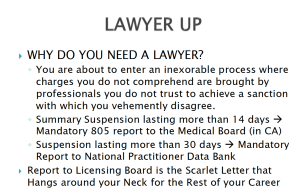
Physician Health Programs use a doctor’s medical license as “leverage” in what they call “contingency management.” What this means is that a doctor who is being monitored by a PHP must comply with any and all demands of the PHP under threat of being reported to the state Medical Board and immediate suspension of licensure. Dupont wants to extend this model to other populations including our elderly, our pregnant mothers, college and high school students and schoolchildren.
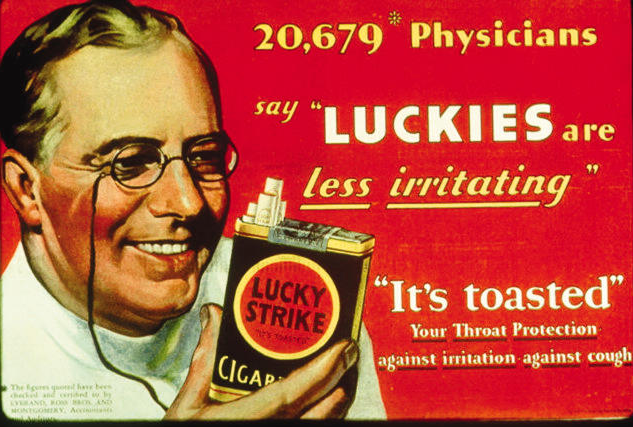
The 2013 American Society of Addiction Medicine White Paper on Drug Testing describes the organizational structure of the “New Paradigm” and this includes utilizing the medical profession as a urine collection agency for their drug and alcohol testing and the loophole they plan to exploit is this: When a doctor-patient relationship exists drug and alcohol testing is rendered “clinical” rather than “forensic”so the consequences of a positive test can legitimately be called “treatment” rather than punishment. Because addiction is currently defined as a disease, addicts must be “treated” (which in the United States is more often coercive than voluntary), and “cured” (which is defined as remaining abstinent). When the disease concept is not strictly reserved for medical conditions but is expanded to any and all drug and alcohol use.
The proposed system bypasses the strict chain-of-custody and Medical Review Officer requirements designed to ensure accuracy and minimize false-positives. These strict protocols are used by essentially all employee assistance programs (EAPs) in workplace drug testing programs. Forensic drug testing is tightly regulated because the results of a positive test can be grave and far reaching and erroneous results are unacceptable.
THE ASAM PAPER DESCRIBES MANDATED DRUG-TESTING FOR PATIENTS IN A NUMBER OF SPECIALTIES INCLUDING ADOLESCENT MEDICINE, PSYCHIATRY, OBSTETRICS, AND GERIATRICS. CONTINGENCY MANAGEMENT WILL INVOLVE “THE POTENTIAL FOR LOSS OF CURRENT OR DESIRED EMPLOYMENT, OR THREATENED LOSS OF OR RESTRICTIONS ON A PROFESSIONAL OR COMMERCIAL LICENSE, OR LEGAL AND FORENSIC NECESSITY.”
“THIS WHITE PAPER ENCOURAGES WIDER AND “SMARTER” USE OF DRUG TESTING WITHIN THE PRACTICE OF MEDICINE AND, BEYOND THAT,BROADLY WITHIN AMERICAN SOCIETY. SMARTER DRUG TESTING MEANS INCREASED USE OF RANDOM TESTING* RATHER THAN THE MORE COMMON SCHEDULED TESTING,* AND IT MEANS TESTING NOT ONLY URINE BUT ALSO OTHER MATRICES SUCH AS BLOOD, ORAL FLUID (SALIVA), HAIR, NAILS, SWEAT AND BREATH WHEN THOSE MATRICES MATCH THE INTENDED ASSESSMENT PROCESS. IN ADDITION, SMARTER TESTING MEANS TESTING BASED UPON CLINICAL INDICATION FOR A BROAD AND ROTATING PANEL OF DRUGS RATHER THAN ONLY TESTING FOR THE TRADITIONAL FIVE-DRUG PANEL.”
Federal workplace drug testing is done in accordance with mandatory guidelines. This testing is regulated using FDA approved tests with established sensitivity, specificity and cutoff levels. FDA approval requires rigorous research and proven validity. The FDA requires valid scientific evidence (with both clinical and analytical validation).
The Federation of State Physician Health Programs (FSPHP), the group currently in managerial control of state physician health programs in 47-states, has introduced non-FDA drug testing via a loophole that removes all accountability. The EtG, EtS, and PEth tests were introduced as Laboratory Developed Tests (LDTs) with little to no evidence base through pathway developed for “clinical” tests of low market potential that would not otherwise be developed due to the prohibitive cost of the FDA approval process. An LDT does not even require testing in humans (“in vivo”) or even proof that the test is testing what it claims to be testing (validity) for. It is an honor system and without FDA oversight a lab can can claim anything they want about these tests with no accountability. They do not have to provide any proof of what they claim or justify what they claim. After partnering with labs to develop these tests, the FSPHP then convinced the Federation of State Medical Boards they were valid and accurate tests that were necessary to detect a bogus cadre of drunk and drugged doctors able to hide their impairment and who were protected by a “code of silence.” This bogus danger was then used to convince state Medical Boards to use these unvalidated tests on doctors in state physician health programs.
(Source: ASAM Physician Health News March 2015)ASAM Physician Health News March 2015)
The ASAM white paper contains the following quote minimizing the critical role of the MRO in drug testing. They feel clinical testing is good enough.
Unlike forensic drug testing where the test results must be able to meet rules of evidence in administrative, civil or criminal proceedings, clinical drug testing* is part of a patient examination performed by a clinician with whom the patient is in a therapeutic relationship. The testing is used for the purposes of diagnosis, treatment, and the promotion of long-term recovery. Clinical drug test results must meet the established standards of medical practice and benefit the therapeutic relationship, rather than meeting the formal legal requirements of forensic testing. Drug testing in medicine employs the same sound procedures, safeguards, and systems of information management that are used for all other health-related laboratory tests, tests on which life-and death medical decisions are commonly made.
Changing Public Policy and Regulatory Authority to Increase Power and avoid Accountability
The Federation of State Physician Health Programs has been able to construct this scaffold with no meaningful opposition and below the public radar. They have done this by removing accountability at multiple levels. By preventing access to information and erecting a system without oversight no consequences exist to deter misconduct and abuse. The same tactics and strategies will be used as they expand this to other populations.
The Federation of State Physician Health Programs trumpets the the 12-step chronic relapsing brain disease model of addiction as defined by A.A. because it supports the drug and alcohol assessment, testing and treatment industries goals of more and more testing and treatment. For example a 2011 FSMB Policy on Physician Impairment identifies, defines and essentially legitimizes “potential impairment” and “relapse without use.”
A PHP Should be empowered to conduct an intervention based on clinical reasons suggestive of potential impairment. Unlike the Board which must build a case capable of withstanding legal challenge, a PHP can quickly intervene based on reasonable concern."
“Empowered” to conduct an “Intervention” for reasons “suggestive” of “potential” impairment means a doctor can be pulled out of practice for anything. It essentially gives them carte blanche authority. Due process and fundamental freedoms of choice are removed.
in 2011 The ASAM issued a Public Policy Statement on coordination between PHPs, regulatory agencies, and treatment providers recommending that only “PHP approved” treatment centers be used in the assessment and treatment of doctors. A recent audit of the North Carolina PHP found financial conflicts of interest and no documented criteria for selecting the out of state treatment centers they used. The common denominator the audit missed was that the 19 “PHP-approved” centers were all ASAM facilities whose medical directors can be seen on this list.
The FSMB House of Delegates adopted an updated Policy on Physician Impairment at their 2011 annual meeting distinguishing “impairment” and “illness” stating that Regulatory Agencies should recognize the PHP as their expert in all matters relating to licensed professionals with “potentially impairing illness.”
According to the FSPHP, physician illness and impairment exist on a continuum with illness typically predating impairment, often by many years.”
The policy extends PHP authority to cover physical illnesses affecting cognitive, motor, or perceptive skills, disruptive physician behavior, and “process addiction” (compulsive gambling, compulsive spending, video gaming, and “workaholism”). It also defines “relapse without use” as “behavior without chemical use that is suggestive of impending relapse.”
G. Douglas Talbott defines “relapse without use” as “emotional behavioral abnormalities” that often precede relapse or “in A A language –stinking thinking.” AA language has entered the Medical Profession and no one seems to have even noticed.
The FSPHP political apparatus exerts a monopoly of force. It selects who will be monitored and dictates every aspect of what that entails. It is a, in fact, a rigged game.
The Need for Regulation, Oversight, and Accountability
Accountability is necessary to prevent corruption and requires both the provision of information and justification for actions. What was done and why? Accountability also necessitates consequences-the ability of outside actors to punish and sanction those who commit the misconduct. Without these constraints corruption is inevitable.
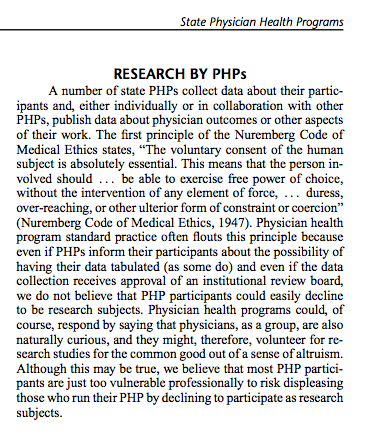
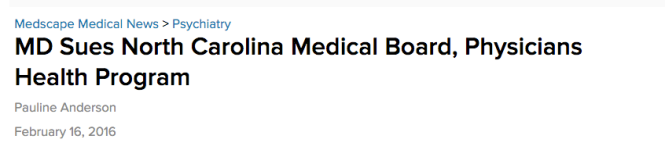
In 2012 Drs. John Knight and Wes Boyd recommended the medical community outside of PHPS provide oversight and demand accountability. In Ethical and Managerial Considerations Regarding State Physician Health Programs they noted the financial conflicts of interest between PHPs and their “approved centers, coercion and abuse and even possible violations of the Nuremberg Code of Medical Ethics yet their paper generated little interest in the medical community. The North Carolina PHP audit revealed financial conflicts-of-interest and no oversight by the state medical society or board and that abuse of doctors could occur undetected due to the complete absence of accountability. State Auditor Beth Woods told the British Medical Journal in a recently published article that the state program had holes in it “big enough to drive a truck through.”
In Ethical and Managerial Considerations Regarding State Physician Health Programs Knight and Boyd state: “Because PHP practices are unknown to most physicians before becoming a client of the PHP, many PHPs operate outside the scrutiny of the medical community at large. Physicians referred to PHPs are often compromised to some degree, have very little power, and are, therefore, not in a position to voice what might be legitimate objections to a PHP’s practices.” And when objections do occur many take the side of the PHP, complacent in their belief that these are just altruistic and competent doctors just helping sick colleagues and protecting the public and valid complaints are deemed nothing more than “bellyaching. In reality the ethical and criminal misconduct occurring in PHPs rivals that of Dr. Farid Fata, the Detroit Oncologist who intentionally misdiagnosed patients with cancer so he could make money off unnecessary chemotherapy treatment. Dr. Fata’s egregious betrayal of trust and unconscionably vile acts resulted in an appropriate response.
 The exact same misconduct is being perpetrated by PHPs but being overlooked, justified or otherwise ignored. Dr. Fata intentionally misdiagnosed patients with cancer who did not have cancer so he could give them chemotherapy to make money. PHPs are intentionally misdiagnosing substance abuse and behavioral disorders in physicians who do not have them in order to give them unneeded treatment and force them into monitoring contracts for profit and control.
The exact same misconduct is being perpetrated by PHPs but being overlooked, justified or otherwise ignored. Dr. Fata intentionally misdiagnosed patients with cancer who did not have cancer so he could give them chemotherapy to make money. PHPs are intentionally misdiagnosing substance abuse and behavioral disorders in physicians who do not have them in order to give them unneeded treatment and force them into monitoring contracts for profit and control.
This undermines the very integrity of the profession. It is particularly vile when the betrayal of trust involves doing the opposite of what was entrusted. Abuse of positions of power, trust and influence in the field of medicine need to be both prevented, recognized and addressed. Oversight, regulation and accountability are essential if this is going to be accomplished. There are no exceptions. Policies and procedures must be enforced in a consistent manner.
The medical boards, medical societies, and departments of health have given the state PHPs carte blanche control and absolute power. They refuse to even investigate accusations and they have convinced law enforcement that this is a parochial matter best handled by within the medical profession. As a result, valid complaints of crimes are not taken seriously. This refusal to investigate or even acknowledge valid and factual complaints of professional misconduct has not only prevented the exposure of wrongdoing and corruption but deepened it. The Federation of State Physician Health Programs and “Like-minded docs” must be recognized for what they are. Front-groups for the drug and alcohol assessment, testing and treatment industry. This is glaringly obvious and you don’t have to look that deep to figure it out. And these are the very same groups being proposed as advocacy bodies for addiction treatment and public policy change. It is not that hard to figure out what they will be advocating for –more diagnoses, more testing and more treatment.
for the drug and alcohol assessment, testing and treatment industry. This is glaringly obvious and you don’t have to look that deep to figure it out. And these are the very same groups being proposed as advocacy bodies for addiction treatment and public policy change. It is not that hard to figure out what they will be advocating for –more diagnoses, more testing and more treatment.

The American philosopher Eric Hoffer noted:
“The only way to predict the future is to have power to shape the future. Those in possession of absolute power can not only prophesy and make their prophecies come true, but they can also lie and make their lies come true.”
The “PHP-blueprint” is built on the very foundation Hoffer describe and unless you want mandated randomized non-FDA approved drug and alcohol testing with “swift and certain” consequences at future visits with your doctor you will need to speak up.
This occurred in the medical profession rapidly and with little notice and that is exactly what will happen here.
“Every time we turn our heads the other way when we see the law flouted, when we tolerate what we know to be wrong, when we close our eyes and ears to the corrupt because we are too busy or too frightened, when we fail to speak up and speak out, we strike a blow against freedom and decency and justice.”








 diagnosis. Pervasive problems include:
diagnosis. Pervasive problems include:
 Creating Bogus Risks of Danger
Creating Bogus Risks of Danger The primary architects of this system can be found on a list of Fellows of the American Society of Addiction Medicine. The list can be seen
The primary architects of this system can be found on a list of Fellows of the American Society of Addiction Medicine. The list can be seen 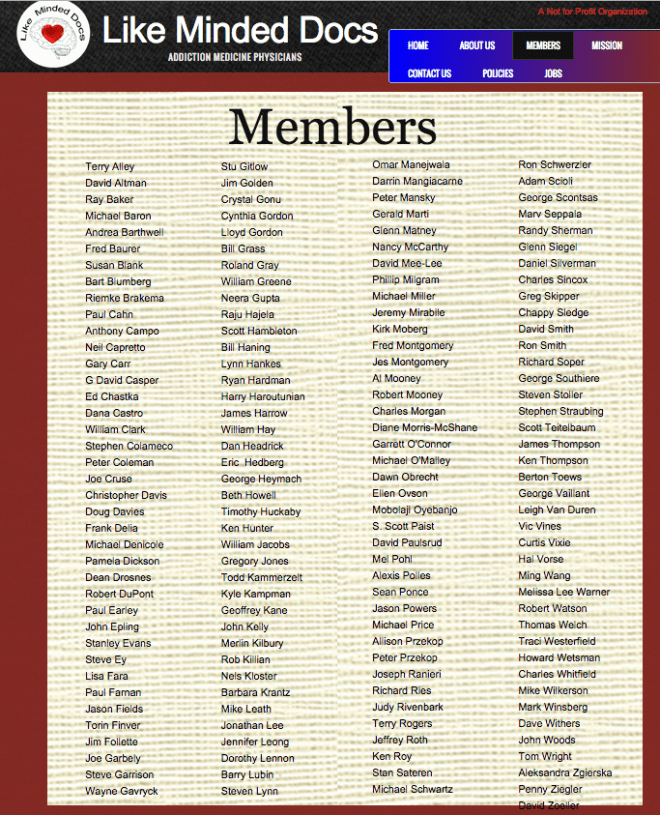




 and alcohol testing labs have no FDA oversight as the tests are non-FDA approved. Other than accreditation agencies such as the College of American Pathologists there is no agency to investigates error or misconduct. CAP cannot sanction. The assessment and treatment centers have little oversight or regulation. In sum this system refuses to provide information and even if they did provide information they do not have to justify it to anyone and no agency exists to punish them even if they could not justify it. Zero accountability.
and alcohol testing labs have no FDA oversight as the tests are non-FDA approved. Other than accreditation agencies such as the College of American Pathologists there is no agency to investigates error or misconduct. CAP cannot sanction. The assessment and treatment centers have little oversight or regulation. In sum this system refuses to provide information and even if they did provide information they do not have to justify it to anyone and no agency exists to punish them even if they could not justify it. Zero accountability. PHCU Board counsel were additionally afforded the power to act as both “hearing-officers” on cases and present these same cases to the Board and recommend disciplinary action. This was by design also.
PHCU Board counsel were additionally afforded the power to act as both “hearing-officers” on cases and present these same cases to the Board and recommend disciplinary action. This was by design also. 












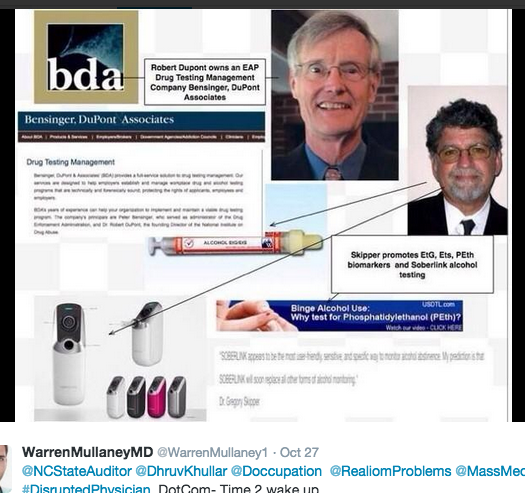
 “In the small world of drug testing, these four—Angarola, Bensinger, DuPont and Willette—are affectionately referred to as the Gang of Four. Dr. John Morgan explains, “They are the ones responsible for a good deal of drug testing’s success, and some of the fear that goes along with it. Remember these names. These men are among the most competent and knowledgeable about drug testing—scientifically and politically. They are well-informed: they have to be. Their livelihoods depend upon their credibility. Unfortunately their expertise represents the greatest threat to the civil liberties we seek to protect. Know your enemy.”
“In the small world of drug testing, these four—Angarola, Bensinger, DuPont and Willette—are affectionately referred to as the Gang of Four. Dr. John Morgan explains, “They are the ones responsible for a good deal of drug testing’s success, and some of the fear that goes along with it. Remember these names. These men are among the most competent and knowledgeable about drug testing—scientifically and politically. They are well-informed: they have to be. Their livelihoods depend upon their credibility. Unfortunately their expertise represents the greatest threat to the civil liberties we seek to protect. Know your enemy.”  On April 23, 2015
On April 23, 2015 






Be the first to comment and start the conversation!