Many say a controversial program designed to help doctors with mental health issues is out of control, destroying careers and causing some doctors to commit suicide.

Author: Investigative Reporter: PJ Randhawa, Erin Richey
Dr. Gary Hammen admits that he was tired on the job.
In 2017, he had a newborn at home and a packed schedule as an anesthesiology resident, on top of a sleep disorder stemming from an injury he got serving our country as a soldier overseas.
But to him, the questions his supervisors asked crossed a line.
“They asked me, is this a drug problem? Are you sure you’re not using drugs?” he recalled. “I was floored.”
The questions came after months of exhaustion for Hammen.
Hammen says repeated, 24-hour shifts were taking their toll on his mental and physical health. Most weeks, he worked more than ninety hours and slept no more than four hours a night.
More than a year earlier, he met with his supervisors to tell them about his sleep disability, and offer them schedule recommendations from his sleep doctor.
He says supervisors promised, but failed to make any accommodation to his schedule or his sleep disability.
Weeks after his supervisors asked him about drugs, he got a call that made him think they didn’t believe him.
An organization called a Missouri Physician’s Health Program wanted him to fly to an addiction recovery center in another state, to be checked out.
Hammen couldn’t believe what was happening. “I had a bad feeling about it,” he said. “The whole thing just felt wrong.”
But he had no choice; colleagues warned him that if he didn’t follow the PHP’s requirements, he could lose his license and his career.
PHPs, or Physician’s Health Programs, are meant to help doctors with addiction or other psychological problems. But some, including Hammen, claim that doctors are sometimes falsely accused and getting help that they don’t need. They say the result drains their savings, endangers their licenses, and has even led some young doctors to take their own lives.
Nearly every state has a PHP. Some states have more than one. They started in the 1980s, often with closeties to the state’s medical boards or hospital associations. Medical industry professionals told 5 On Your Side’s I-Team that now big money is involved, and the lack of regulation turned a well-meaning measure into something that doctors fear even when they need help.
Dr. Wes Boyd of Harvard University is one of the skeptics. He used to work for a state PHP. Now he and others have raised concerns about these programs in the American Medical Association’s Journal of Ethics and in other respected publications.
“The physician is basically at the mercy of the PHP,” said Boyd. “There is no one outside the program looking at them, monitoring their practices and making sure that they’re really acting in a benevolent way.”
Boyd told us that when a PHP gets a tip about a supposed problem doctor, there is usually no way for the physician to appeal or dispute it. Instead, he or she must go to a “preferred” treatment center for evaluation. That center has complete authority to decide which doctors need treatment and how much.
Hammen made the flight to a treatment center, where evaluators made an unusual diagnosis. They said he had “provisional alcohol disorder,” something Hammen never heard of before.
“They hadn’t even talked to my wife to see if I drink. Most people wouldn’t make that sort of diagnosis without talking to some sort of outside person beside the patient,” said Hammen.
That diagnosis, Hammen thought, came from the fact that he told evaluators he and his wife shared a bottle of wine over the course of several dinners that week. It’s the only thing listed in the part of his evaluation describing his alcohol use.
Many of the treatment centers that PHPs refer doctors to are for-profit and specialize in addiction, even though doctors enter PHP monitoring because of stress and depression as well.
The I Team found many of the “preferred” treatment centers also donate money to the PHP trade organization: the Federation of State Physician Health Programs (FSPHP). Newsletters on the FSPHP website show several treatment centers are donors and exhibitors at FSPHP events.
Boyd told the I-Team that the bottom line motivates the centers to push doctors into treatment regardless of whether it’s really needed.
“Even in cases where there was no substance dependence, these centers come back and say, ‘You need to stay for 30 or 90 days of treatment,’” he said. “It is very hard not to think that financial motivations were behind the misdiagnoses.”
That can mean weeks of being unable to work, attending a treatment center that might not even offer services that doctors really need, with no way to get a second opinion or to choose their own care.
Even doctors who need help find the system difficult to navigate, with a high price to them and their community. Karen Miday once hoped that her son would get to help the community as a Cancer Specialist, but now he’ll never get that chance.
The words he left behind in a suicide note are so painful that she never took it out of the police department’s evidence envelope. But she read them to KSDK’s PJ Randhawa to show what he was feeling at the end of his life.
“That ‘I love you’ line stays with me,” she said.
“This is just the end of the line for my particular train,” Dr. Greg Miday wrote. “Earth wasn’t a great place for me.”
Dr. Greg Miday was 29 years old when he finished his residency in St. Louis in 2012. Friends and colleagues described him as bright, talented, and gentle. Under the surface, he also battled a drinking problem.
Miday’s last phone call was to the Missouri PHP. Karen Miday believes they had a chance to help him.
“I think all they needed to do was say, get yourself to a place of safety, you know, we’re behind you. That was all they needed to do,” she said.
Dr. Miday had been to one of the program’s approved out-of-state treatment centers before, where he followed the PHP’s requirements exactly. Then, just as he was about to start a new fellowship, he had a relapse.
Karen told the I-Team that he knew he needed help, but he also didn’t want to lose his new job. He suggested to the PHP that he could go to the outpatient program at a recovery center in St. Louis. This would let him keep his job and get treatment.
When Dr. Miday called the Missouri PHP, they said he must go to one of their “preferred” centers outside of the state. If he didn’t, the organization said, they would report Dr. Miday to the medical board.
“I think he thought there was no way out,” Karen said. “They have dual agency. It’s like being a policeman and a therapist at the same time.”
The list of approved facilities for Missouri physicians to get treatment includes just one in the state of Missouri. The nearest out-of-state option is in Lawrence, Kan.
“There’s no legitimate reason why they should have that handful of centers around the country that they prefer to use,” said Boyd.
“You start thinking after a while if there’s some diagnosing for dollars going on because now it’s not just substance use disorders, but now the “disruptive physician” and they’re talking about aging physicians,” said Miday.
Many doctors told the I-Team that the same lack of options that Dr. Miday felt is the reason that they fear contacting their local PHP when they really need help. That could put you at risk.
“If they’re afraid to ask for help, the chance that you’re going to get a doctor who shouldn’t be taking care of patients that day, goes up. And you won’t even be able to know what the chances that that’ll happen. Because nobody will say anything,” said Hammen.
The I-Team reached out to the Missouri Physician’s Health Program with questions, and even went to the home of program director Bob Bondurant, RN, to ask them. He declined to talk about the doctors’ concerns, as did the Missouri Medical Association, and the Missouri Board of Healing Arts.
The National Federation of State PHPs declined to answer any of our specific questions about how their programs work. Instead, they issued this statement:
“Physician Health Programs (PHPs) across the United States and Canada provide physicians and other health care professionals a resource to ensure they are healthy, can practice their craft and at the same time ensure public safety. Today’s physicians often suffer from stress and burnout. A smaller number develop substance use disorders and depression. We are a ready resource to physicians with such untreated conditions who would otherwise be at risk to the public an/or face loss of licensure by their state medical board. PHPs lessen the significant barriers that stand in the way of physicians asking for help.
Treatment is necessarily different for those in safety-sensitive professions, such as pilots and physicians; PHPs help physicians access care specifically designed to their needs. Our goal is to restore physicians’ lives and safely return them to patient care. Research as shown that the PHP care model has unmatched long-term consequences for substance use disorders. Additional research demonstrates successful graduates of PHP’s have a lower risk of malpractice.”
“There’s no legitimate reason why they should have that handful of centers around the country that they prefer to use,” said Boyd.
“You start thinking after a while if there’s some diagnosing for dollars going on because now it’s not just substance use disorders, but now the “disruptive physician” and they’re talking about aging physicians,” said Miday.
Many doctors told the I-Team that the same lack of options that Dr. Miday felt is the reason that they fear contacting their local PHP when they really need help. That could put you at risk.
“If they’re afraid to ask for help, the chance that you’re going to get a doctor who shouldn’t be taking care of patients that day, goes up. And you won’t even be able to know what the chances that that’ll happen. Because nobody will say anything,” said Hammen.
The I-Team reached out to the Missouri Physician’s Health Program with questions, and even went to the home of program director Bob Bondurant, RN, to ask them. He declined to talk about the doctors’ concerns, as did the Missouri Medical Association, and the Missouri Board of Healing Arts.
The National Federation of State PHPs declined to answer any of our specific questions about how their programs work. Instead, they issued this statement:
“Physician Health Programs (PHPs) across the United States and Canada provide physicians and other health care professionals a resource to ensure they are healthy, can practice their craft and at the same time ensure public safety. Today’s physicians often suffer from stress and burnout. A smaller number develop substance use disorders and depression. We are a ready resource to physicians with such untreated conditions who would otherwise be at risk to the public an/or face loss of licensure by their state medical board. PHPs lessen the significant barriers that stand in the way of physicians asking for help.
Treatment is necessarily different for those in safety-sensitive professions, such as pilots and physicians; PHPs help physicians access care specifically designed to their needs. Our goal is to restore physicians’ lives and safely return them to patient care. Research as shown that the PHP care model has unmatched long-term consequences for substance use disorders. Additional research demonstrates successful graduates of PHP’s have a lower risk of malpractice.”













 In response to a request for documents submitted for specific board hearings the board has not provided a single satisfactory response. They have not been able to provide a single document that is chronologically consistent with it being considered at the board hearing for which it was submitted. I had no expectations they would and this was the precise point of my record request. These are documents that should exist but do not exist. The vault is empty. None of the documents are in the records because they were suppressed on arrival and never got to the full board. They never considered any of it. The records do not exist.
In response to a request for documents submitted for specific board hearings the board has not provided a single satisfactory response. They have not been able to provide a single document that is chronologically consistent with it being considered at the board hearing for which it was submitted. I had no expectations they would and this was the precise point of my record request. These are documents that should exist but do not exist. The vault is empty. None of the documents are in the records because they were suppressed on arrival and never got to the full board. They never considered any of it. The records do not exist. It has now been over two months and this shows how transparency is not just about shedding light on what is there but what is not there–transparency can also illuminate contrivances and lies. If these documents existed then they would have provided them long ago and this is all coming to light as a result of Public Records Division staff enforcing new Public Records Law and they should be applauded for their integrity, honesty and genuine concern. In a culture of deference, impunity and apathy where giving allowances are the rule rather than the exception this agency deserves an A+ amidst a sea of D’s and F’s.
It has now been over two months and this shows how transparency is not just about shedding light on what is there but what is not there–transparency can also illuminate contrivances and lies. If these documents existed then they would have provided them long ago and this is all coming to light as a result of Public Records Division staff enforcing new Public Records Law and they should be applauded for their integrity, honesty and genuine concern. In a culture of deference, impunity and apathy where giving allowances are the rule rather than the exception this agency deserves an A+ amidst a sea of D’s and F’s.



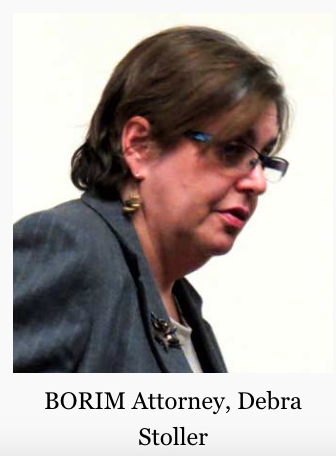


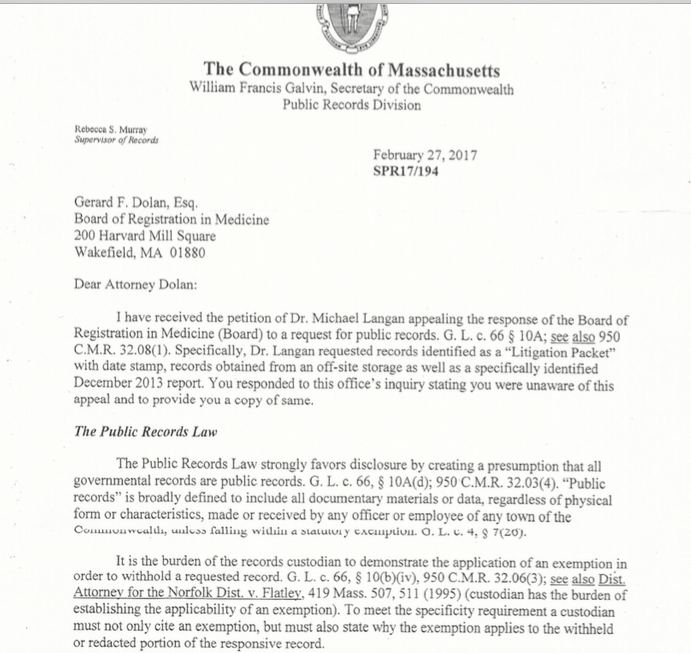

 These documents were requested to determine if they were ever entered into evidence as none of them had ever been addressed. The date-stamps confirm they were not. Requests to clarify the illegible dates have been curtailed and rebuffed with the last response being June 17, 2016 when Katy Condon E-mailed me that she was “currently working on it.”
These documents were requested to determine if they were ever entered into evidence as none of them had ever been addressed. The date-stamps confirm they were not. Requests to clarify the illegible dates have been curtailed and rebuffed with the last response being June 17, 2016 when Katy Condon E-mailed me that she was “currently working on it.” None of the sleazy misconduct here has ever been addressed. This is not just evidence withheld but crimes concealed and the seriousness and severity of this needs to register somewhere. The fact of the matter is a state attorney was made aware of felony crimes that were committed by identifiable individuals in obvious conspiratorial collusion to falsely create evidence. The intentions are clear. This is not accidental but deliberate. The documents were provided to a state employee who instead of reporting what they revealed, concealed them and never brought them up again. Sanchez is a Board of Registration in Medicine licensee. He must abide by the same rules and regulations and laws as everyone else. Allowances and selective application of the law are not part of good governance.
None of the sleazy misconduct here has ever been addressed. This is not just evidence withheld but crimes concealed and the seriousness and severity of this needs to register somewhere. The fact of the matter is a state attorney was made aware of felony crimes that were committed by identifiable individuals in obvious conspiratorial collusion to falsely create evidence. The intentions are clear. This is not accidental but deliberate. The documents were provided to a state employee who instead of reporting what they revealed, concealed them and never brought them up again. Sanchez is a Board of Registration in Medicine licensee. He must abide by the same rules and regulations and laws as everyone else. Allowances and selective application of the law are not part of good governance. The crimes here are not Annie Dookhan level misconduct isolated to just Massachusetts either. The documents sho collusion between a state physician health program and its drug-testing lab, a pattern that appears to be standard operating procedure as allegations of laboratory fraud as well as diagnosis fraud are coming in all across the country and the consequences of these tests can be grave. These tests end careers and can end lives. I know of multiple suicides due to allegedly false tests; many using this same test. The fact that the falsified test was requested by fax and complied with without hesitation shows a chilling absence of empathy. It is unconscionable. These are more murders than suicides as it is an institutional injustice with no lifeline. No outside agency exists with authority to both investigate lab misconduct and provide punishment if it is found.
The crimes here are not Annie Dookhan level misconduct isolated to just Massachusetts either. The documents sho collusion between a state physician health program and its drug-testing lab, a pattern that appears to be standard operating procedure as allegations of laboratory fraud as well as diagnosis fraud are coming in all across the country and the consequences of these tests can be grave. These tests end careers and can end lives. I know of multiple suicides due to allegedly false tests; many using this same test. The fact that the falsified test was requested by fax and complied with without hesitation shows a chilling absence of empathy. It is unconscionable. These are more murders than suicides as it is an institutional injustice with no lifeline. No outside agency exists with authority to both investigate lab misconduct and provide punishment if it is found. These documents show crimes. I have re-requested these records under HB 4333 as well as documents that Bertram claims “puts the matter to rest.” He claims they reviewed their “records” and “minutes’ for the December 21, 2011 hearing and all of this was “carefully considered.” This begs the question has anyone else outside this circle ever even looked at these documents? They were never considered and if the Board complies with HB 4333 the uncensored documents will add to the already overwhelming evidence that this is the case. It is certain that every illegible date uncovered will reveal a date sometime after the hearing for which it was submitted. The documents retrieved from “off-site storage” does not exist. The Board has not used off-site storage since 2004 when they installed the Document Imaging Unit. This fact can be found in multiple annual reports and other documents. The question are they trying to cover-up a cover-up of a cover-up? Why is he going to such great lengths to protect criminals, allow this racket to continue and inevitably cause a great deal of harm to many? Rules of professional conduct forbid attorney’s from being complicit in fraud. The obvious cannot be ignored. These are crimes and both the commission and concealment of them are egregious. This is not simply a matter of withholding evidence but of concealing crimes and it puts both doctors and the public in immediate or eventual danger.
These documents show crimes. I have re-requested these records under HB 4333 as well as documents that Bertram claims “puts the matter to rest.” He claims they reviewed their “records” and “minutes’ for the December 21, 2011 hearing and all of this was “carefully considered.” This begs the question has anyone else outside this circle ever even looked at these documents? They were never considered and if the Board complies with HB 4333 the uncensored documents will add to the already overwhelming evidence that this is the case. It is certain that every illegible date uncovered will reveal a date sometime after the hearing for which it was submitted. The documents retrieved from “off-site storage” does not exist. The Board has not used off-site storage since 2004 when they installed the Document Imaging Unit. This fact can be found in multiple annual reports and other documents. The question are they trying to cover-up a cover-up of a cover-up? Why is he going to such great lengths to protect criminals, allow this racket to continue and inevitably cause a great deal of harm to many? Rules of professional conduct forbid attorney’s from being complicit in fraud. The obvious cannot be ignored. These are crimes and both the commission and concealment of them are egregious. This is not simply a matter of withholding evidence but of concealing crimes and it puts both doctors and the public in immediate or eventual danger.


 Employee Assistance Programs (EAPs)
Employee Assistance Programs (EAPs) With time these programs broadened to include other issues that could potentially impact job performance. Worker Assistance Programs (WAPs) emerged in the 1950s when companies such as Consolidated Edison, Standard Oil of New Jersey, and American Cyanamid extended their alcoholism programs to also address mental health issues in their employees (Roman, 1981; Steele, 1995).
With time these programs broadened to include other issues that could potentially impact job performance. Worker Assistance Programs (WAPs) emerged in the 1950s when companies such as Consolidated Edison, Standard Oil of New Jersey, and American Cyanamid extended their alcoholism programs to also address mental health issues in their employees (Roman, 1981; Steele, 1995). Another significant development was the formation of private EAP firms that began to offer EAP services and drug-testing via contracts with employers. One such example is Bensinger, DuPont & Associates (BDA) which was founded in 1982 by former DEA Chief Peter Bensinger and National Institute on Drug Abuse (NIDA) founding director Robert Dupont. BDA became the sixth largest employee assistance program (EAP) provider in the United States and provided workplace drug testing and other services to some 10-million employees of companies such as Kraft Foods, American Airlines, Johnson & Johnson and the Federal Aviation Administration (FAA). On December 1, 2015 Bensinger, DuPont & Associates was acquired by the Canadian firm of Mourneau Sheppel which employs 4000 plus individuals and has approximately 20,000 clients ranging from small businesses to some of the largest corporations in North America.
Another significant development was the formation of private EAP firms that began to offer EAP services and drug-testing via contracts with employers. One such example is Bensinger, DuPont & Associates (BDA) which was founded in 1982 by former DEA Chief Peter Bensinger and National Institute on Drug Abuse (NIDA) founding director Robert Dupont. BDA became the sixth largest employee assistance program (EAP) provider in the United States and provided workplace drug testing and other services to some 10-million employees of companies such as Kraft Foods, American Airlines, Johnson & Johnson and the Federal Aviation Administration (FAA). On December 1, 2015 Bensinger, DuPont & Associates was acquired by the Canadian firm of Mourneau Sheppel which employs 4000 plus individuals and has approximately 20,000 clients ranging from small businesses to some of the largest corporations in North America.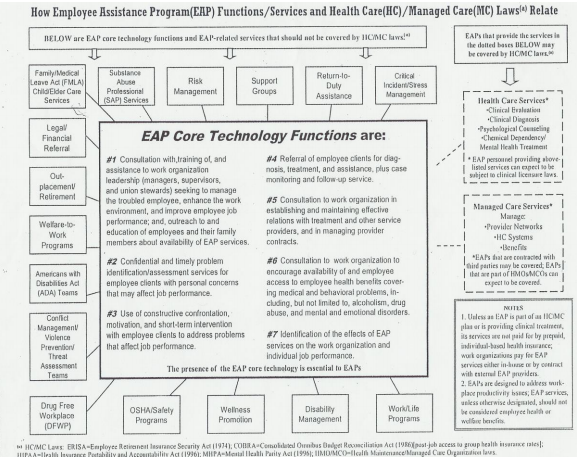
 This topic is addressed in the book Employee Assistance Programs: What Works and what Doesn’t by Lawrence Mannion in which he discusses the notion of “control” in the context of managed mental health care. For those wishing to control any direction, entity or circumstances pertaining to these types of services Mannion states:
This topic is addressed in the book Employee Assistance Programs: What Works and what Doesn’t by Lawrence Mannion in which he discusses the notion of “control” in the context of managed mental health care. For those wishing to control any direction, entity or circumstances pertaining to these types of services Mannion states:

 The White Paper’s writing Committee Chair, Dr. Robert Dupont, described this “New Paradigm” in his
The White Paper’s writing Committee Chair, Dr. Robert Dupont, described this “New Paradigm” in his  These six lessons are:
These six lessons are: The “PHP-blueprint” is being promoted as “Gold standard” and a “
The “PHP-blueprint” is being promoted as “Gold standard” and a “






 diagnosis. Pervasive problems include:
diagnosis. Pervasive problems include:
 Creating Bogus Risks of Danger
Creating Bogus Risks of Danger The primary architects of this system can be found on a list of Fellows of the American Society of Addiction Medicine. The list can be seen
The primary architects of this system can be found on a list of Fellows of the American Society of Addiction Medicine. The list can be seen 

