“Gentlemen, it is a disagreeable custom to which one is too easily led by the harshness of the discussions, to assume evil intentions. It is necessary to be gracious as to intentions; one should believe them good, and apparently they are; but we do not have to be gracious at all to inconsistent logic or to absurd reasoning. Bad logicians have committed more involuntary crimes than bad men have done intentionally.”–Pierre S. du Pont (September 25, 1790)
“It is easier to believe a lie one has heard a hundred times than a truth one has never heard before.” –Robert S. Lynd
Ridgeview Institute was a drug and alcohol treatment program for “impaired physicians” in Georgia created by G. Douglas Talbott, a former cardiologist who lost control of his drinking and recovered through the 12-steps of Alcoholics Anonymous.
Up until his death on October 18, 2014 at the age of 90, Talbott owned and directed a number of treatment facilities for impaired professionals, most recently the Talbott Recovery Campus in Atlanta, one of the preferred referrals for physicians ordered into evaluation and treatment by licensing boards today.
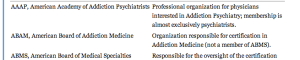
G. Douglas Talbott is a prototypical example of an “impaired physician movement” physician–in fact in many ways he may be considered the”godfather” of the current organization. He helped organize and serve as past president of the American Society of Addiction Medicine (ASAM) and was a formative figure in the American Medical Association’s (AMA’s) Impaired Physician Program.

G. Douglas Talbott (center), with sons Mark (left) and Dave (right). (image: Ham Biggar)
The cost of a 28-day program for nonprofessionals at Ridgeview in 1987 was $10,000 while the cost was “higher for those going through impaired-health professionals program,” which lasted months rather than 28 days.1
In 1975 after creating the DeKalb County Impaired Physicians Committee for the Medical Association of Georgia, Talbott founded the Georgia Disabled Doctors Program for the assessment and treatment of physicians. Founded in part because “traditional one-month treatment programs are inadequate for disabled doctors,” and they required longer treatment to recover from addiction and substance abuse. According to Talbott, rehabilitation programs that evaluate and treat the rest of the population for substance abuse issues are incapable of doing so in doctors as they are unlike any other of the inhabitants of our society. Physicians are unique. Unique because of their incredibly high denial”, and he includes this in what he calls the “Four MDs,” “M-Deity”, “Massive Denial” “Militant Defensiveness” and “More Drugs.”2 And these factors set doctors apart from the rest.
According to Talbott, “impaired doctors must first acknowledge their addiction and overcome their ‘terminal uniqueness’ before they can deal with a drug or alcohol problem.” “Terminal uniqueness “ is a phrase Talbott uses to describe doctors’ tendency to think they can heal themselves.
“M-Deity” refers to doctors “being trained to think they’re God;”3 blinded by an overblown sense of self-importance and thinking that they are invincible-an unfounded generalization considering the vast diversity of individuals that make up our profession. Although this type of personality does exist in medicine, it is a small minority -just one of many opinions with little probative value offered as factual expertise by the impaired physician movement and now sealed in stone.

Former Assistant Surgeon General (Ret) Admiral (Ret) John C. Duffy
This attitude, according to some critics, stems from the personal histories of the treatment staff, including Talbott, who are recovering alcoholics and addicts themselves. One such critic was Assistant Surgeon General under C. Everett Koop John C. Duffy who said that Ridgeview suffered from a “boot-camp mentality” toward physicians under their care and “assume every physician suffering from substance abuse is the same lying, stealing, cheating, manipulating individual they were when they had the illness. Certainly some physicians are manipulative, but it’s naïve to label all physicians with these problems.”1
LeClair Bissell
American Society of Addiction Medicine (ASAM) President (1981-1983) LeClair Bissell was also highly critical of Talbott’s approach. Bissell, co-author of the first textbook of ethics for addiction professionals4 when asked if there was any justification to the claim that doctors are sicker than other people and more vulnerable to addiction replied:
“Well, based on my treatment experience, I think they are less sick and much easier to treat than many other groups. I think one reason for that is that in order to become a physician…one has to have jumped over a great many hurdles. One must pass the exams, survive the screening tests and the interviews, be able to organize oneself well enough to do examinations and so on, and be observed by a good many colleagues along the way. Therefore I think the more grossly psychotic, or sicker, are frequently screened out along the way. The ones we get in treatment are usually people who are less brain-damaged, are still quite capable of learning, are reasonably bright. Not only that, but they are quite well motivated in most cases to hang on to their licenses, the threat of the loss of which is frequently what puts them in treatment in the first place. So are they hard to treat? No! Are they easy patients? Yes! Are they more likely to be addicted than other groups? We don’t know.”5
“I’m not much for the bullying that goes along with some of these programs,” Bissell commented to the Atlanta Journal and Constitution in 1987.3
The constitution did a series of reports after five inpatients died by suicide during a four-year period at Ridgeview.6 In addition there were at least 20 more who had killed themselves over the preceding 12 years after leaving the treatment center.1
Bissell, the recipient of the 1997 Elizabeth Blackwell Award for outstanding contributions to the cause of women and medicine remarked: “When you’ve got them by the license, that’s pretty strong leverage. You shouldn’t have to pound on them so much. You could be asking for trouble.”3
According to Bissell: “There’s a lot of debate in the field over whether treatment imposed by threats is worthwhile…To a large degree a person has to seek the treatment on his own accord before it will work for him.”3
A jury awarded $1.3 million to the widow of one of the deceased physicians against Ridgeview,7 and other lawsuits initiated on behalf of suicides were settled out of court.6
The Constitution reported that doctors entered the program under threats of loss of licensure “even when they would prefer treatment that is cheaper and closer to home.” 8 The paper also noted that Ridgeview “enjoys unparalleled connections with many local and state medical societies that work with troubled doctors,” “licensing boards often seek recommendations from such groups in devising an approved treatment plan,” and those in charge are often “physicians who themselves have successfully completed Ridgeview’s program.”8
In 1997 William L. White interviewed Bissell whom he called “one of the pioneers in the treatment of impaired professionals.” The interview was not published until after her death in 2008 per her request. Noting that her book Alcoholism in the Professions9 “remains one of the classics in the field”, White asked her when those in the field began to see physicians and other professionals as a special treatment population; to which she replied:
“When they started making money in alcoholism. As soon as insurance started covering treatment, suddenly you heard that residential treatment was necessary for almost everybody. And since alcoholic docs had tons of money compared to the rest of the public, they not only needed residential treatment, they needed residential treatment in a special treatment facility for many months as opposed to the shorter periods of time that other people needed.”10
Talbott claimed a “92.3 percent recovery rate according to information compiled from a five-year follow-up survey based on complete abstinence and other treatment.”11 A 1995 issue of The Federal Bulletin: The Journal of Medical Licensure and Discipline, published by the Federation of State Medical Boards, contains articles outlining impaired physician programs in 8 separate states. Although these articles were little more than descriptive puff-pieces written by the state PHP program directors and included no described study-design or methodology the Editor notes a success rate of about 90% in these programs and others like them 12 and concludes:
“cooperation and communication between the medical boards and the physician health programs must occur in an effort to protect the public while assisting impaired physicians in their recovery.” 12
No one bothered to examine the methodology to discern the validity of these claims and it is this acceptance of faith without objective assessment that has allowed the impaired physician movement through the ASAM and FSPH to advance their agenda; confusing ideological opinions with professional knowledge.
“There is nothing special about a doctor’s alcoholism,” said Bissel
“These special facilities will tell you that they come up with really wonderful recovery rates. They do. And the reason they do is that any time you can grab a professional person by the license and compel him or her into treatment and force them to cooperate with that treatment and then monitor them for years, you’ll get good outcomes—in the high 80s or low 90s in recovery rates—no matter what else you do.”10
“The ones I think are really the best ones were not specialized. There were other well-known specialty clinics that claimed all the docs they treated got well, which is sheer rot. They harmed a great many people, keeping them for long, unnecessary treatments and seeing to it that they hit their financial bottom for sure: kids being yanked out of college, being forced to sell homes to pay for treatment, and otherwise being blackmailed on the grounds that your husband has a fatal disease. It’s ugly.”10
Stanton Peele’s “In the Belly of the American Society of Addiction Medicine Beast” describes the coercion, bullying, threats and indoctrination that are standard operating procedure in Talbott’s facilities.13 Uncooperative patients, “and this covers a range of sins of commission or omission including offering one’s opinion about one’s treatment,” are “threatened with expulsion and with not being certified-or advocated for with their Boards.”13
The cornerstone of treatment is 12-step spiritual recovery. All new patients are indoctrinated into A.A. and coerced to confess they are addicts or alcoholics. Failure to participate in A.A. and 12-step spirituality means expulsion from the program with the anticipated result being loss of one’s medical license.
In May 1999 Talbott stepped down as president of the American Society of Addiction Medicine (ASAM) as a jury awarded Dr. Leonard Masters a judgment of $1.3 million in actual damages and an undisclosed sum in punitive damages for fraud, malpractice, and the novel claim of false imprisonment.14
The fraud finding required a finding that errors in the diagnosis were intentional. Masters, who was accused of overprescribing narcotics to his patients was told by the director of the Florida PHP that he could either surrender his medical license until the allegations were disproved or submit to a four-day evaluation.
Masters agreed to the latter, thinking he would have an objective and fair evaluation. He was instead diagnosed as “alcohol dependent” and coerced into “treatment under threat of loss of his medical license. Staff would routinely threaten to report any doctor who questioned any aspect of their diagnosis or treatment to their state medical boards “as being an impaired physician, leaving necessary treatment against medical advice,”14 the equivalent of professional suicide.
Masters, however, was not an alcoholic.
According to his attorney, Eric. S. Block, “No one ever accused him of having a problem with alcohol. Not his friends, not his wife, not his seven children, not his fellow doctors, not his employees, not his employers, No one.” 15
He was released 4 months later and forced to sign a five-year “continuing care” contract with the PHP, also under continued threat of his medical license.
Talbott faced no professional repercussions and no changes in their treatment philosophy or actions were made. They still haven’t. They have simply tightened the noose and taken steps to remove accountability.
Up until his recent death, Talbott continued to present himself and ASAM as the most qualified advocates for the assessment and treatment of medical professionals for substance abuse and addiction.16
ASAM and like-minds still do.
In most states today any physician referred for an assessment for substance abuse will be mandated to do so in a facility just like Ridgeview.
There is no choice. In mechanics and mentality, this same system of coercion, control, and indoctrination has metastasized to almost every state only more powerful and opaque in an unregulated gauntlet protected from public scrutiny, answerable and accountable to no one. Laissez faire Machiavellian egocentricity unleashed. For what they have done is taken the Ridgeview model and replicated it over time state by state and tightened the noose. By subverting the established Physician Health Programs (PHPs) started by state medical societies and staffed by volunteer physicians they eliminated those not believing in the mentality of the groupthink. They then mandated assessment and treatment of all doctors be done at a “PHP-approved” facility which means a facility identical to Ridgeview. This was done under the scaffold of the Federation of State Physician Health Programs (FSPHP). They are now in charge of all things related to physician wellness in doctors.
- Durcanin C, King M. The suicides at Ridgeview Institute: Suicides mar success at Ridgeview with troubled professionals. Atlanta Journal and Constitution. December 18, 1987, 1987: A13.
- Gonzales L. When Doctors are Addicts: For physicians getting Drugs is easy. Getting help is not. Chicago Reader. July 28, 1988, 1988.
- King M, Durcanin C. The suicides at Ridgeview Institute: A Doctor’s treatment program may be too tough, some say. Atlanta Journal and Constitution. December 18, 1987a, 1987: A12.
- Bissell L, Royce JE. Ethics for Addiction Professionals. Center City, Minnesota: Hazelden; 1987.
- Addiction Scientists from the USA: LeClair Bissell. In: Edwards G, ed. Addiction: Evolution of a Specialist Field. 1 ed: Wiley, John & Sons, Incorporated; 2002:408.
- Durcanin C. The suicides at Ridgeview Institute: Staff members didn’t believe Michigan doctor was suicidal. Atlanta Journal and Constitution. December 18, 1987, 1987: A8.
- Ricks WS. Ridgeview Institute loses $1.3 million in suit over suicide. Atlanta Journal and Constitution. October 11, 1987, 1987: A1.
- King M, Durcanin C. The suicides at Ridgeview Institute: Many drug-using doctors driven to Ridgeview by fear of losing licenses. Atlanta Journal and Constitution. December 18, 1987b, 1987: A1.
- Bissell L, Haberman PW. Alcoholism in the Professions. Oxford University Press; 1984.
- White W. Reflections of an addiction treatment pioneer. An Interview with LeClair Bissell, MD (1928-2008), conducted January 22, 1997. Posted at http://www.williamwhitepapers.com. 2011.
- Williams c. Health care field chemical dependency threat cited. The Tuscaloosa News. January 16, 1988, 1988: 16.
- Schneidman B. The Philosophy of Rehabilitation for Impaired Physicians. The Federal Bulletin: The Journal of Medical Licensure and Discipline. 1995;82(3):125-127.
- Peele S. In the Belly of the American Society of Addiction Medicine Beast. The Stanton Peele Addiction Website (accessed March 28, 2014) http://web.archive.org/web/20080514153437/http://www.peele.net/debate/talbott.html.
- Ursery S. $1.3M verdict coaxes a deal for doctor’s coerced rehab. Fulton County Daily Report. May 12, 1999b 1999.
- Ursery S. I was wrongly held in alcohol center, doctor charges. Fulton Count y Daily Report. April 27, 1999a 1999.
- Parker J. George Talbott’s Abuse of Dr. Leon Masters MD ( http://medicalwhistleblowernetwork.jigsy.com/george-talbott-s-abuse-of-leon-masters ). Medical Whistelblower Advocacy Network.
There is enormous inertia—a tyranny of the status quo—in private and especially governmental arrangements. Only a crisis—actual or perceived—produces real change. When that crisis occurs, the actions that are taken depend on the ideas that are lying around. That, I believe, is our basic function: to develop alternatives to existing policies, to keep them alive and available until the politically impossible becomes politically inevitable.-Milton Friedman