—There is no place in science for consensus or opinion, only evidence.-Claude Bernard
Dear Senator Warren,
Thank you for your reply regarding laboratory developed tests (LDTs) and the need for regulatory oversight. As you mention, LDTs are developed without FDA approval—a pathway in which is not even necessary to prove validity of a test (that it is actually testing what it claims to be testing for) to bring it to market. With no FDA oversight or regulation a commercial lab can claim any validity they want in marketing these tests. The regulation debate has focused on the reliability and validity of a number of clinical tests marketed with unverified claims of accuracy such as prenatal screening and Lyme disease and this lack of oversight is a direct threat to patient safety.
I am sure you would agree with me that the importance of tests diagnostic accuracy is directly proportional to that tests potential to cause patient harm if reported inaccurately.
Sensitivity and specificity are important components of any diagnostic test because there are consequences associated with both false-positive and false negative results.
A test falsely indicating the absence of a condition in someone who truly has it can delay or prevent needed treatment wile a test falsely indicating the presence of a condition in someone who does not truly have it can result in unnecessary testing and treatment.
Incorrect treatment and false labeling of patients can also occur. Therefore diagnostic accuracy is paramount if a test is being used as the basis for further tests and treatment. Any test being used as a basis for further tests or treatment needs to be accurate. It needs to be reliable and valid. Moreover, if the consequences of a test can result in significant patient harm (such as unneeded chemotherapy) it needs to be either 100% accurate or be combined with other tests to confirm the true diagnosis.
“Forensic” vs. “Clinical” Laboratory Testing
“Forensic” testing differs from “clinical” testing because of the consequences and the process is tightly controlled because false-positive results are unacceptable as the consequences can be grave, far-reaching and even permanent.
Forensic testing demands special handling and safeguards to protect the donor such as validated tests, certified labs, strict chain-of-custody procedures and MRO (Medical Review Officer) review. These safeguards of quality control assure the validity and integrity of the specimen. The LDT pathway was not designed for forensic tests.
Forensic Laboratory Developed Tests (LDTs)
Paradoxically, laboratory developed tests with the potential to cause life-changing and possibly irreparable harm have been absent from the regulatory debate; LDT drug and alcohol tests used for “forensic” monitoring purposes.
A panoply of tests using urine, blood, hair, fingernails breath and saliva have been developed and brought to market since 2003 when the first one was introduced by Gregory Skipper, then Medical Director of the Alabama Physicians Health Program, who “convinced the initial lab in the USA, NMS near Philadelphia to start performing EtG testing.” 1
Developed as an LDT, Skipper and NMS then claimed the alcohol biomarker (which was discovered in the 1950s) “appeared to be 100 percent specific” in detecting covert use of alcohol based on a study he coauthored that involved a mere 35 forensic psychiatric inpatients in Germany, all male. 2 With this “evidence-base” and a not yet published paper in the pipeline,3 Skipper then pitched the test to the Federation of State Medical Boards (FSMB) as an accurate and reliable tool detect covert alcohol use in health care professionals.
Policy Entrepreneurship
In “Agendas, Alternatives, and Public Policies,”4 John W. Kingdon describes the problem, policy and political streams involved in public policy making. When these three streams come together a specific problem becomes important on the agenda, policies matching the problem get attention, and then policy change becomes possible.
Kingdon also describes “policy entrepreneurs’ who use their knowledge of the process to further their own policy ends. They ‘lie in wait… with their solutions at hand, waiting for problems to float by to which they can attach their solutions, waiting for a development in the political stream they can use to their advantage.”4
And due to a perfect confluence of streams ( Institute of Medicine report that 44,000 people die each year due to medical error,5 media reports of “impaired physicians,” the the war-on-drugs, etc.) the FSMB was swayed into accepting not just the validity but the necessity of using an alcohol biomarker of unknown reliability and validity on doctors referred to or monitored by state Physician Health Programs (PHPs) .
As the national organization that gives guidance to state medical boards through public policy development and recommendations, the individual state medical boards adopted use of the test without critical appraisal and no meaningful opposition.
Shortly after its founding in 1912, the FSMB began publishing a journal called the Quarterly of the Federation of State Boards of the United States. Now known as the Journal of Medical Regulation, the publication has archived all issues with full articles dating back to 1967 and, as the official journal of the national organization involved in medical licensing and regulation this facilitates an unskewed and impartial examination of how and when specific issues and problems were presented and who presented them and, in doing so, the “policy entrepreneurship” Kingdon describes can be seen quite clearly. For example a 1995 issue containing articles written by the program directors of PHPs in 8 different states contains an FSMB editorial acknowledging the reported 90% success rate claimed of these programs (in part attributed to the 90-day inpatient treatment programs) that concludes:
“Cooperation and communication between the medical boards and the physician health programs must occur in an effort to protect the public while assisting impaired physicians in their recovery.” 6
No one bothered to examine the methodology of these reports to discern the validity of the claims and it is this acceptance of faith without objective assessment that has allowed the passage of flawed public policy in medical regulation.
Nowhere is “policy entrepreneurship” more glaringly displayed as it is in a 2004 issue promoting the use of EtG in monitoring doctors as under the same cover is an article identifying both the need7 for such a test and an article providing the solution.8
“Detection of Alcohol Use in Monitored Aftercare Programs: A National Survey of State Physician Health Programs,” a survey of state Physician Health Programs (PHPs) concludes that “surreptitious alcohol use” is a significant concern” for PHPs, there is no current “best method” for detection, but a promising new test with “exceptional specificity (100 percent) and sensitivity” in detecting small amounts of alcohol for up to 18 hours has recently become available.7
This same issue contains an article authored by Skipper about a new marker “not detectable unless alcohol has been consumed” recently introduced in the United States and now commercially available.”8
Notably absent from both of these articles is Skipper’s role in the commercial availability of the test. This conflict-of-interest is nowhere mentioned in this display of “creating a market then filling it.”
This “regulatory sanctification” of the test implied its tacit approval by the medical profession (i.e. “if they are using it on doctors it must be valid”) and facilitated its marketing to other monitoring agencies (nurses, airline pilots) as well as Courts and Probation Departments where those doing the monitoring had absolute power while those being monitored had no voice.
Bent Science
In Bending Science: How Special Interests Corrupt Public Health Research9, Thomas McGarity and Wendy Wagner describe how special interest groups scheme to advance their own economic or ideological goals by using carefully crafted distorted or “bent” science to influence legal, regulatory and public health policy. The authors describe how those making these decisions often assume the information that reaches them has been sufficiently vetted by the scientific community as it flows through a pipeline of rigorous peer-review and professional oversight and that the final product that exits the pipeline is unbiased and produced in accordance with the norms and procedures of science.
McGarity and Wagner note the serious and sometimes horrific consequences of bent science and provide examples involving Tobacco and Big Pharma . The authors call for:
“..immediate action to reduce the role that bent science plays in regulatory and judicial decision making” and the need for the scientific community to be involved in “designing and implementing reform.”
“Shedding even a little light on how advocates bend policy -relevant science could go a long way toward remedying these problems. Indeed, precisely because the advocates have overtaken the law in this area, heightened attention to the social costs of bending science could itself precipitate significant change.”
In the case of EtG this shedding of light is not very hard as no “carefully crafted” studies bending science were used to sway opinion. None existed. The only items in the pipeline were directly related to Skipper. If anyone dare to look, the Emperor has no clothes.
Lack of Answerability and Accountability
There are difficulties in challenging bent science including a general lack of recognition of the problem and an absence of counter-studies to oppose deliberately manufactured ends-oriented research. This has proven true with the myriad LDTs introduced into the marketplace as no counter-forces or competing economic interests producing counter-studies exist.
Multiple lawsuits, including a class-action, have been decided in favor of the labs who have taken a stand-your-ground approach supported by a body of industry-related “research” they or their affiliates produced to support the validity and reliability of the tests.
Those affected by these tests either have no power or have had their power removed. Most do not have the resources to mount a defense let alone produce counter-studies questioning the reliability and validity of the tests.
Most employee drug testing follows Department of Health and Human Services (DHHS) guidelines using FDA-approved tests that have specific cutoff levels defining a positive-result in an effort to eliminate false-positive results.10 Procedural safeguards are in place in these programs to protect the donor. Forensic testing programs using LDTs provide no such safeguards as the testing is unregulated and there is no oversight from outside actors.
Unlike clinical LDTs “forensic” LDTs are even exempt from CLIA oversight. The only avenue for complaint is through the College of American Pathologists (CAP) and, as an accrediting agency, they can only address problems by ensuring compliance with CAP guidelines. If an investigation concludes lab error or misconduct CAP can mandate the lab correct the test result and come into compliance with their guidelines under threat of loss of accreditation but no other consequences exist. Accountability has been removed yet the consequences to those harmed by these are significant and without remedy.
State Physician Health Programs
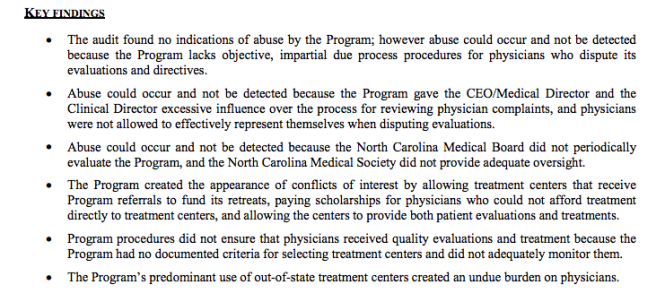
As is the case with the LDTs they introduced, Physician Health Programs have no oversight or regulation. A 2013 Audit of the North Carolina PHP 11 prompted by complaints from doctors and performed by State Auditor Beth Woods found absolutely no oversight of the program by either the state medical board or medical society and that “abuse could occur without being detected.”
The Audit also found that doctors were predominantly referred to the same “PHP-approved” out-of-state facilities to which they in part attribute their high success rates in treatment. Interestingly the PHP could not identify what quality indicators or quantitative measurements were used by the PHP to “approve” the “PHP-approved” facilities.
In January of 2015 a Federal class action lawsuit was filed in the Eastern District of Michigan against the state PHP program and found health care providers were subject to the same referral system using these out-of-state facilities. The suit alleges constitutional violations related to the forced medical treatment of health care professionals and the “callous and reckless termination of professional licenses without due process.” 12
As with North Carolina, the Michigan PHP will be unable to provide what quality indicators and quantitative measurements are being used to “qualify” and “approve these facilities. None exist. The sole indicators for approving these assessment centers are ideological and economic. In fact, the medical directors of most, if not all, of these facilities can be seen on this list of “like-minded docs.”
Institutional Injustice
You once said “People feel like the system is rigged against them. And here’s the painful part: they’re right. The system is rigged.”
So too is this system.
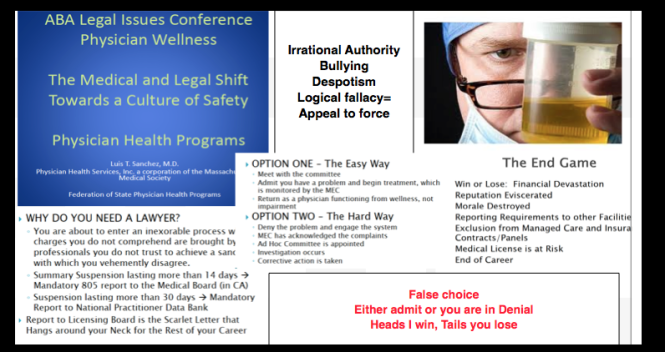
As the Michigan lawsuit notes: “Unfortunately, a once well-meaning program has turned into a highly punitive and involuntary program where health professionals are forced into extensive and unnecessary substance abuse/dependence treatment under the threat of the arbitrary application of pre-hearing deprivations.”
This has become the rule not the exception. The Federation of State Physician Health Programs (FSPHP), the same group to which Dr. Skipper belongs, has systematically taken over these programs state by state by removing competent and caring doctors not agreeing with the groupthink and silenced them under threat of litigation if they violate their confidentiality agreements and “peer review” statutes.
The same system of coercion, control and abuse exists in Massachusetts. In the past week alone I have heard from a medical student, a resident and two doctors who complained of misconduct misconduct involving fraudulent testing and falsified diagnoses.
In “Ethical and Managerial Considerations Regarding State Physician Health Programs,” published in the Journal of Addiction Medicine in 2012, Drs. John Knight, M.D. and J. Wesley Boyd, M.D., PhD who collectively have more than 20 years experience with the Massachusetts Physician Health Program (PHP) state that:
“Because PHP practices are unknown to most physicians before becoming a client of the PHP, many PHPs operate out- side the scrutiny of the medical community at large. Physicians referred to PHPs are often compromised to some degree, have very little power, and are, therefore, not in a position to voice what might be legitimate objections to a PHP’s practices.”13
Noting that “for most physicians, participation in a PHP evaluation is coercive, and once a PHP recommends monitoring, physicians have little choice but to cooperate with any and all recommendations if they wish to continue practicing medicine,” Knight and Boyd raise serious ethical and managerial questions about current PHP policies and practice including conflicts of interest in referrals for evaluation and treatment, lack of adherence to standards of care for forensic testing of substances of abuse, violations of ethical guidelines in PHP research, and conflicts of interest with state licensing boards.
Knight and Boyd recommend “the broader medical community begin to reassess PHP’s as a whole” and that “consideration be given toward the implementation of independent ethical oversight and establish and appeals process for PHP clients who feel they are being treated unfairly.” 13
They recommend the relationship between PHP’s and the evaluation and treatment centers and licensing boards be transparent and that national standards be developed “that can be debated by all physicians, not just those who work within PHPs.”13
Accountability, or answerability, is necessary to prevent corruption. This requires both the provision of information and justification for actions. What was done and why? Accountability also requires that consequences be imposed on those who engage in misconduct.
In discussing the financial conflicts-of-interest between PHPs and “PHP-approved” assessment centers Knight and Boyd state:
“..if a PHP highlights a physician as particularly problematic, the evaluation center might–whether consciously or otherwise–tailor its diagnosis and recommendations in a way that will support the PHP’s impression of that physician.”
To “consciously tailor a diagnosis” is fraud. It is political abuse of psychiatry. And it is not only the assessment and treatment centers willing to “tailor” a diagnosis; so too are the labs involved.
Physician Suicide
I can think of nothing more institutionally unjust than an unregulated zero-tolerance monitoring program with no oversight using unregulated drug and alcohol testing of unknown validity. But that is what is occurring. Some of us are trying to expose this corrupt system but barriers exist. As with the Laboratory Developed Tests (LDTs), those involved have intentionally taken steps to remove both answerability and accountability. Both the tests and the body of individuals administering these tests are notable for their lack of transparency, oversight and regulation. This renders them a power unto themselves.
Doctors (and others coerced into Professional Health Programs) across the country have reported going to law enforcement and state agencies only to be turned away. The Federation of State Physician Health Programs (FSPHP) has convinced these outside agencies that this is a “parochial” issue best handled by the medical profession.. Those reporting crimes are turned back over to the very people committing the crimes.
The Massachusetts Medical Society and Massachusetts DPH claim no oversight of the Massachusetts PHP, PHS.inc. The Massachusetts Board of Registration in Medicine (BORM) will not address ethical or even criminal complaints about the doctors involved in the PHP and there is good evidence that some members of the BORM are in fact complicit in unethical and even criminal behavior. As the Massachusetts AGO represents the BORM they defer issues back to them and dig no deeper.
Drs. Knight and Boyd have suggested State Audits and we are hoping that MA State Auditor Suzanne Bump will investigate the MA PHP and the Board of Registration in Medicine’s Physician Health and Compliance Unit shortly.
One major problem is that barriers have been put in place to prevent information from getting to the right people.
The majority of people at medical societies, boards, departments of public health and other organizations are individuals of integrity and honesty but the system has been erected so that valid complaints are deflected, delayed, dismissed or otherwise tabled by sympathizers, apologists and those complicity. The criminal activity the Massachusetts PHP is engaging in is undeniable and indefensible but who is going to hold them to account?
It is going to take a while to reform this system of institutional abuse and it has to be done state by state. Please take a look at the facts and documentary evidence and help me hold them accountable. This needs to be exposed, acknowledged and addressed. Doctors are dying from this system of institutional abuse. It is a public health emergency no one is talking about. Yet those behind the PHP programs are claiming this system of coercion, abuse and control is the “gold standard” of addiction treatment and, using another loophole, they want to expand this system to mainstream healthcare.
Sincerely,
Michael L. Langan, M.D.
- Skipper G. Exploring the Reliability, Frequency, and Methods of Drug Testing: What is Enough to Ensure Compliance?: Alcohol Markers and Devices. 2013; http://www.fsphp.org/Skipper, Exploring the Reliability Frequency and Methods 2 Presentation.pdf.
- Wurst FM, Vogel R, Jachau K, et al. Ethyl glucuronide discloses recent covert alcohol use not detected by standard testing in forensic psychiatric inpatients. Alcoholism, clinical and experimental research. Mar 2003;27(3):471-476.
- Skipper GE, Weinmann W, Thierauf A, et al. Ethyl glucuronide: a biomarker to identify alcohol use by health professionals recovering from substance use disorders. Alcohol Alcohol. Sep-Oct 2004;39(5):445-449.
- Kingdon JW. Agendas, alternatives, and public policies. Updated 2nd ed. Boston: Longman; 2011.
- Leape LL. Institute of Medicine medical error figures are not exaggerated. JAMA : the journal of the American Medical Association. Jul 5 2000;284(1):95-97.
- Schneidman B. The Philosophy of Rehabilitation for Impaired Physicians. The Federal Bulletin: The Journal of Medical Licensure and Discipline. 1995;82(3):125-127.
- Jansen M, Bell LB, Sucher MA, Stoehr JD. Detection of Alcohol Use in Monitored Aftercare Programs: A National Survey of State Physician Health Programs. Journal of Medical Licensure and Discipline. 2004;90(2):8-13
- Skipper G, Weinmann W, Wurst F. Ethylglucuronide (EtG): A New Marker to Detect Alcohol Use in Recovering Physicians. Journal of Medical Licensure and Discipline. 2004;90(2):14-17.
- McGarity TO, Wagner WE. Bending Science: How Special Interests Corrupt Public Health Research. Cambridge, MA: Harvard University Press; 2008.
- US Department of Health and Human Services. Mandatory guidelines and proposed revisions to mandatory guidelines for federal workplace drug testing programs: notices. Federal Register. April 13, 2004;69(71):19659-19660.
- Wood B. State of North Carolina Performance Audit North Carolina Physicians Health Program. . http://www.ncauditor.net/EPSWeb/Reports/Performance/PER-2013-8141.pdf. Accessed March 17, 2015.
- U.S. District Court Eastern District of Michigan, Case No: 2:15-cv-10337-AJT-RSW (2015). Carole Lucas, R.N., Tara Vialpandno, R.N., Scott Sanders, R.N., Kelly Schultz, P.A., and all other similarly situated health professionals v. Michigan Department of Licensing and Regulatory Affairs, Carole Engel, J.D.Former Director of Michigan Bureau of Health Professions, Ulliance, Inc. (State Contractor), Carolyn Batchelor (HPRP Contract Administrator), Stephen Batchelor (HPRP Contract Administrator), and Nikki Jones, LMSW. Filed January 30, 2015.
- Boyd JW, Knight JR. Ethical and managerial considerations regarding state physician health programs. Journal of addiction medicine. Dec 2012;6(4):243-246.



 Psychopathy is present in all professions. In The Wisdom of Psychopaths: What Saints, Spies, and Serial Killers Can Teach Us About Success, Kevin Dutton provides a side-by-side list of professions with the highest (CEO tops the list) and lowest (care-aid) percentage of psychopaths. Interestingly surgeons come in at #5 among the professions with the highest percentage of psychopathy while doctors (in general) are listed among the lowest.
Psychopathy is present in all professions. In The Wisdom of Psychopaths: What Saints, Spies, and Serial Killers Can Teach Us About Success, Kevin Dutton provides a side-by-side list of professions with the highest (CEO tops the list) and lowest (care-aid) percentage of psychopaths. Interestingly surgeons come in at #5 among the professions with the highest percentage of psychopathy while doctors (in general) are listed among the lowest.






















 Circa 1995
Circa 1995