 Educational and Professional Standards in Medical Specialties and Subspecialties
Educational and Professional Standards in Medical Specialties and Subspecialties
The increasingly rapid growth and complexity of medical knowledge in twentieth century American medicine resulted in the creation of specialties and subspecialties.
A related development was the creation of “boards” to “certify” physicians as knowledgeable and competent in the specialties and subspecialties in which they claimed to have expertise. The American Board of Ophthalmology, organized in 1917, was the first of these.
As the number of medical specialties proliferated an umbrella organization was formed to accomplish this task. The Advisory Board for Medical Specialties was created in 1933 and reorganized as the American Board of Medical Specialties (ABMS) in 1970. This non-profit organization oversees board certification of all physician specialists and sub-specialists in the United States.
The ABMS recognizes 24 medical specialties in which physicians can pursue additional training and education to pursue Board Certification.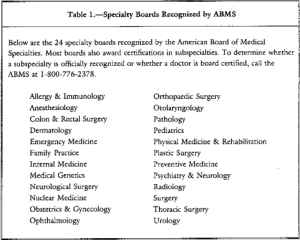
In 1991 the American Board of Medical Genetics was approved as the 24th ABMS board and these 24 boards grant the 37 general certificates and 88 subspecialty certificates available to medical specialists today.
The ABMS Member Boards are responsible for developing and implementing the educational and professional standards for quality practice in a particular medical specialty or subspecialty and evaluate physician candidates for Board Certification. They set the bar of knowledge and competence for their given area of expertise.
All of the ABMS Member Boards are:
“committed to the principle of examining doctors based on six general competencies designed to encompass quality care: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice.”These areas have been collectively identified by the ABMS, the American College of Graduate Medical Education (ACGME) and the Institute of Medicine (IOM) in order to standardize graduate medical education in any specialty from medical school graduation through retirement.1
One of the 24 medical specialties ABMS recognizes in which physicians can pursue additional training and education and pursue Board Certification is Psychiatry.
Founded in 1934, The American Board of Psychiatry and Neurology (ABPN) is one of the 24 ABMS specialty boards. In 1959, the ABPN issued its first subspecialty certificate in Child and Adolescent Psychiatry and was the only ABNP subspecialty until 1991 when the first examination in Geriatric Psychiatry was administered.4 Addiction Psychiatry became a subspecialty of ABPN in 1993.
The ABPN governs the specialty of Psychiatry, of which Addiction Psychiatry is a subspecialty. Board Certification in Addiction Psychiatry requires a four-year psychiatric-residency program for training in the prevention, diagnosis and treatment of mood, anxiety, substance-abuse as well as other psychological and interpersonal problems followed by an additional year of training in one of the 40 accredited Addiction Psychiatry Fellowship programs. The Accreditation Council for Graduate Medical Education (ACGME) is the professional organization responsible for the accreditation residency education programs in the US for ABMS specialty and subspecialty areas of medicine. Addiction Psychiatry training programs are governed by the ACGME and graduates are eligible for ABPN Certification in Addiction Psychiatry.
When this rigorous education and training is complete a candidate is Board Eligible and can then take the subspecialty certification exam. The exam assesses competency in the dand consultation, pharmacotherapy, pharmacology of drugs, psychosocial treatment and behavioral basis of practice to be Board Certified in the subspecialty of Addiction Psychiatry by the ABPN.
Candidates must then be assessed in a number of areas including psychiatric evaluation and consultation, pharmacotherapy, pharmacology, toxicology, psychosocial treatment, behavioral basis of practice, and many other areas in which for the past half-decade they where taught and apprenticed.
The current structure of residency training is little changed from when it was conceived originally by William Stewart Halsted in the late 19th Century. Physicians acquire knowledge and skills necessary to safely and competently manage patients through apprenticeship. Training in a specialty area provides a comprehensive platform that allows medical school graduates to apply a body of knowledge to patient care and the treatment of disease. This forms the foundation of our Guild–undifferentiated and general but pluripotential.
The American Academy of Addiction Psychiatry (AAAP) is the only professional organization in the US focused on the subspecialty of Addiction Psychiatry. The AAAP Mission Statements are to: 2
-
PROMOTE HIGH QUALITY EVIDENCE-BASED SCREENING, ASSESSMENT AND TREATMENT FOR SUBSTANCE USE AND CO-OCCURRING MENTAL DISORDERS.
-
TRANSLATE AND DISSEMINATE EVIDENCE-BASED RESEARCH TO CLINICAL PRACTICE AND PUBLIC POLICY.
-
STRENGTHEN ADDICTION PSYCHIATRY SPECIALTY TRAINING AND FOSTER CAREERS IN ADDICTION PSYCHIATRY.
-
PROVIDE EVIDENCE-BASED ADDICTION EDUCATION TO HEALTH CARE TRAINEES AND HEALTH PROFESSIONALS TO ENHANCE PATIENT CARE AND PROMOTE RECOVERY.
-
EDUCATE THE PUBLIC AND INFLUENCE PUBLIC POLICY FOR THE SAFE AND HUMANE TREATMENT OF THOSE WITH SUBSTANCE USE DISORDERS.
-
PROMOTE PREVENTION AND ENHANCE ADDICTION TREATMENT AND RECOVERY ACROSS THE LIFE SPAN.
-
PROMOTE RESEARCH ON THE ETIOLOGY, PREVENTION, IDENTIFICATION AND TREATMENT OF SUBSTANCE USE AND RELATED DISORDERS.
Self-Designated Practice Specialty : An AMA Census Term Indicating What a Group of Doctors are Calling Themselves.
 The American Medical Association records a physician’s Self-Designated Practice Specialty (SDPS) in response to an annual credentialing survey. According to the AMA, SDPS are “historically related to the record-keeping needs of the American Medical Association and do not imply ‘recognition’ or ‘endorsement’ of any field of medical practice by the Association. SDPS refers to a self-designated specialty and this is not equivalent nor does it imply ABMS [American Board of Medical Specialties] Board Certification.
The American Medical Association records a physician’s Self-Designated Practice Specialty (SDPS) in response to an annual credentialing survey. According to the AMA, SDPS are “historically related to the record-keeping needs of the American Medical Association and do not imply ‘recognition’ or ‘endorsement’ of any field of medical practice by the Association. SDPS refers to a self-designated specialty and this is not equivalent nor does it imply ABMS [American Board of Medical Specialties] Board Certification.
“The fact that a physician chooses to designate a given specialty/area of practice on our records does not necessarily mean that the physician has been trained or has special competence to practice the SDPS.”3
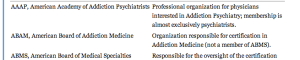
Physicians have been able to list addiction medicine as a self-designated area of practice using the specialty code “ADM” since 1990.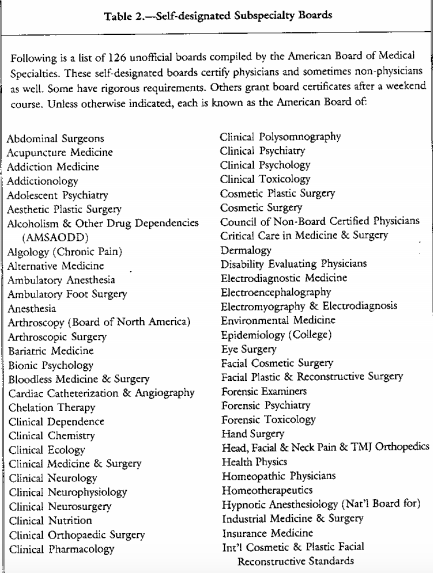
In contrast to these accepted board credentials, American Board of Addiction Medicine (ABAM) certification requires only a medical degree, a valid license to practice medicine, completion of a residency training in ANY specialty, and one year‘s full time involvement plus 50 additional hours of medical education in the field of alcoholism and other drug dependencies. The majority of American Society of Addiction Medicine (ASAM) physicians meet these requirements by “working in a chemical dependency treatment facility, taking continuing medical education courses in addiction, or participating in research.”6
The American Society of Addiction Medicine’s mission is to “establish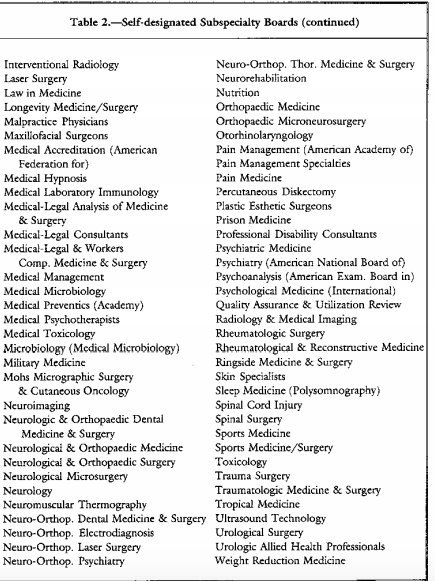 addiction medicine as a specialty recognized by professional organizations, governments,, physicians, purchasers, and consumers of health care products, and the general public.’5 They have succeeded in doing this as many consider them to be the experts in addiction medicine including regulatory agencies.
addiction medicine as a specialty recognized by professional organizations, governments,, physicians, purchasers, and consumers of health care products, and the general public.’5 They have succeeded in doing this as many consider them to be the experts in addiction medicine including regulatory agencies.
The goal of the American Board of Addiction Medicine (ABAM) Foundation is to “gain recognition of Addiction Medicine as a medical specialty by the American Board of Medical Specialties (ABMS).”
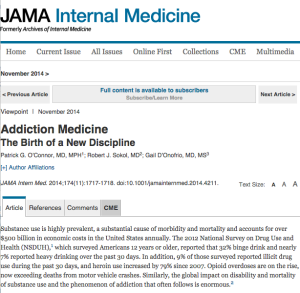
But Addiction Medicine is currently not recognized by the ABMS. It is still a a Self-Designated Practice Specialty and the ABAM is a Self-Designated Board. So too is the American Academy of Ringside Medicine and Surgery, the American Academy of Bloodless Medicine and Surgery and the Council of Non-Board Certified Physicians. But these Self-Designated Boards do not have the multi-billion dollar drug and alcohol testing and treatment industry supporting them. Addiction Medicine has deep pockets, and if the November 2014 issue of the Journal of the American Medical Association (JAMA) is a harbinger of what’s to come, this self-designated practice specialty currently being certified by a self-designated Board and bereft of anything resembling the the educational and professional standards for quality practice in a particular medical specialty or subspecialty may soon robber baron its way into acceptance by the American Board of Medical Specialties.
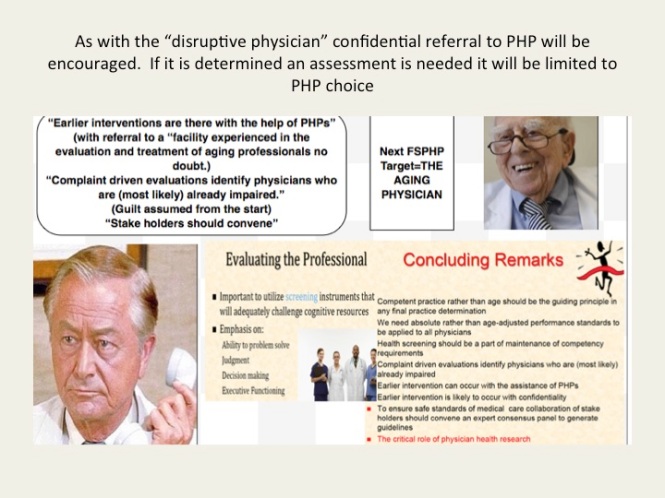
One thing is for certain. When society gives power of diagnosis and treatment to individuals within a group schooled in just one uncompromising model of addiction with the majority attributing their very own sobriety to that model, they will exercise that power to diagnose and treat anyone and everyone according to that model. The birth of Addiction Medicine as an ABMS accepted discipline is sure to be a success for the drug and alcohol testing and 12-step treatment industry, but its spawn is sure to be an inauspicious mark on the Profession and Guild of Medicine and a bane of society for years to come.
- Stevens RA. In: Stevens R, Rosenberg C, Burns L, eds. History and Health Policy in the United States: Putting the Past Back in: Rutgers University Press; 2006:49-83.
- American Association of Addiction Psychiatry Website http://www.aaap.org/about-aaap/mission-statement (accessed 4/2/2014).
- American Medical Association. List & Definitions of Self-Designated Practice Specialties. August 21, 2012 http://www.ama-assn.org/ama.
- Juul D, Scheiber SC, Kramer TA. Subspecialty certification by the American Board of Psychiatry and Neurology. Academic psychiatry : the journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry. Spring 2004;28(1):12-17.
- http://www.asam.org/about-us/mission-and-goals.
- Tontchev GV, Housel TR, Callahan JF, Kunz KB, Miller MM, Blondell RD. Specialized training on addictions for physicians in the United States. Substance abuse : official publication of the Association for Medical Education and Research in Substance Abuse. Apr 2011;32(2):84-92.



















 “Spirituality can go hand-in-hand with ruthless single-mindedness when the individual is convinced his cause is just”
“Spirituality can go hand-in-hand with ruthless single-mindedness when the individual is convinced his cause is just”











 In addition to an up to date medication list we decided to put in the bare but essential elements of the medical record that would be needed in an emergency; these consisted of demographics, emergency contacts, a basic problem list, allergies and a baseline EKG.
In addition to an up to date medication list we decided to put in the bare but essential elements of the medical record that would be needed in an emergency; these consisted of demographics, emergency contacts, a basic problem list, allergies and a baseline EKG. They don’t see the problem and they don’t see a need for a solution. Many believe it is the patient’s responsibility to keep track of their medications and that any problem associated with not providing their medication list up to date were self-inflicted.” He said it will be a different story in five or ten years when the problem is acknowledged and accepted by the rank and file.
They don’t see the problem and they don’t see a need for a solution. Many believe it is the patient’s responsibility to keep track of their medications and that any problem associated with not providing their medication list up to date were self-inflicted.” He said it will be a different story in five or ten years when the problem is acknowledged and accepted by the rank and file.

